Abstract
To assess the relationship between ankle-brachial index (ABI) and up to 10-year mortality in older individuals below and above the age of 80 years. In a multicenter survey of health status in the community dwelling subjects aged 55–59 and 65 + years in Poland, we assessed baseline medical history including risk-factors. We measured ABI, and serum creatinine, cholesterol, NT-proBNP, and interleukin-6 (IL-6) concentrations. We assessed mortality based on public registry. Between 2009 and 2019, 27.3% of 561 participants < 80 years, and 79.4% of 291 participants ≥ 80 years, died (p < 0.001); 67.8, 41.5, and 40.3% in the ABI groups < 0.9, 0.9–1.4, and > 1.4, respectively (p < 0.01). In the unadjusted Cox models, ABI was associated with mortality in the entire group, and < 80 years. In the entire group, analysis adjusted for age and sex showed mortality risk increased by 11% per year, and 50% with male sex. Mortality decreased by 37% per 1 unit ABI increase. In the group of people ≥ 80 years, only age was significantly associated with mortality (p < 0.001). In stepwise regression ABI < 0.9, male sex, active smoking, and NT-proBNP level were associated with risk of death < 80 years. In the ≥ 80 years old, mortality risk was associated with older age, and higher levels of IL-6, but not ABI. The ABI < 0.9 is associated with higher mortality in older people, but not among the oldest-old. In the oldest age group, age is the strongest predictor of death. In this age group, inflammageing is of importance.
Similar content being viewed by others
Introduction
Background
Ankle-brachial index (ABI) 0.9 has been used to diagnose peripheral arterial disease (PAD), even at the pre-clinical stage [1]. Low ABI is associated with atherosclerosis of coronary and carotid arteries [2,3,4,5,6], and increased all-cause and cardiovascular mortality [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19]. ABI of more than 1.4, an index of arterial stiffness, has also been associated with adverse outcome, especially in older subjects [8, 20, 21]. Age is a potent modifier of risk, and passing the age of 80 years is considered to be a threshold beyond which relation between risk-factors and outcome may change. Few studies, yielding inconclusive results addressed the issue of ABI in relation to hard outcome in the very old persons [22, 23].
The aim of this study was to assess the relationship between baseline ABI, in the context of other cardiovascular risk factors, and the mortality of participants of the PolSenior survey in older individuals below and above the age of 80 years.
Methods
Study population
The PolSenior study was a nationwide, multicentre, cross-sectional survey of health status and its determinants in the community dwelling subjects aged 55–59 and 65 and more years [24]. Research participants were randomly recruited from among the population of Poland, in a stratified, proportional draw performed in three stages. In the first stage, the municipalities were selected according to the population, in the second the street addresses, and in the case of rural communities the villages, and in the third stage, based on the Ministry of Internal Affairs and Administration personal identification data the individuals in bundles were selected [24]. Between January 2009 and April 2010, we enrolled 5695 participants. In 1018 (17.8%), medical examination was performed by geriatricians. In the current report, we present the data from 852 participants in whom we obtained the data on ABI on the right lower limb, and for whom vital status was available as of 20th April 2019.
Data collection
Sociodemographic data, information about habits, and past medical history were obtained using a structured questionnaire administered by trained nurses during home visits. As part of the geriatric assessment, basic activities of daily living (ADL) and the Tinetti gait and balance test were performed, with higher values associated with better preservation of function [25, 26].
Medical examination by the geriatrician included ABI measurement according to the guidelines. Blood pressure was measured on both arms with an A&D, UA 787 Plus automatic device, in supine position, after 5-min rest. In case of between-arm difference of blood pressure, higher values were used for subsequent analyses.
The systolic blood pressure (SBP) on both posterior tibial arteries was assessed using Doppler Bidop ES-100VX device with 8 MHz ultrasound probe (Hadeco, Inc, Kawasaki, Japan). Blood pressure cuff was positioned on a calf with the distal edge of the cuff 3 cm above the medial malleolus. The SBP measurement was performed on both lower extremities. ABI was calculated as: systolic blood pressure on posterior tibial artery (mm Hg)/systolic blood pressure on brachial artery (mm Hg) [27]. There were five missing values for the left lower extremity, and the average difference between right and left lower extremity values was not statistically significant (p = 0.27). Accordingly, we decided to use the values from right lower extremity in all subsequent analyses.
