Abstract
Objectives
To evaluate the effect of intensified treatment parameters on safety, functional outcomes, and PSA after MR-Guided Transurethral Ultrasound Ablation (TULSA) of prostatic tissue.
Patients and methods
Baseline and 6-month follow-up data were collected for a single-center cohort of the multicenter Phase I (n = 14/30 at 3 sites) and Pivotal (n = 15/115 at 13 sites) trials of TULSA in men with localized prostate cancer. The Pivotal study used intensified treatment parameters (increased temperature and spatial extent of ablation coverage). The reporting site recruited the most patients to both trials, minimizing the influence of physician experience on this comparison of adverse events, urinary symptoms, continence, and erectile function between subgroups of both studies.
Results
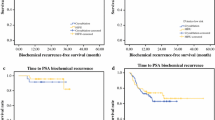
For Phase I and TACT patients, median age was 71.0 and 67.0 years, prostate volume 41.0 and 44.5 ml, and PSA 6.7 and 6.7 ng/ml, respectively. All 14 Phase I patients had low-risk prostate cancer, whereas 7 of 15 TACT patients had intermediate-risk disease. Baseline IIEF, IPSS, quality of life, and pad use were similar between groups. Pad use at 1 month and quality of life at 3 months favored Phase I patients. At 6 months, there were no significant differences in functional outcomes or adverse events.
Conclusion
TULSA demonstrated acceptable clinical safety in Phase I trial. Intensified treatment parameters in the TACT Pivotal trial increased ablation coverage from 90 to 98% of the prostate without affecting 6-month adverse events or functional outcomes. Long-term follow-up and 12-month biopsies are needed to evaluate oncological safety.

Similar content being viewed by others
Abbreviations
- CEM43:
-
Cumulative equivalent minutes at 43 °C
- IIEF:
-
International index for erectile function
- IPSS:
-
International prostate symptom score
- IQR:
-
Interquartile range
- MRI:
-
Magnetic resonance imaging
- PCa:
-
Prostate cancer
- PS:
-
Positioning system
- QoL:
-
Quality of life
- TACT:
-
TULSA-PRO Ablation Clinical Trial
- TULSA:
-
Transurethral ultrasound ablation
- UA:
-
Ultrasound applicator
References
Krebs in Deutschland 2013/2014 (2017) 11. Ausgabe. Robert Koch-Institut (Hrsg) und die Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. (Hrsg). Robert Koch-Institut, Berlin. https://doi.org/10.17886/rkipubl-2017-007. ISBN: 978-3-89606-288-8
Mottet N, Bellmunt J, Briers E, Bolla M, Bourke L, Cornford P, De Santis M, Henry A, Joniau S, Lam T, Mason MD, Van den Poel H, Van den Kwast TH, Rouvière O, Wiegel T members of the EAU–ESTRO–SUR–SIOG Prostate Cancer Guidelines Panel. EAU–ESTRO–ESUR–SIOG Guidelines on Prostate Cancer. Edn. Presented at the EAU annual congress Copenhagen 2018. ISBN:978-94-92671-02-8. EAU Guidelines Office. Place published, Arnhem, The Netherlands
Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, Davis M, Peters TJ, Turner EL, Martin RM, Oxley J, Robinson M, Staffurth J, Walsh E, Bollina P, Catto J, Doble A, Doherty A, Gillatt D, Kockelbergh R, Kynaston H, Paul A, Powell P, Prescott S, Rosario DJ, Rowe E, Neal DE, Protec TSG (2016) 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 375(15):1415–1424. https://doi.org/10.1056/NEJMoa1606220
Chin JL, Billia M, Relle J, Roethke MC, Popeneciu IV, Kuru TH, Hatiboglu G, Mueller-Wolf MB, Motsch J, Romagnoli C, Kassam Z, Harle CC, Hafron J, Nandalur KR, Chronik BA, Burtnyk M, Schlemmer HP, Pahernik S (2016) Magnetic resonance imaging-guided transurethral ultrasound ablation of prostate tissue in patients with localized prostate cancer: a prospective phase 1 clinical trial. Eur Urol 70(3):447–455. https://doi.org/10.1016/j.eururo.2015.12.029
Burtnyk M, Hill T, Cadieux-Pitre H, Welch I (2015) Magnetic resonance image guided transurethral ultrasound prostate ablation: a preclinical safety and feasibility study with 28-day followup. J Urol 193(5):1669–1675. https://doi.org/10.1016/j.juro.2014.11.089
