Abstract
Background and purpose
Notwithstanding guidelines, indications for mechanical thrombectomy (MT) in acute ischemic stroke are multifactorial and can be complex. Our aim was to exploratively evaluate decision-making on the advisability of performing MT in cases presented as an interview-administered questionnaire.
Methods
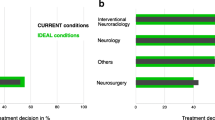
Fifty international raters assessed 12 cases and decided to recommend or exclude MT. Each case contained a brief summary of clinical information and eight representative images of the initial multimodal CT. The demographic characteristics and stroke protocols were recorded for raters. For each case, the reasons for excluding MT were recorded. Uni- and multivariate logistic regression analysis were performed for the different demographic and case characteristics to identify factors that might influence decision-making.
Results
All raters performed MT (median MTs/hospital/year [IQR], 100 [50–141]) with a median of 7 years of experience as first operator (IQR, 4–12). Per case, diversity in decision-making ranged between 1 (case 6, 100% yes MT) and 0.50 (case 12, 54.2% yes MT and 45.8% no MT). The most common reasons for excluding MT were small CBV/CBF mismatch (17%, 102/600), size of infarct core on the CBV map (15.2%, 91/600), and low NIHSS score (National Institute of Health Stroke Scale, 8.3%, 50/600). All clinical and radiological characteristics significantly affected the decision regarding MT, but the general characteristics of the raters were not a factor.
Conclusions
Clinical and imaging characteristics influenced the decision regarding MT in stroke. Nevertheless, a consensus was reached in only a minority of cases, revealing the current divergence of opinion regarding therapeutic decisions in difficult cases.
Key Points
• This is the first study to explore differences in decision-making in respect of mechanical thrombectomy in ischemic stroke with complex clinical and radiological constellations.
• Fifty experienced international neurointerventionalists answered this interview-administered stroke questionnaire and made decisions as to whether to recommend or disadvise thrombectomy in 12 selected cases.
• Diversity in decision-making for thrombectomy ranged from 1 (100% of raters offered the same answer) to 0.5 (50% indicated mechanical thrombectomy). There was a consensus in only a minority of cases, revealing the current disparity of opinion regarding therapeutic decisions in difficult cases.

Similar content being viewed by others
Abbreviations
- ACA:
-
Anterior cerebral artery
- CI:
-
Confidence intervals
- CTA:
-
CT angiography
- CTP:
-
CT perfusion
- GEEs:
-
Generalized estimation equations
- ICA:
-
Internal carotid artery
- IQR:
-
Interquartile range
- LR:
-
Logistic regression
- MCA:
-
Middle cerebral artery
- MT:
-
Mechanical thrombectomy
- NECT:
-
Non-enhanced CT
- NIHSS:
-
National Institute of Health Stroke Scale
- OR:
-
Odds ratio
- SR:
-
Stent retriever
References
Powers WJ, Derdeyn CP, Biller J et al (2015) 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:3020–3035
Powers WJ, Rabinstein AA, Ackerson T et al (2018) 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49:e46–e110
Higgs J, Jones MA, Lufthus S et al (2007) Clinical reasoning in the health professions Elsevier-Health Sciences Division, ed: Heidi Harrison; 2007. Smith M, Higgs J, Ellis E Chapter 8: Factors influencing clinical decision making 89–98
Thomson RG, De Brún A, Flynn D et al (2017) Factors that influcence variation in clinical decision-making about thrombolysis in the treatment of acute ischemic stroke: results of a discrete choice experiment. HIHR Journals Library (Health Services and Delivery Rearch), Southampton
De Brún A, Flynn D, Ternent L et al (2018) Factors that influence clinicians' decisions to offer intravenous alteplase in acute ischemic stroke patients with uncertain treatment indication: results of a discrete choice experiment. Int J Stroke 13:74–82
Levine SR, Weingast SZ, Weedon J et al (2018). To treat or not to treat? Exploring factors influencing intravenous thrombolysis Treatment decisions for minor stroke. Stroke 49:1933–1938
Simpson EH (1949) Measurement of diversity. Nature 163:688
McLaughlin JE, McLaughlin GW, McLaughlin JS, White CY (2016) Using Simpson’s diversity index to examine multidimensional models of diversity in health professions education. Int J Med Educ 7:1–5
Lewis ML (1997) Decision-making task complexity: model development and initial testing. J Nurs Educ 36:114–120
Raza SA, Rangaraju S (2018) A review of pre-intervention prognostic scores for early prognostication and patient selection in endovascular management of large vessel occlusion stroke. Interv Neurol 7:171–181