For the stratified analyses, we categorized ABI into normal: 0.9–1.4, low: < 0.9, and high: > 1.4. Body mass index (BMI) was calculated according to the formula: body weight (kg)/height (m2). Creatinine and cholesterol levels were measured by the standard method with an automated analyzer Modular PPE (Roche Diagnostics) and Roche Diagnostics GmbH reagents (Mannheim Germany), and the LDL cholesterol was measured directly with enzymatic-colorimetric method.
A serum aminoterminal pro-brain natriuretic peptide (NT-proBNP) level was measured by an electrochemiluminescence immunoassay (ECLIA) method (Roche Diagnostics GmbH, Mannheim, Germany) with a immunoassay analyzer Cobas e411 (Roche Diagnostics GmbH, Mannheim, Germany).
Plasma interleukin 6 (IL-6) concentration was determined by high-sensitivity ELISA using R&D Systems kits (Minneapolis, MN, USA).
Mortality was assessed 10 years after beginning of the study. Data on deaths were obtained from the personal id number (PESEL) register, after obtaining the consent of the Ministry of Digitization. The study was approved by the Bioethics Committee of the Medical University of Silesia in Katowice (KNW-6501–38/I//08). Each participant gave written, informed consent to take part in the study.
Statistical analysis
The database management and the statistical analyses were performed with SAS 9.4 (SAS Institute Inc., Cary, NC, USA). Continuous variables were presented as means with standard deviations, and compared with the standard normal Z-test, in case of normal distribution, and as medians with interquartile ranges and compared with Wilcoxon’s test. The proportions were compared with Chi square test. To demonstrate the influence of ABI at baseline on 10-year mortality, we first plotted the Kaplan-Maier curves, for the entire group and in individuals under and over 80, where the ABI status was categorized into 3 subcategories (< 0.9, 0.9–1.4, > 1.4). Where applicable, the analyses were adjusted for multiple comparisons with Bonferroni method. Further, we used Cox regression to model time to event (death) as a function of baseline ABI. The models were fitted for entire group and in the subgroups under 80 and over 80 years of age. Each time we started with unadjusted model, then fitted a model with adjustment for sex and age and finally on top of ABI, sex, and age, the stepwise procedure selected significant confounders form among the following: SBP, DBP, IL-6, LDL cholesterol, NT-proBNP, creatinine, BMI, current smoking status; and the history of each of the following: myocardial infarction (MI), stroke, heart failure, diabetes mellitus, and hypertension. In the survival analyses, cases with no event and follow-up shorter than 10.4 years were right-censored.
Results
The characteristics of study population divided into groups according to the age is shown in Table 1. Low ABI was present in 118 (13.9%), normal ABI in 662 (77.7%) and high ABI in 72 (8.4%) participants, respectively.
The time between entry into the study and assessment of vital status averaged 9.4 years (range 8.4 to 10.5, years) years. During the average 9.4-year follow-up, 153 (27.3%), and 231 (79.4%) participants died in the group of < 80 years of age, and in the group ≥ 80 years (p < 0.001), respectively. In the entire age-range, the mortality was: 67.8% (80 persons) in the low ABI group, 41.5% (275 persons) in the normal ABI group and 40.3% (29 persons) in the high ABI group, respectively (p < 0.001).
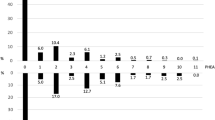
Kaplan–Meier survival analysis in the entire group revealed significantly higher mortality rate in low ABI group in comparison to people with ABI within normal range and with high ABI (Log-rank test, p < 0.001) (Fig. 1). The mortality did not differ between the two latter groups (Fig. 1).
