Abstract
Objectives
To assess the diagnostic accuracy of a junctional zone (JZ) thickness of ≥ 12 mm and morphological features of the JZ in MRI in diagnosing adenomyosis in a premenopausal study population.
Methods
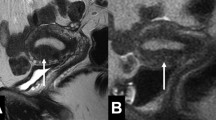
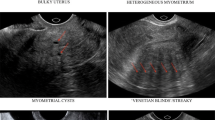
This single-center, prospective observational study consecutively enrolled 93 premenopausal women suffering from a benign gynecological condition, from September 2014 to August 2016. Institutional review board approval and written consent were obtained. All participants underwent MRI and hysterectomy with a histopathological examination. MR images were evaluated in a blinded fashion by two independent readers. The maximum junctional zone thickness (JZmax), presence of JZmax ≥ 12 mm, and any irregular appearance of the JZ (defined as irregular outer or inner borders, focal thickening, presence of high-intensity signal foci, or fingerlike indentations at the inner border) were documented, and the diagnostic performance was evaluated with the AUC, chi-square test, and multiple regression.
Results
Adenomyosis was histopathologically confirmed in 57 (61%) of the women. JZmax was not positively correlated with adenomyosis diagnosis (AUC = 0.57, p = 0.26) and did not differ significantly between those with and without adenomyosis (10.3 vs 10.1 mm, p = 0.88), nor was a cutoff of JZmax ≥ 12 mm (n = 30/57 (53%) vs n = 16/36 (44%), p = 0.29). The presence of an irregular JZ showed the best association with adenomyosis among the evaluated signs (sensitivity 74% (95% CI, 60, 85); specificity 83% (95% CI, 67, 94) (p < 0.001)).
Conclusions
JZmax was not correlated with adenomyosis in the present premenopausal study population, but direct signs of adenomyosis such as irregularities of the JZ provided a good diagnostic accuracy.
Key Points
• Measuring the junctional zone thickness is of limited value for diagnosing adenomyosis with MRI and should not be used for diagnosing adenomyosis in premenopausal women with moderate disease severity.
• An irregular appearance of the junctional zone, the presence of myometrial cysts, and adenomyoma appear to provide the highest specificity for diagnosing adenomyosis.
• A consensus for the definition and reading of the junctional zone is needed.





Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the receiver operating characteristics curve
- ICC:
-
Intraclass correlation coefficient
- JZ:
-
Junctional zone
- MRI:
-
Magnetic resonance imaging
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- R1:
-
Reader 1
- R2:
-
Reader 2
- ROC:
-
Receiver operating characteristics
- T1W:
-
T1-weighted
- T2W:
-
T2-weighted
- TSE:
-
Turbo spin echo
References
Naftalin J, Hoo W, Pateman K, Mavrelos D, Holland T, Jurkovic D (2012) How common is adenomyosis? A prospective study of prevalence using transvaginal ultrasound in a gynaecology clinic. Hum Reprod 27:3432–3439
Bird CC, McElin TW, Manalo-Estrella P (1972) The elusive adenomyosis of the uterus--revisited. Am J Obstet Gynecol 112:583–593
Choi EJ, Cho SB, Lee SR et al (2017) Comorbidity of gynecological and non-gynecological diseases with adenomyosis and endometriosis. Obstet Gynecol Sci 60:579–586
Li X, Liu X, Guo SW (2014) Clinical profiles of 710 premenopausal women with adenomyosis who underwent hysterectomy. J Obstet Gynaecol Res 40:485–494
Younes G, Tulandi T (2017) Effects of adenomyosis on in vitro fertilization treatment outcomes: a meta-analysis. Fertil Steril 108:483–490 e483
Bruun MR, Arendt LH, Forman A, Ramlau-Hansen CH (2018) Endometriosis and adenomyosis are associated with increased risk of preterm delivery and a small-for-gestational-age child: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 97:1073–1090
Bazot M, Darai E (2018) Role of transvaginal sonography and magnetic resonance imaging in the diagnosis of uterine adenomyosis. Fertil Steril 109:389–397
Agostinho L, Cruz R, Osorio F, Alves J, Setubal A, Guerra A (2017) MRI for adenomyosis: a pictorial review. Insights Imaging 8:549–556
Reinhold C, McCarthy S, Bret PM et al (1996) Diffuse adenomyosis: comparison of endovaginal US and MR imaging with histopathologic correlation. Radiology 199:151–158
Dueholm M, Lundorf E, Hansen ES, Sorensen JS, Ledertoug S, Olesen F (2001) Magnetic resonance imaging and transvaginal ultrasonography for the diagnosis of adenomyosis. Fertil Steril 76:588–594