Liebeskind DS, Jahan R, Nogueira RG et al (2016) Early arrival at the emergency department is associated with better collaterals, smaller established infarcts and better clinical outcomes with endovascular stroke therapy: SWIFT study. J Neurointerv Surg 8:553–558
Broussalis E, Weymayr F, Hitzl W et al (2016) Endovascular mechanical recanalization of acute ischaemic stroke in octogenarians. Eur Radiol 26:1742–1750
Adams HP Jr, Davis PH, Leira EC et al (1999) Baseline NIH stroke scale score strongly predicts outcome after stroke: a report of the trial of org 10172 in Acute Stroke Treatment (TOAST). Neurology 53:126–131
Rebello LC, Bouslama M, Haussen DC et al (2017) Endovascular treatment for patients with acute stroke who have a large ischemic core and large mismatch imaging profile. JAMA Neurol 74:34–40
Wannamaker R, Guinand T, Menon BK et al (2018) Computed tomographic perfusion predicts poor outcomes in a randomized trial of endovascular therapy. Stroke 49:1426–1433
Pexman JH, Barber PA, Hill MD et al (2001) Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol 22:1534–1542
Saposnik G, Johnston SC (2014) Decision making in acute stroke care: learning from neuroeconomics, neuromarketing, and poker players. Stroke 45:2144–2150
Elstein AS, Schwartz A (2002) Clinical problem solving and diagnostic decision making: selective review of the cognitive literature. BMJ 324:729–732
Shamy MC, Jaigobin CS (2013) The complexities of acute stroke decision-making: a survey of neurologists. Neurology 81:1130–1133
Scharf J, Brockmann MA, Daffertshofer M et al (2006) Improvement of sensitivity and interrater reliability to detect acute stroke by dynamic perfusion computed tomography and computed tomography angiography. J Comput Assist Tomogr 30:105–110
Campbell BC, Mitchell PJ, Kleinig TJ et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009–1018
Tsogkas I, Knauth M, Schregel K et al (2016) Added value of CT perfusion compared to CT angiography in predicting clinical outcomes of stroke patients treated with mechanical thrombectomy. Eur Radiol 26:4213–4219
Kloska SP, Nabavi DG, Gaus C et al (2004) Acute stroke assessment with CT: do we need multimodal evaluation? Radiology 233:79–86
Sheth SA, Yoo B, Saver JL et al (2015) M2 occlusions as targets for endovascular therapy: comprehensive analysis of diffusion/perfusion MRI, angiography, and clinical outcomes. J Neurointerv Surg 7:478–483
Moreau F, Asdaghi N, Modi J, Goyal M, Coutts SB (2013) Magnetic resonance imaging versus computed tomography in transient ischemic attack and minor stroke: the more upsilonou see the more you know. Cerebrovasc Dis Extra 3:130–136
Vert C, Parra-Farinas C, Rovira A (2017) MR imaging in hyperacute ischemic stroke. Eur J Radiol 96:125–132
Campbell BC, Purushotham A, Christensen S et al (2012) The infarct core is well represented by the acute diffusion lesion: sustained reversal is infrequent. J Cereb Blood Flow Metab 32:50–56
Albers GW, Thijs VN, Wechsler L et al (2006) Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann Neurol 60:508–517
Acknowledgements
Aglae Velasco Gonzalez performed this study during a six months fellowship in the Institute of Biostatistics and Clinical Research from the Faculty of Medicine, Westfälische Wilhelms-Universität Münster (WWU). The authors thank the University of Muenster (WWU) for giving us the time to complete this project. We wish to thank all the raters from various countries that participated in this questionnaire and especially Dr. Miguel Castaño (Spain) whose enthusiasm and support enabled us to recruit the ideal number of participants for this stroke questionnaire on mechanical thrombectomy.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Aglaé Velasco González.
Conflict of interest
All authors disclosed no relevant relationships related to the present article. One author (RC) disclosed activities not related to the present article: author received payment from Balt, EV3, and Microvention for consultancy, expert testimony, and payment for lectures.
Statistics and biometry
Two authors of the Institute of Biostatistics and Clinical Research of the University of Muenster conducted the statistical analysis (Dennis Görlich and Cristina Sauerland). One third author (Aglaé Velasco González) participated in the statistical analyses.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• cross-sectional study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 6729 kb)
Rights and permissions
About this article
Cite this article
Velasco González, A., Buerke, B., Görlich, D. et al. Variability in the decision-making process of acute ischemic stroke in difficult clinical and radiological constellations: analysis based on a cross-sectional interview-administered stroke questionnaire. Eur Radiol 29, 6275–6284 (2019). https://doi.org/10.1007/s00330-019-06199-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06199-4