Similar results were obtained in the subgroup of participants below 80 years of age. Mortality was significantly higher in individuals with ABI < 0.9 in comparison to persons with normal and high ABI (Log-rank test, p < 0.001). Mortality did not differ between normal range ABI and ABI > 1.4 (Fig. 1).
In the group ≥ 80 years, the mortality rate over a 9.4-year period did not differ according to the ABI status (p = 0.10) (Fig. 1).
In the unadjusted models, ABI was associated with mortality in the entire group and in subgroup < 80 years of age, but not in oldest subgroup. In the entire group, analysis adjusted for age and sex showed that mortality risk increased by 11% for each year of life, by 50% for male sex, and decreased by 37% for 1 unit greater ABI (Table 2). Similar direction of relationship was demonstrated in persons under 80 years of age, however in men, the risk of death was more than two-fold higher than in women, and 1 unit higher ABI value was associated with mortality risk lower by 62%. In similar analyses in the group ≥ 80 years, only age was significantly associated with mortality (p < 0.001). In this age group, neither sex nor ABI were associated with a risk of death (Table 2).
In the final step, after forcing sex, age, and ABI into the model, the stepwise procedure was employed to select important confouders from among the following baseline characteristics: smoking status, BMI, systolic and diastolic blood pressure, serum levels of creatinine, IL-6, LDL, and NT-proBNP, presence of hypertension, diabetes, heart failure, history of stroke and myocardial infarction. In these analyses, ABI was associated with mortality only in the subgroup aged < 80 years. ABI higher by 1 unit decreased mortality risk by 55%. In the entire group, increased risk of death was associated with older age, male sex, lower BMI, higher diastolic blood pressure, higher NT-proBNP and IL-6 concentration and active smoking (Table 2).
Low ABI value, next to age, male sex, active smoking, and increased NT-proBNP level was significantly associated with risk of death in the group aged < 80 years (Table 2).
According to the results of stepwise regression performed in the group aged ≥ 80 years, mortality risk was associated with older age, and higher levels of IL-6, but not with ABI (Table 2). These results were not materially altered when ADL (Table 2) or results of Tinetti test were added to stepwise procedure.
Discussion
We demonstrated that ABI of < 0.9 is associated with increased mortality in older persons, as opposed to both normal (0.9–1.4) and increased (> 1.4) ABI values. This was driven by the results in participants below the age of 80 years. In the octogenarian-and-older group, ABI status did not influence mortality.
We based our results on a 9.4-year follow-up for vital status, of a large subsample from a nation-wide study of health of older persons and its determinants that was carried out in Poland. We demonstrated mortality gradient from low ABI (67.8%), to normal (41.5%) and high ABI (40.3%). Previously, the estimated two to fourfold increase of risk of mortality [14] associated with low ABI was confirmed in a number of populations. These included high-risk patients diagnosed with cardiovascular (CVD) disease [18], burdened with CVD risks factors [11], symptomatic and asymptomatic PAD [9, 12, 17], and diabetes mellitus [13, 15, 18]. The risk was demonstrated in the primary care setting [10, 13], and in population-based studies [4, 5, 8, 16,17,18,19], alike. This was further confirmed in systematic reviews and meta-analyses [16, 28, 29]. Two studies published thus far assessed 10-year mortality according to ABI status. Mueller et al. [15] showed three-fold higher risk of death associated with low ABI in comparison to the matched controls, but study was carried out in the symptomatic PAD group with a mean age of 64 years, which may correspond to our younger group aged < 80 years. Sartipy et al. [17] obtained similar results in a population-based observational study of 4940 subjects with a mean age of 71 years. They showed that the 10-year all-cause mortality was 27% in the control group, 56% in the asymptomatic PAD, 63% in the intermittent claudication, and 75% in the severe limb ischaemia groups, respectively.
The incidence of low ABI increases with age reaching 23% to 60% after the age of 802 [30, 31]. Previously, we showed that in the Polish older population abnormal ABI was found in 31.8%; the value of ABI < 0.9 in 19.9%, and ABI > 1.4 in 11.9% of examined persons [32].