Bazot M, Cortez A, Darai E et al (2001) Ultrasonography compared with magnetic resonance imaging for the diagnosis of adenomyosis: correlation with histopathology. Hum Reprod 16:2427–2433
Tellum T, Nygaard S, Skovholt EK, Qvigstad E, Lieng M (2018) Development of a clinical prediction model for diagnosing adenomyosis. Fertil Steril 110:957–964
Byun JY, Kim SE, Choi BG, Ko GY, Jung SE, Choi KH (1999) Diffuse and focal adenomyosis: MR imaging findings. Radiographics 19 Spec No:S161–S170
Tamai K, Togashi K, Ito T, Morisawa N, Fujiwara T, Koyama T (2005) MR imaging findings of adenomyosis: correlation with histopathologic features and diagnostic pitfalls. Radiographics 25:21–40
Togashi K, Nishimura K, Itoh K et al (1988) Adenomyosis: diagnosis with MR imaging. Radiology 166:111–114
Togashi K, Ozasa H, Konishi I et al (1989) Enlarged uterus: differentiation between adenomyosis and leiomyoma with MR imaging. Radiology 171:531–534
Stamatopoulos CP, Mikos T, Grimbizis GF et al (2012) Value of magnetic resonance imaging in diagnosis of adenomyosis and myomas of the uterus. J Minim Invasive Gynecol 19:620–626
Van den Bosch T, Dueholm M, Leone FP et al (2015) Terms, definitions and measurements to describe sonographic features of myometrium and uterine masses: a consensus opinion from the Morphological Uterus Sonographic Assessment (MUSA) group. Ultrasound Obstet Gynecol 46:284–298
Novellas S, Chassang M, Delotte J et al (2011) MRI characteristics of the uterine junctional zone: from normal to the diagnosis of adenomyosis. AJR Am J Roentgenol 196:1206–1213
Tamai K, Koyama T, Umeoka S, Saga T, Fujii S, Togashi K (2006) Spectrum of MR features in adenomyosis. Best Pract Res Clin Obstet Gynaecol 20:583–602
Bergeron C, Amant F, Ferenczy A (2006) Pathology and physiopathology of adenomyosis. Best Pract Res Clin Obstet Gynaecol 20:511–521
Machin D, Campbell MJ, Tan SB, Tan SH (2008) Sample size tables for clinical studies, 3rd edn. Wiley-Blackwell, Oxford
Watson PF, Petrie A (2010) Method agreement analysis: a review of correct methodology. Theriogenology 73:1167–1179
Mehasseb MK, Bell SC, Brown L, Pringle JH, Habiba M (2011) Phenotypic characterisation of the inner and outer myometrium in normal and adenomyotic uteri. Gynecol Obstet Invest 71:217–224
Halligan S, Altman DG, Mallett S (2015) Disadvantages of using the area under the receiver operating characteristic curve to assess imaging tests: a discussion and proposal for an alternative approach. Eur Radiol 25:932–939
Kang S, Turner DA, Foster GS, Rapoport MI, Spencer SA, Wang JZ (1996) Adenomyosis: specificity of 5 mm as the maximum normal uterine junctional zone thickness in MR images. AJR Am J Roentgenol 166:1145–1150
Acknowledgments
The authors thank Else Kathrine Skovholt, M.D. for the analysis of the histopathological specimen.
Funding
The first author received a PhD-grant from the Norwegian Women’s Health Association (Norske Kvinners Sanitetsforening) to perform this study (grant number NKS14901), who was involved in neither the design, data analysis, nor publication of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Marit Lieng.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Staale Nygaard kindly provided statistical advice for this manuscript. Also, several of the authors have significant statistical expertise. However, no complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Ultrasound examination was performed on the whole study cohort; the results are reported elsewhere [12]. The data reported in this article have no overlap with previously published work.
Methodology
• Prospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Table 1
Protocol for magnetic resonance imaging.aPerpendicular to the long axis of the uterine cavity. bParallel to the long axis of the uterine cavity. T1W, T1-weighted; T2W, T2-weighted; B-TFE, balanced turbo field echo; TSE, turbo spin echo; VISTA, Volumetric Isotropic TSE Acquisition (DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Tellum, T., Matic, G.V., Dormagen, J.B. et al. Diagnosing adenomyosis with MRI: a prospective study revisiting the junctional zone thickness cutoff of 12 mm as a diagnostic marker. Eur Radiol 29, 6971–6981 (2019). https://doi.org/10.1007/s00330-019-06308-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06308-3