Abstract
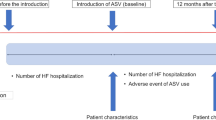
Adaptive servo-ventilation (ASV) therapy is a novel modality of noninvasive positive pressure ventilation and is now widely utilized to treat patients with chronic heart failure (CHF). However, there has been no clinical study of the effect of ASV therapy on readmission and cost-effectiveness for the treatment of CHF. The present study was conducted to evaluate the clinical efficacy and cost-effectiveness of home ASV therapy in 45 patients with a history of two or more admissions a year for worsening CHF. Seven patients refused to undergo chronic ASV therapy and three died. Thus, 35 patients were eventually enrolled in the present study. New York Heart Association class (2.8 ± 0.4 versus 2.3 ± 0.5, p < 0.001), log plasma B-type natriuretic peptide level (2.53 ± 0.44 versus 2.29 ± 0.40 pg/mL, p < 0.0001), left atrial dimension (47.5 ± 7.0 versus 44.9 ± 7.6 mm, p = 0.014), and mitral regurgitation area ratio (20.3 ± 12.1 versus 16.9 ± 8.9%, p = 0.007) decreased significantly after 12 months of ASV therapy. The frequency of hospitalization after ASV was significantly lower than before ASV (1.0 ± 1.0 versus 2.3 ± 0.5 times/year/patient, p < 0.0001). ASV also decreased the duration of hospitalization from 64.4 ± 46.5 to 22.8 ± 27.5 days/year/patient (p < 0.0001). Consequently, the total medical costs were reduced by 37% after ASV (1.95 ± 1.37 versus 3.11 ± 1.75 million yen/patient, p = 0.003). ASV therapy reduced readmissions and medical costs in patients with CHF.



Similar content being viewed by others
References
Ho KK, Pinsky JL, Kannel WB, Levy D (1993) The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol 22(Suppl A):6A–13A
Redfield MM (2002) Heart failure: an epidemic of uncertain proportions. N Engl J Med 347:1442–1444
Hamaguchi S, Kinugawa S, Goto D, Tsuchihashi-Makaya M, Yokota T, Yamada S, Yokoshiki H, Takeshita A, Tsutsui H, JCARE-CARD Investigators (2011) Predictors of long-term adverse outcomes in elderly patients over 80 years hospitalized with heart failure. A report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD)-. Circ J 75:2403–2410
Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Piña IL, Trogdon JG, American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council (2013) Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 6:606–619
Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L, Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators (2005) The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 352:1539–1549
Momomura S (2012) Treatment of Cheyne–Stokes respiration-central sleep apnea in patients with heart failure. J Cardiol 59:110–116
Haruki N, Takeuchi M, Kaku K, Yoshitani H, Kuwaki H, Tamura M, Abe H, Okazaki M, Tsutsumi A, Otsuji Y (2011) Comparison of acute and chronic impact of adaptive servo-ventilation on left chamber geometry and function in patients with chronic heart failure. Eur J Heart Fail 13:1140–1146
Harada D, Joho S, Oda Y, Hirai T, Asanoi H, Inoue H (2011) Short term effect of adaptive servo-ventilation on muscle sympathetic nerve activity in patients with heart failure. Auton Neurosci 161:95–102
Joho S, Oda Y, Ushijima R, Hirai T, Inoue H (2012) Effect of adaptive servo-ventilation on muscle sympathetic nerve activity in patients with chronic heart failure and central sleep apnea. J Card Fail 18:769–775
Yamada S, Sakakibara M, Yokota T, Kamiya K, Asakawa N, Iwano H, Yamada S, Oba K, Tsutsui H (2013) Acute hemodynamic effects of adaptive servo-ventilation in patients with heart failure. Circ J 77:1214–1220
Ushijima R, Joho S, Akabane T, Oda Y, Inoue H (2014) Differing effects of adaptive servoventilation and continuous positive airway pressure on muscle sympathetic nerve activity in patients with heart failure. Circ J 78:1387–1395
Imamura T, Kinugawa K (2017) Right ventricular end-diastolic pressure is a key to the changes in cardiac output during adaptive servo-ventilation support in patients with heart failure. Int Heart J 58:536–543
Kinoshita M, Okayama H, Kawamura G, Shigematsu T, Takahashi T, Kawada Y, Hiasa G, Yamada T, Kazatani Y (2017) Beneficial effects of rapid introduction of adaptive servo-ventilation in the emergency room in patients with acute cardiogenic pulmonary edema. J Cardiol 69:308–313