Few studies focused on the relationship between the ABI value and the risk of death in people over 80 years of age. Murabito et al. [22] in a 4-year follow-up of 251 men and 423 women with mean age of 80 years and Bo et al. [23] in study group of 632 nursing home residents with mean age of 82 years showed that ABI < 0.9 was not related to all-cause and cardiovascular mortality. Our results extend this evidence into over twice as long a follow-up and onto community dwelling very old subjects.
In our study, the characteristics of the groups < 80 years and ≥ 80 years, are similar, however, the older subgroup was characterized by slightly greater percentage of men, lower frequency of smoking, two times higher prevalence of heart failure and higher median NT-pro BNP level, higher frequency of stroke, higher IL-6 concentration, lower DBP and lower LDL level. No significant differences were observed between the study groups in terms of diabetes mellitus, BMI, hypertension, and myocardial infarction. We did not find relation between medical history and risk of mortality.
These results, and in particular the lack of significant effect of diabetes on mortality, contradicts the results of other studies [10, 12, 15, 18]. Our Cox models with stepwise selection of significant explanatory variables demonstrated that in the < 80 years group, in addition to low ABI, survival was shortened by older age, male sex, smoking and elevated NT-proBNP level. In the ≥ 80 years old group, only age and IL-6 levels had a significant impact on survival. These results are consistent with other studies [10, 12]. In the German Get ABI study during 3-year follow-up of persons with mean age of 72 years, in addition to ABI < 0.9, the older age, male sex, smoking, diabetes, and CVD episodes have been associated with mortality, while hyperlipidemia and hypertension were not significantly associated with the fatal outcome [10]. In turn, in the study by Mueller et al. [12] which included data from the Linz Peripheral Arterial Disease study, the factor affecting mortality was the elevated NT-proBNP concentration, and additionally, in diabetic patients, a higher hsCRP level.
The observation that in our group above the age of 80 years classic cardiovascular risk factor did not influence outcome may reflect the fact that at the advanced age other factors, such low grade inflammation, may play more important role. The higher concentration of IL-6 shown in our group of subjects ≥ 80 years of age, and its significant negative impact on survival are in line with other studies conducted in the populations of older persons [33]. Aging is associated with an increasing activation of the entire inflammatory cascade resulting in systemic low-grade inflammation. The inflammaging, is defined as 2 – fourfold increase in inflammation-related cytokines, acute phase proteins and elevated count of inflammatory cells [34]. Moreover, it is recognized that local inflammatory processes and systemic low-grade inflammation were characteristic parts of the pathology in almost all chronic, age-associated diseases. The association of chronic low grade inflammation with risk of death was demonstrated in a number of studies conducted in the population of people older than 80 years, showing the association between markers of inflammation and the cardiovascular mortality independently of common cardiovascular risk factors such as sex, hypertension, hypercholesterolemia, BMI, low physical activity [34,35,36].
In none of the analyses did we find a relationship between high ABI, a marker of medial arterial calcification and arterial stiffness, and mortality. The mortality did not differ between ABI of 0.9–1.4 and > 1.4. The results presented in the literature are contradictory. Some reports documented increased mortality in high ABI population [8, 20, 21], while others showed no relationship similar to our results [4, 16, 19, 37,38,39].
Our results need to be interpreted in the context of their possible limitations. First, our follow-up for mortality, which was based on public registry, did not include the cause of death. Likewise we did not perform assessment of non-fatal events, including cardiovascular events and hospitalisations. On the other hand, our data are based on a planned follow-up, and the subjects were drawn from a sample representative at the national level. The subsample we used was prespecified in the protocol of our survey to undergo technical examination.
In conclusion, the ABI below 0.9 is associated with higher mortality in older people, but not among the oldest-old, over 80 years of age. In the oldest age group, age and inflammation seem to be the strongest risk factors for all-cause mortality. Although, surprisingly, the ADL was not predictive of mortality in the oldest group, the Tinetti test result was. Thus, our results underpin the need for employment of the comprehensive geriatric assessment in all older patients, largely irrespective of their cardiovascular status.
