Abstract
Background
The disruption of dual antiplatelet therapy (DAPT) due to non-compliance or bleeding is known to significantly increase the risk of adverse outcomes after percutaneous coronary intervention (PCI). However, it is currently unknown if there are differences in the predictors and clinical impact of disruption due to non-compliance compared with bleeding.
Methods
The patterns of non-adherence to antiplatelet regimens in stented patients (PARIS) registry was an international, multicenter prospective study of PCI patients discharged on DAPT (aspirin + a P2Y12 receptor). We analyzed the incidence, patient characteristics, predictors, and outcomes in patients with DAPT disruption due to non-compliance as compared to DAPT disruption due to bleeding in the PARIS registry. Predictors of non-recommended disruption and bleeding disruption were assessed using logistic regression. Risks associated with disruption on major adverse cardiac events (MACE, a composite of cardiac death, definite or probable stent thrombosis, spontaneous myocardial infarction, and target lesion revascularization) were analyzed using time-updated Cox regression over 2-year follow-up.
Results
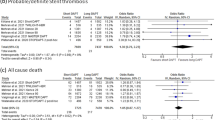
Out of 5018 patients, the rate of non-compliant DAPT disruption was 1.6% at 30 days (n = 79), 6.5% at 12 months (n = 328), and 9.1% at 2 years from PCI (n = 457). The rate of bleeding DAPT disruption was 0.6% at 30 days (n = 32), 3.1% at 12 months (n = 156), and 4.6% at 2 years (n = 229). Multivariate predictors of non-compliant disruption included female gender, history of smoking, acute coronary syndrome, and US patients which were associated with greater risk; and dyslipidemia and discharge PPI which were associated with lower risk. Multivariate predictors of bleeding disruption included older age, prior MI, and discharge warfarin which were associated with greater risk; and US region and intervention to the LAD which were associated with lower risk. Non-compliant disruption was associated with a significantly greater risk for MACE (HR 1.73, 95% CI 1.17–2.54, p = 0.006) and spontaneous myocardial infarction (HR 2.93, 95% CI 1.85–4.65, p < 0.001). Bleeding disruption was associated with a significantly greater risk for all-cause death (HR 1.93, 95% CI 1.22–3.08, p = 0.005).
Conclusion
Approximately 1 in 10 patients disrupts DAPT due to non-compliance and 1 in 20 disrupts DAPT due to bleeding. Disruption due to non-compliance resulted in higher risk for ischemic events and disruption due to bleeding had higher subsequent mortality. These data warrant efforts to focus on patient education in those at high risk of non-compliance.



Similar content being viewed by others
References
Brown MT, Bussell JK (2011) Medication adherence: WHO cares? Mayo Clin Proc 86:304–314
De Geest S, Sabate E (2003) Adherence to long-term therapies: evidence for action. Eur J Cardiovasc Nurs 2:323
Lee JK, Grace KA, Taylor AJ (2006) Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA 296:2563–2571
Osterberg L, Blaschke T (2005) Adherence to medication. N Engl J Med 353:487–497
Tarn DM, Heritage J, Paterniti DA, Hays RD, Kravitz RL, Wenger NS (2006) Physician communication when prescribing new medications. Arch Intern Med 166:1855–1862
Duerschmied D, Brachmann J, Darius H, Frey N, Katus HA, Rottbauer W, Schäfer A, Thiele H, Bode C, Zeymer U (2018) Antithrombotic therapy in patients with non-valvular atrial fibrillation undergoing percutaneous coronary intervention: should we change our practice after the PIONEER AF-PCI and RE-DUAL PCI trials? Clin Res Cardiol 107(7):533–538. https://doi.org/10.1007/s00392-018-1242-2 PMID: 29679144