Chopra R, Burtnyk M, N’Djin WA, Bronskill M (2010) MRI-controlled transurethral ultrasound therapy for localised prostate cancer. Int J Hyperthermia 26(8):804–821. https://doi.org/10.3109/02656736.2010.503670
Partanen A, Yerram NK, Trivedi H, Dreher MR, Oila J, Hoang AN, Volkin D, Nix J, Turkbey B, Bernardo M, Haines DC, Benjamin CJ, Linehan WM, Choyke P, Wood BJ, Ehnholm GJ, Venkatesan AM, Pinto PA (2013) Magnetic resonance imaging (MRI)-guided transurethral ultrasound therapy of the prostate: a preclinical study with radiological and pathological correlation using customised MRI-based moulds. BJU Int 112(4):508–516. https://doi.org/10.1111/bju.12126
Siddiqui K, Chopra R, Vedula S, Sugar L, Haider M, Boyes A, Musquera M, Bronskill M, Klotz L (2010) MRI-guided transurethral ultrasound therapy of the prostate gland using real-time thermal mapping: initial studies. Urology 76(6):1506–1511. https://doi.org/10.1016/j.urology.2010.04.046
Sapareto SA, Dewey WC (1984) Thermal dose determination in cancer therapy. Int J Radiat Oncol Biol Phys 10(6):787–800
McDannold NJ, King RL, Jolesz FA, Hynynen KH (2000) Usefulness of MR imaging-derived thermometry and dosimetry in determining the threshold for tissue damage induced by thermal surgery in rabbits. Radiology 216(2):517–523. https://doi.org/10.1148/radiology.216.2.r00au42517
Bonekamp D, Wolf MB, Roethke MC, Pahernik S, Hadaschik BA, Hatiboglu G, Kuru TH, Popeneciu IV, Chin JL, Billia M, Relle J, Hafron J, Nandalur KR, Staruch RM, Burtnyk M, Hohenfellner M, Schlemmer HP (2018) Twelve-month prostate volume reduction after MRI-guided transurethral ultrasound ablation of the prostate. Euro Radiol 29:299–308. https://doi.org/10.1007/s00330-018-5584-y
National Cancer Institute; Common Terminology Criteria for Adverse Events (CTCAE) version 4.0; https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed 01.02.2019
Hadaschik BA, Kuru TH, Tulea C, Rieker P, Popeneciu IV, Simpfendorfer T, Huber J, Zogal P, Teber D, Pahernik S, Roethke M, Zamecnik P, Roth W, Sakas G, Schlemmer HP, Hohenfellner M (2011) A novel stereotactic prostate biopsy system integrating pre-interventional magnetic resonance imaging and live ultrasound fusion. J Urol 186(6):2214–2220. https://doi.org/10.1016/j.juro.2011.07.102
Klotz L, Penson D, Chin J, Pavlovich C, Relle J, Koch M, Hatiboglu G, Oto A, Futterer J, Raman SS, Lotan Y, Persigehl T, Heidenreich A, Suarez JF, Staruch R, Burtnyk M, Pantuck A, Sedelaar JP, Arora SS, Zagaja G, Tirkes T, Macura K, Bonekamp D, Haider M, Eggener S (2018) LBA20 MRI-guided transurethral ultrasound ablation (TULSA) in patients with localized prostate cancer: preliminary results of tact pivotal study. J Urol 199(4):e1077–e1078. https://doi.org/10.1016/j.juro.2018.03.091
Ganzer R, Robertson CN, Ward JF, Brown SC, Conti GN, Murat FJ, Pasticier G, Rebillard X, Thuroff S, Wieland WF, Blana A (2011) Correlation of prostate-specific antigen nadir and biochemical failure after high-intensity focused ultrasound of localized prostate cancer based on the stuttgart failure criteria—analysis from the @-Registry. BJU Int 108(8 Pt 2):E196–E201. https://doi.org/10.1111/j.1464-410X.2011.10091.x
Chen PY, Chiang PH, Liu YY, Chuang YC, Cheng YT (2018) Primary whole-gland ablation for localized prostate cancer with high-intensity focused ultrasound: the important predictors of biochemical recurrence. Int J Urol 25(6):615–620. https://doi.org/10.1111/iju.13581
Baumunk D, Andersen C, Heile U, Ebbing J, Cash H, Porsch M, Liehr UB, Janitzky A, Wendler JJ, Schindele D, Blaschke S, Miller K, Schostak M (2013) High-intensity focussed ultrasound in low-risk prostate cancer—oncological outcome and postinterventional quality of life of an inexperienced therapy centre in comparison with an experienced therapy centre. Aktuelle Urol 44(4):285–292. https://doi.org/10.1055/s-0033-1348253
Chaussy C, Thuroff S (2001) Results and side effects of high-intensity focused ultrasound in localized prostate cancer. J Endourol 15(4):437–440. https://doi.org/10.1089/089277901300189501