Data availability
Available upon reasonable request.
Code availability
SAS Base codes.
References
Aboyans V, Ricco J, Bartelink M, Björck M, Brodmann M, Cohnert T, Collet JP, Czerny M, De Carlo M, Debus S, Espinola-Klein C, Kahan T, Kownator S, Mazzolai L, Naylor AR, Roffi M, Röther J, Sprynger M, Tendera M, Tepe G, Venermo M, Vlachopoulos C, Desormais I (2018) 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European society for vascular surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal. Eur Heart J 39:763–816
Poli L, Zanocchi M, Bo M, Fonte G, Fabris F (1993) Risk factors for atherosclerosis: ultrasound evaluation of carotid and femoral arteries in patients examined by coronary angiography. Int Angiol 12:13–20
Fiandra U, Bo M, Poli L, Casoli G, Esposito E, Fonte G, Fabris F (1996) Correlation between ankle-arm blood pressure index (AAI) and atherosclerotic vascular involvement in coronary arteries. Arch Gerontol Geriatr 22 (Suppl 1):85–94
Alzamora MT, Forés R, Pera G, Torán P, Heras A, Sorribes M, Baena-Diez JM, Urrea M, Alegre J, Viozquez M, Vela C (2013) Ankle-brachial index and the incidence of cardiovascular events in the Mediterranean low cardiovascular risk population ARTPER cohort. BMC Cardiovasc Disord 13:119
Alzamora MT, Forés R, Pera G, Baena-Díez JM, Valverde M, Torán P (2019) Low, borderline and normal ankle-brachial index as a predictor of incidents outcomes in the Mediterranean based-population ARTPER cohort after 9 years follow-up. PLoS One 14 (1):e0209163
Reinecke H, Unrath M, Freisinger E, Bunzemeier H, Meyborg M, Lüders F, Gebauer K, Roeder N, Berger K, Malyar MN (2015) Peripheral arterial disease and critical limb ischaemia: still poor outcomes and lack of guideline adherence. Eur Heart J 36:932–938
Criqui MH, Langer RD, Fronek A, Feigelson HS, Klauber MR, McCann TJ, Browner D (1992) Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med 326:381–386
Resnick HE, Lindsay RS, McDermott MM, Devereux RB, Jones KL, Fabsitz RR, Howard BV (2004) Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: the strong heart study. Circulation 109:733–739
Diehm C, Allenberg JR, Pittrow D, Mahn M, Tepohl G, Haberl RL, Darius H, Burghaus I, Trampisch HJ, German Epidemiological Trial on Ankle Brachial Index Study Group (2009) Mortality and vascular morbidity in older adults with asymptomatic versus symptomatic peripheral artery disease. Circulation 120:2053–2061
Diehm C, Lange S, Darius H, Pittrow D, von Stritzky B, Tepohl G, Haberl RL, Allenberg JR, Dasch B, Trampisch HJ (2006) Association of low ankle brachial index with high mortality in primary care. Eur Heart J 27:1743–1749
Li X, Luo Y, Xu Y, Li J, Hu D (2010) Relationship of ankle-brachial index with all-cause mortality and cardiovascular mortality after a 3-year follow-up: the China ankle-brachial index cohort study. J Hum Hypertens 24:111–116
Mueller T, Hinterreiter F, Luft C, Poelz W, Haltmayer M, Dieplinger B (2014) Mortality rates and mortality predictors in patients with symptomatic peripheral artery disease stratified according to age and diabetes. J Vasc Surg 59:1291–1299
Yokoyama H, Sone H, Honjo J, Okizaki S, Yamada D, Shudo R, Shimizu H, Moriya T, Haneda M (2014) Relationship between a low ankle brachial index and all-cause death and cardiovascular events in subjects with and without diabetes. J Atheroscler Thromb 21:574–581
Qu B, Liu Q, Li J (2015) Systematic review of association between low ankle-brachial index and all-cause cardiovascular, or non-cardiovascular mortality. Cell Biochem Biophys 73:571–575