Koyama T, Watanabe H, Kobukai Y, Makabe S, Munehisa Y, Iino K, Kosaka T, Ito H (2010) Beneficial effects of adaptive servo-ventilation in patients with chronic heart failure. Circ J 74:2118–2124
Momomura S, Seino Y, Kihara Y, Adachi H, Yasumura Y, Yokoyama H (2015) Adaptive servo-ventilation therapy using an innovative ventilator for patients with chronic heart failure: a real-world, multicenter, retrospective, observational study (SAVIOR-R). Heart Vessels 30:805–817
Imamura T, Kinugawa K, Nitta D, Komuro I (2016) Long-term adaptive servo-ventilator treatment prevents cardiac death and improves clinical outcome. Int Heart J 57:47–52
Takama N, Kurabayashi M (2011) Effectiveness of adaptive servo-ventilation for treating heart failure regardless of the severity of sleep-disordered breathing. Circ J 75:1164–1169
Takama N, Kurabayashi M (2012) Effect of adaptive servo-ventilation on 1-year prognosis in heart failure patients. Circ J 76:661–667
Koyama T, Watanabe H, Igarashi G, Tamura Y, Ikeda K, Terada S, Ito H (2012) Effect of short-duration adaptive servo-ventilation therapy on cardiac function in patients with heart failure. Circ J 76:2606–2613
Koyama T, Watanabe H, Tamura Y, Oguma Y, Kosaka T, Ito H (2013) Adaptive servo-ventilation therapy improves cardiac sympathetic nerve activity in patients with heart failure. Eur J Heart Fail 15:902–909
Takama N, Kurabayashi M (2014) Safety and efficacy of adaptive servo-ventilation in patients with severe systolic heart failure. J Cardiol 63:302–307
Cowie MR, Woehrle H, Wegscheider K, Angermann C, d’Ortho MP, Erdmann E, Levy P, Simonds AK, Somers VK, Zannad F, Teschler H (2015) Adaptive servo- ventilation for central sleep apnea in systolic heart failure. N Engl J Med 373:1095–1105
Spießhöfer J, Fox H, Lehmann R, Efken C, Heinrich J, Bitter T, Körber B, Horstkotte D, Oldenburg O (2016) Heterogenous haemodynamic effects of adaptive servoventilation therapy in sleeping patients with heart failure and Cheyne-Stokes respiration compared to healthy volunteers. Heart Vessels 31:1117–1130
Hetland A, Lerum TV, Haugaa KH, Edvardsen T (2017) Patients with Cheyne-Stokes respiration and heart failure: patient tolerance after three-month discontinuation of treatment with adaptive servo-ventilation. Heart Vessels 32:909–915
Al-Khazaali A, Arora R, Helu HK (2016) Effective strategies in reducing rehospitalizations in patients with heart failure. Am J Ther 23:e799–e804
Yoshida M, Ando S, Kodama K, Ebihara K, Tanaka K, Hayashi A, Taguchi E, Kadokami T, Nakao K, Sakamoto T (2017) Adaptive servo-ventilation therapy reduces hospitalization rate in patients with severe heart failure. Int J Cardiol 238:173–176
Momomura S, Seino Y, Kihara Y, Adachi H, Yasumura Y, Yokoyama H, Wada H, Ise T, Tanaka K, SAVIOR-C investigators (2015) Adaptive servo-ventilation therapy for patients with chronic heart failure in a confirmatory, multicenter, randomized, controlled study. Circ J 79:981–990
Kihara Y, Seino Y, Momomura S, SAVIOR-C investigators (2016) Adaptive servo-ventilation for central sleep apnea in heart failure. N Engl J Med 374:687–688
Cioffi G, Tarantini L, De Feo S, Pulignano G, Del Sindaco D, Stefenelli C, Di Lenarda A, Opasich C (2005) Functional mitral regurgitation predicts 1-year mortality in elderly patients with systolic chronic heart failure. Eur J Heart Fail 7:1112–1117
Yoshida M, Kadokami T, Momii H, Hayashi A, Urashi T, Narita S, Kawamura N, Ando S (2012) Enhancement of cardiac performance by bilevel positive airway pressure ventilation in heart failure. J Card Fail 18:912–918
Gheorghiade M, Abraham WT, Albert NM, Greenberg BH, O’Connor CM, She L, Stough WG, Yancy CW, Young JB, Fonarow GC, OPTIMIZE-HF Investigators and Coordinators (2006) Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA 296:2217–2226
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hiasa, G., Okayama, H., Hosokawa, S. et al. Beneficial effects of adaptive servo-ventilation therapy on readmission and medical costs in patients with chronic heart failure. Heart Vessels 33, 859–865 (2018). https://doi.org/10.1007/s00380-018-1124-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1124-6