Crouzet S, Chapelon JY, Rouviere O, Mege-Lechevallier F, Colombel M, Tonoli-Catez H, Martin X, Gelet A (2014) Whole-gland ablation of localized prostate cancer with high-intensity focused ultrasound: oncologic outcomes and morbidity in 1002 patients. Eur Urol 65(5):907–914. https://doi.org/10.1016/j.eururo.2013.04.039
Netsch C, Pfeiffer D, Gross AJ (2010) Development of bladder outlet obstruction after a single treatment of prostate cancer with high-intensity focused ultrasound: experience with 226 patients. J Endourol 24(9):1399–1403. https://doi.org/10.1089/end.2009.0607
Ohigashi T, Nakamura K, Nakashima J, Baba S, Murai M (2007) Long-term results of three different minimally invasive therapies for lower urinary tract symptoms due to benign prostatic hyperplasia: comparison at a single institute. Int J Urol 14(4):326–330. https://doi.org/10.1111/j.1442-2042.2007.01692.x
Chopra R, Burtnyk M, Haider MA, Bronskill MJ (2005) Method for MRI-guided conformal thermal therapy of prostate with planar transurethral ultrasound heating applicators. Phys Med Biol 50(21):4957–4975. https://doi.org/10.1088/0031-9155/50/21/001
Steele GS, Sleep DJ (1997) Transurethral needle ablation of the prostate: a urodynamic based study with 2-year followup. J Urol 158(5):1834–1838
Gravas S, Laguna MP, de la Rosette JJ (2003) Efficacy and safety of intraprostatic temperature-controlled microwave thermotherapy in patients with benign prostatic hyperplasia: results of a prospective, open-label, single-center study with 1-year follow-up. J Endourol 17(6):425–430. https://doi.org/10.1089/089277903767923236
Vesely S, Knutson T, Dicuio M, Damber JE, Dahlstrand C (2005) Transurethral microwave thermotherapy: clinical results after 11 years of use. J Endourol 19(6):730–733. https://doi.org/10.1089/end.2005.19.730
Norby B, Nielsen HV, Frimodt-Moller PC (2002) Transurethral interstitial laser coagulation of the prostate and transurethral microwave thermotherapy vs transurethral resection or incision of the prostate: results of a randomized, controlled study in patients with symptomatic benign prostatic hyperplasia. BJU Int 90(9):853–862
Chaussy C, Thuroff S (2003) The status of high-intensity focused ultrasound in the treatment of localized prostate cancer and the impact of a combined resection. Curr Urol Rep 4(3):248–252
Funding
Profound Medical Inc. helped design and conduct the study, manage and analyze the data, and prepare and approve the manuscript.
Author information
Authors and Affiliations
Contributions
GH: project development, data collection, data analysis, manuscript writing and editing. VP: data collection, data analysis. DB: data collection, data analysis, manuscript writing and editing. MB: project development, data analysis, manuscript writing and editing. RS: project development, data analysis, manuscript writing and editing. SP: project development, data collection, data analysis. GT: data collection, data analysis. JPR: data analysis, manuscript writing and editing. JM: data collection, supervision. HPS: project development, supervision, critical revision of manuscript. MH: project development, manuscript writing and editing, supervision, critical revision of manuscript. JNN-D: data analysis, manuscript writing and editing, supervision, critical revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
R. Staruch and M. Burtnyk are employees of Profound Medical and receive a salary and stock options. The other authors declare, that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hatiboglu, G., Popeneciu, V., Bonekamp, D. et al. Magnetic resonance imaging-guided transurethral ultrasound ablation of prostate tissue in patients with localized prostate cancer: single-center evaluation of 6-month treatment safety and functional outcomes of intensified treatment parameters. World J Urol 38, 343–350 (2020). https://doi.org/10.1007/s00345-019-02784-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02784-w