Mueller T, Hinterreiter F, Poelz W, Haltmayer M, Dieplinger B (2016) Mortality rates at 10 years are higher in diabetic than in non-diabetic patients with chronic lower extremity peripheral arterial disease. Vasc Med 21:445–452
Ohkuma T, Ninomiya T, Tomiyama H, Kario K, Hoshide S, Kita Y, Inoguchi T, Maeda Y, Kohara K, Tabara Y, Nakamura M, Ohkubo T, Watada H, Munakata M, Ohishi M, Ito N, Nakamura M, Shoji T, Vlachopoulos C, Aboyans V, Yamashina A, collaborative group for the Japan Brachial-Ankle pulse wave VELocity individual participant data meta-analysis of prospective studies to examine the significance of the Ankle-Brachial Index (J-BAVEL-ABI) (2018) Ankle-brachial index measured by oscillometry is predictive for cardiovascular disease and premature death in the Japanese population: an individual participant data meta-analysis. Atherosclerosis 275:141–148
Sartipy F, Sigvant B, Lundin F, Wahlberg E (2018) Ten year mortality in different arterial disease stages: a population based observational study on outcome. Eur J Vasc Endovasc Surg 55:529–536
Alves-Cabratosa L, Garcia-Gil M, Comas-Cufí M, Blanch J, Ponjoan A, Martí-Lluch R, Elosua-Bayes M, Parramon D, Camós L, Ramos R (2019) Role of low ankle-brachial index in cardiovascular and mortality risk compared with major risk conditions. J Clin Med 8 (6):870
Samba H, Guerchet M, Ndamba-Bandzouzi B, Kehoua G, Mbelesso P, Desormais I, Aboyans V, Preux PM, Lacroix P (2019) Ankle brachial index (ABI) predicts 2-year mortality risk among older adults in the Republic of Congo: the EPIDEMCA-FU study. Atherosclerosis 286:121–127
Suominen V, Uurto I, Saarinen J, Venermo M, Salenius J (2010) PAD as a risk factor for mortality among patients with elevated ABI - a clinical study. Eur J Vasc Endovasc Surg 39:316–322
Gu X, Man C, Zhang H, Fan Y (2019) High ankle-brachial index and risk of cardiovascular or all-cause mortality: a meta-analysis. Atherosclerosis 282:29–36
Murabito JM, Evans JC, Larson MG, Nieto K, Levy D, Wilson PW, Framingham Study (2003) The ankle-brachial index in the elderly and risk of stroke, coronary disease, and death: the Framingham study. Arch Intern Med 163:1939–1942
Bo M, Zanocchi M, Poli L, Molaschi M (2005) The ankle-brachial index is not related to mortality in elderly subjects living in nursing homes. Angiology 56:693–697
Bledowski P, Mossakowska M, Chudek J, Grodzicki T, Milewicz A, Szybalska A, Wieczorowska-Tobis K, Wiecek A, Bartoszek A, Dabrowski A, Zdrojewski T (2011) Medical, psychological and socioeconomic aspects of aging in Poland: assumptions and objectives of the PolSenior project. Exp Gerontol 46:1003–1009
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW (1963) Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 185:914–919
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34:119–126
Aboyans V, Ricco J, Bartelink M, Björck M, Brodmann M, Cohnert T, Collet JP, Czerny M, De Carlo M, Debus S, Espinola-Klein C, Kahan T, Kownator S, Mazzolai L, Naylor AR, Roffi M, Röther J, Sprynger M, Tendera M, Tepe G, Venermo M, Vlachopoulos C, Desormais I (2018) 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European society for vascular surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries endorsed by: the European stroke organization (ESO)the task force for the diagnosis and treatment of peripheral arterial diseases of the European society of cardiology (ESC) and of the European society for vascular surgery (ESVS). Eur Heart J 39:763–816
Sigvant B, Lundin F, Wahlberg E (2016) The risk of disease progression in peripheral arterial disease is higher than expected: a meta-analysis of mortality and disease progression in peripheral arterial disease. Eur J Vasc Endovasc Surg 51:395–403
