Abstract
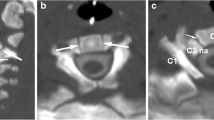
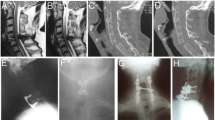
Upper cervical synchondrosis fractures are the most common types of cervical fractures in the pediatric population less than 7 years of age (Blauth et al (Eur Spine J 5:63-70, 1996); Connolly et al (Pediatr Radiol 25(Suppl1):S129-133, 1995); Mandabach et al (Pediatr Neurosurg 19(5):225-232, 1993); Schippers et al (Acta Neurochir 138:524-530, 1990)) The vast majority occur through the dentocentral or basilar synchondrosis. We present the second reported case in recent literature of a unilateral neurosynchondrosis fracture. The patient, a 4-year-old male, was initially managed conservatively with a rigid cervical collar for a period of 3 months. Despite multiple counseling sessions with family, the patient remained poorly compliant with cervical immobilization. After 3 months, imaging demonstrated partial fusion with persistent anterolisthesis of C2 on C3. The decision was made to place the child in external halo fixation as an attempt to achieve fusion prior to committing to internal surgical fixation and the associated sequelae. Immobilization with a hard cervical collar is often first line treatment. In the case of failed fusion, debate exists regarding surgical fixation in children. Occipito-atlanto-axial fusion leads to permanent loss of a significant degree of flexion, extension, and rotatory movement. The pediatric population has a strong propensity to fuse; however, compliance is often a barrier to conservative treatment due to age-related behavioral practices. We demonstrate that even with initial failed fusion and progression of deformity while in a cervical collar, conservative management with external halo fixation can potentially obviate the need for internal fixation.




Similar content being viewed by others
References
Akbarnia BA, Yazici M, Thompson GH (2011) The growing spine: management of spinal disorders in young children. Springer, Heidelberg
Blauth M, Shmidt U, Otte D, et al. (1996) Fractures of the odontoid process in small children: biomechanical analysis and report of three cases. Eur Spine J 5:63–70
Botte M, Byrne T, Abrams R, Garfin S (1996) Halo skeletal fixation: techniques of application and prevention of complications. J Am Acad Orthop Surg 4:44–53
Brown RL, Brunn MA, Garcia VF (2001) Cervical spine injuries in children: a review of 103 patients treated consecutively at a level 1 pediatric trauma center. J Pediatr Surg 36:1107–1114
Cattell HS, Filtzer DL (1965) Pseudosubluxation and other normal variations in the cervical spine in children. A study of one hundred and sixty children. J Bone Joint Surg Am 47:1295–1309
Connolly B, Emery D, Armstrong D (1995) The odontoid synchondrotic slip: an injury unique to young children. Pediatr Radiol 25(Suppl1):S129–S133
Dormans JP, Criscitiello AA, Drummond DS, Davidson RS (1995) Complications in children managed with immobilization in a halo vest. J Bone Joint Surg Am 77:1370–1373
Englander O (1942) Nontraumatic occipito-atlanto-axial dislocation: a contribution to the radiology of the atlas. Br J Radiol 15:341–345
Fassett D, McCall T, Brockmeyer D (2006) Odontoid synchondrosis fractures in children. Neurosurg Focus 20(2):E7
Fesmire F, Luten R (1989) The pediatric cervical spine: developmental anatomy and clinical aspects. J Emerg Med 7:133–142
Fulkerson DH, Hwang SW, Patel AJ, Jea A (2012) Open reduction and internal fixation for angulated, unstable odontoid synchondrosis fractures in children: a safe alternative to halo fixation? J Neurosurg Pediatr 9:35–41
Hadley MN (2002) Management of pediatric cervical spine and spinal cord injuries. Neurosurgery 50:S85–S99
Hosalkar HS, Greenbaum JN, Flynn JM, Cameron DB, Dormans JP, Drummond DS (2009) Fractures of the odontoid in children with an open basilar synchondrosis. J Bone Joint Surg (Br) 91(6):789–796