Lee SY, Hong MK, Shin DH, Kim JS, Kim BK, Ko YG, Choi D, Jang Y, Kim HS, Valgimigli M, Palmerini T, Stone GW (2017) Clinical outcomes of dual antiplatelet therapy after implantation of drug-eluting stents in patients with different cardiovascular risk factors. Clin Res Cardiol 106(3):165–173. https://doi.org/10.1007/s00392-016-1035-4 PMID: 27631821
Airoldi F, Colombo A, Morici N et al (2007) Incidence and predictors of drug-eluting stent thrombosis during and after discontinuation of thienopyridine treatment. Circulation 116:745–754
Giustino G, Baber U, Sartori S et al (2015) Duration of dual antiplatelet therapy after drug-eluting stent implantation: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Cardiol 65:1298–1310
Mehran R, Baber U, Steg PG et al (2013) Cessation of dual antiplatelet treatment and cardiac events after percutaneous coronary intervention (PARIS): 2 year results from a prospective observational study. Lancet 382:1714–1722
Cutlip DE, Windecker S, Mehran R et al (2007) Clinical end points in coronary stent trials—a case for standardized definitions. Circulation 115:2344–2351
Thygesen K, Alpert JS, White HD et al (2007) Universal definition of myocardial infarction. Eur Heart J 28:2525–2538
Mehran R, Rao SV, Bhatt DL et al (2011) Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the bleeding academic research consortium. Circulation 123:2736–2144
Stone GW, McLaurin BT, Cox DA et al (2006) Bivalirudin for patients with acute coronary syndromes. New Engl J Med 355:2203–2216
Biondi-Zoccai G, Frati G, Abbate A (2015) Noncompliance and cessation of dual antiplatelet therapy after coronary stenting looking at the speck rather than noticing the log? Jacc-Cardiovasc Inte 8:411–413
Mauri L, Kereiakes DJ, Yeh RW et al (2014) Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. New Engl J Med 371:2155–2166
McFadden EP, Stabile E, Regar E et al (2004) Late thrombosis in drug-eluting coronary stents after discontinuation of antiplatelet therapy. Lancet 364:1519–1521
Dauerman H, Stoler R, Kereiakes D, Mauri L, Cutlip D, Grp ES (2013) Thrombosis, bleeding and DAPT non-adherence in the EDUCATE registry. Eur Heart J 34:877–877
Grines CL, Bonow RO, Casey DE et al (2007) Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents. J Am Coll Cardiol 49:734–739
Yu AP, Yu YF, Nichol MB, Gwadry-Sridhar F (2008) Delay in filling the initial prescription for a statin: a potential early indicator of medication nonpersistence. Clin Ther 30:761–774
Prochaska JH, Göbel S, Nagler M, Knöpfler T, Eggebrecht L, Lamparter H, Panova-Noeva M, Keller K, Coldewey M, Bickel C, Lauterbach M, Hardt R, Espinola-Klein C, Ten Cate H, Rostock T, Münzel T, Wild PS (2018) Sustained atrial fibrillation increases the risk of anticoagulation-related bleeding in heart failure. Clin Res Cardiol. https://doi.org/10.1007/s00392-018-1293-4 (PMID: 29948286; epub ahead of print)
Richardt G, Maillard L, Nazzaro MS, Abdel-Wahab M, Carrié D, Iñiguez A, Garot P, Abdellaoui M, Morice MC, Foley D, Copt S, Stoll HP, Urban P (2018) Polymer-free drug-coated coronary stents in diabetic patients at high bleeding risk: a pre-specified sub-study of the LEADERS FREE trial. Clin Res Cardiol. https://doi.org/10.1007/s00392-018-1308-1 (PMID:29951803; epub ahead of print)
Benner JS, Chapman RH, Petrilla AA, Tang SSK, Rosenberg N, Schwartz JS (2009) Association between prescription burden and medication adherence in patients initiating antihypertensive and lipid-lowering therapy. Am J Health-Syst Ph 66:1471–1477
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moalem, K., Baber, U., Chandrasekhar, J. et al. Incidence, predictors, and outcomes of DAPT disruption due to non-compliance vs. bleeding after PCI: insights from the PARIS Registry. Clin Res Cardiol 108, 643–650 (2019). https://doi.org/10.1007/s00392-018-1392-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1392-2