Agnelli G, Belch JJF, Baumgartner I, Giovas P, Hoffmann U (2020) Morbidity and mortality associated with atherosclerotic peripheral artery disease: a systematic review. Atherosclerosis 293:94–100
Meijer W, Grobbee D, Hunink M, Hofman A, Hoes A (2000) Determinants of peripheral arterial disease in the elderly. The Rotterdam study. Arch Intern Med 160:2934–2938
Ostchega Y, Paulose-Ram R, Dillon C, Gu Q, Hughes J (2007) Prevalence of peripheral arterial disease and risk factors in persons aged 60 and older: data from the national health and nutrition examination survey 1999–2004. J Am Geriatr Soc 55:583–589
Królczyk J, Piotrowicz K, Chudek J, Puzianowska-Kuźnicka M, Mossakowska M, Szybalska A, Grodzicki T, Skalska A, Gąsowski J (2019) Clinical examination of peripheral arterial disease and ankle-brachial index in a nationwide cohort of older subjects: practical implications. Aging Clin Exp Res 31:1443–1449
Harris TB, Ferrucci L, Tracy RP, Corti MC, Wacholder S, Ettinger WH Jr, Heimovitz H, Cohen HJ, Wallace R (1999) Associations of elevated interleukin-6 and C-reactive protein levels with mortality in the elderly. Am J Med 106:506–512
Bruunsgaard H (2006) The clinical impact of systemic low-level inflammation in elderly populations. Dan Med Bull 53:285–309
Reuben DB, Cheh AI, Harris TB, Ferrucci L, Rowe JW, Tracy RP, Seeman TE (2002) Peripheral blood markers of inflammation predict mortality and functional decline in high-functioning community-dwelling older persons. J Am Geriatr Soc 50:638–644
Roubenoff R, Parise H, Payette HA, Abad LW, D’Agostino R, Jacques PF, Wilson PWF, Dinarello ChA, Harris TB (2003) Cytokines, insulin-like growth factor 1, sarcopenia, and mortality in very old community-dwelling men and women: the Framingham heart study. Am J Med 115:429–435
Hyun S, Forbang NI, Allison MA, Denenberg JO, Criqui MH, Ix JH (2014) Ankle-brachial index, toe-brachial index, and cardiovascular mortality in persons with and without diabetes mellitus. J Vasc Surg 60:390–395
Hendriks EJE, Westerink J, de Jong PA, de Borst GJ, Nathoe HM, Mali WPThM, van der Graaf Y, van der Schouw YT, Beulens JW, SMART Study Group (2016) Association of high ankle brachial index with incident cardiovascular disease and mortality in a high-risk population. Arterioscler Thromb Vasc Biol 36:412–417
Velescu A, Clara A, Martí R, Ramos R, Perez-Fernandez S, Marcos L, Grau M, Degano IR, Marrugat J, Elosua R (2017) Abnormally high ankle-brachial index is associated with all-cause and cardiovascular mortality: the REGICOR study. Eur J Vasc Endovasc Surg 54:370–377
Funding
Project was supported by the national grant from the Polish Ministry of Science and Higher Education [grant nb PBZ-MEiN-9/2/2006].
Author information
Authors and Affiliations
Contributions
Study concept and design: JK, AS, JG. Acquisition of data: list names: MM, AS, KP. Analysis and interpretation of data: JK, JG, AS, KP, TG. Drafting of the manuscript: JK, AS, JG. Critical revision of the manuscript for important intellectual content: TG, MM, JG, AS.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
The study was approved by the Bioethics Committee of the Medical University of Silesia in Katowice (KNW-6501–38/I//08). Each participant gave written, informed consent to take part in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Królczyk, J., Skalska, A., Piotrowicz, K. et al. Disparate effects of ankle-brachial index on mortality in the ‘very old’ and ‘younger old’ populations-the PolSenior survey. Heart Vessels 37, 665–672 (2022). https://doi.org/10.1007/s00380-021-01949-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-021-01949-1