Karwacki GM, Schneider JF (2012a) Normal ossification patterns of atlas and axis: a CT study. Am J Neuroradiol 33(10):1882–1887
Leonard JR, Jaffe DM, Kuppermann N, Olsen CS, Leonard JC, Group PECARNPCSS (2014) Cervical spine injury patterns in children. Pediatrics 133:e1179–e1188
Lidar Z, Constantini S, Regev G, Salame K (2012) Absorbable anterior cervical plate for corpectomy and fusion in a 2-year-old child with neurofibromatosis: technical note. J Neurosurg Pediatr 9:442–446
Kalfas I, Wilberger J, Goldberg A, et al. (1988) Magnetic resonance imaging in acute spinal cord trauma. Neurosurgery 23:295–299
Karwacki GM, Schneider JF (2012b) Normal ossification patterns of atlas and axis: a CT study. AJNR Am J Neuroradiol 33:1882–1887
Knox J, Schneider J, Wimberly RL, Riccio AI (2014a) Characteristics of spinal injuries secondary to nonaccidental trauma. J Pediatr Orthop 34:376–381
Knox JB, Schneider JE, Cage JM, Wimberly RL, Riccio AI (2014b) Spine trauma in very young children: a retrospective study of 206 patients presenting to a level 1 pediatric trauma center. J Pediatr Orthop 34:698–702
Mandabach M, Ruge JR, Hahn YS, et al. (1993) Pediatric axis fractures: early halo immobilization, managment and outcome. Pediatr Neurosurg 19(5):225–232
Pang D, Sun PP (2004) Pediatric vertebral column and spinal cord injuries. In: Winn HR (ed) Neurological surgery. WB Saunders, Philadelphia, pp. 3515–3557
Polk-Williams A, Carr BG, Blinman TA, Masiakos PT, Wiebe DJ, Nance ML (2008) Cervical spine injury in young children: a National Trauma Data Bank review. J Pediatr Surg 43(9):1718–1721
Shacked I, Ram Z, Hadani M (1993) The anterior cervical approach for traumatic injuries to the cervical spine in children. Clin Orthop Relat Res 292:144–150
Sherk HH, Nicholson JT, Chung SM (1978) Fractures of the odontoid process in young children. J Bone Joint Surg Am 60:921–924
Schippers N, Konings P, Hassler W, et al. (1990) Typical and atypical fractures of the odontoid process in young children. Report of two cases and a review of the literature. Acta Neurochir 138:524–530
Shaw M, Burnett H, Wilson A, et al. (1999) Pseudosubluxation of C2 on C3 in polytraumatized children—prevalence and significance. Clin Radiol 54:377–380
Tokunaga S, Ishii Y, Aizawa T, et al. (2011) Remodeling capacity of malunited odontoid process fractures in kyphotic angulation in infancy: an observation up to maturity in three patients. Spine 1;36(23):E1515–1518
Wang JC, Nuccion SL, Feighan JE, et al. (2001) Growth and development of the pediatric cervical spine documented radiographically. J Bone Joint Surg Am 83A:1212–1218
Ware ML, Gupta N, Sun PP, et al. (2006) Clinical biomechanics of the pediatric craniocervical junction and the subaxial spine. In: Brockmeyer DL (ed) Advanced pediatric craniocervical surgery. Thieme, New York, pp. 27–42
Wong ST, Zovickian J, Hou Y, et al. (2014) Traumatic rupture of the neurocentral synchondrosis of the axis in a child. J Neurosurg Pediatr 23(5):548–552
Compliance with ethical standards
Informed consent was not required for this case report. Reporting and research was performed within compliance of ethical standards.
Conflict of Interest
The authors included below have no conflict of interest to report and are not participating in any human or animal research related to this procedure.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shammassian, B., Wright, C.H., Wright, J. et al. Successful delayed non-operative management of C2 neurosynchondrosis fractures in a pediatric patient: a case report and review of management strategies and considerations for treatment. Childs Nerv Syst 32, 163–168 (2016). https://doi.org/10.1007/s00381-015-2821-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2821-4