Abstract
Purpose
To construct a decision tree based on CT findings to differentiate acute pelvic inflammatory disease (PID) from acute appendicitis (AA) in women with lower abdominal pain and inflammatory syndrome.
Materials and methods
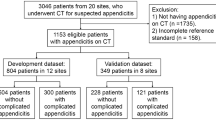
This retrospective study was approved by our institutional review board and informed consent was waived. Contrast-enhanced CT studies of 109 women with acute PID and 218 age-matched women with AA were retrospectively and independently reviewed by two radiologists to identify CT findings predictive of PID or AA. Surgical and laboratory data were used for the PID and AA reference standard. Appropriate tests were performed to compare PID and AA and a CT decision tree using the classification and regression tree (CART) algorithm was generated.
Results
The median patient age was 28 years (interquartile range, 22–39 years). According to the decision tree, an appendiceal diameter ≥ 7 mm was the most discriminating criterion for differentiating acute PID and AA, followed by a left tubal diameter ≥ 10 mm, with a global accuracy of 98.2 % (95 % CI: 96–99.4).
Conclusion
Appendiceal diameter and left tubal thickening are the most discriminating CT criteria for differentiating acute PID from AA.
Key points
• Appendiceal diameter and marked left tubal thickening allow differentiating PID from AA.
• PID should be considered if appendiceal diameter is < 7 mm.
• Marked left tubal diameter indicates PID rather than AA when enlarged appendix.
• No pathological CT findings were identified in 5 % of PID patients.






Similar content being viewed by others
Abbreviations
- AA:
-
Acute appendicitis
- CART:
-
Classification and regression tree
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- ICD:
-
International classification of diseases
- IQR:
-
Interquartile range
- IUD:
-
Intrauterine device
- PID:
-
Pelvic inflammatory disease
- TOA:
-
Tubo-ovarian abscess
References
Sellors J, Mahony J, Goldsmith C et al (1991) The accuracy of clinical findings and laparoscopy in pelvic inflammatory disease. Am J Obstet Gynecol 164:113–120
Centers for Disease Control and Prevention (2010) Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep 59:63–67
Morcos R, Frost N, Hnat M, Petrunak A, Caldito G (1993) Laparoscopic versus clinical diagnosis of acute pelvic inflammatory disease. J Reprod Med 38:53–56
Maleckiene L, Kajenas S, Nadisauskiene RJ, Railaite DR (2009) Comparison of clinical and laparoscopic diagnoses of pelvic inflammatory disease. Int J Gynaecol Obstet 104:74–75
Bongard F, Landers DV, Lewis F (1985) Differential diagnosis of appendicitis and pelvic inflammatory disease. A prospective analysis. Am J Surg 150:90–96
Webster DP, Schneider CN, Cheche S, Daar AA, Miller G (1993) Differentiating acute appendicitis from pelvic inflammatory disease in women of childbearing age. Am J Emerg Med 11:569–572
Morishita K, Gushimiyagi M, Hashiguchi M, Stein GH, Tokuda Y (2007) Clinical prediction rule to distinguish pelvic inflammatory disease from acute appendicitis in women of childbearing age. AmJ Emerg Med 25:152–157
Weström L, Joesoef R, Reynolds G, Hagdu A, Thompson SE (1992) Pelvic inflammatory disease and fertility. A cohort study of 1,844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results. Sex Transm Dis 19:185–192
Buchan H, Vessey M, Goldacre M, Fairweather J (1993) Morbidity following pelvic inflammatory disease. Br J Obstet Gynaecol 100:558–562
Van Randen A, Bipat S, Zwinderman AH, Ubbink DT, Stoker J, Boermeester MA (2008) Acute appendicitis: metaanalysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology 249:97–106
Bhosale PR, Javitt MC, Atri M et al (2016) ACR Appropriateness Criteria® Acute Pelvic Pain in the Reproductive Age Group. Ultrasound Q. 32:108–115
Jung SI, Kim YJ, Park HS, Jeon HJ, Jeong K-A (2011) Acute pelvic inflammatory disease: diagnostic performance of CT. J Obstet Gynaecol Res 37:228–235
Lee MH, Moon MH, Sung CK, Woo H, Oh S (2014) CT findings of acute pelvic inflammatory disease. Abdom Imaging 39:1350–1355
Rao PM, Rhea JT, Novelline RA (1997) Sensitivity and specificity of the individual CT signs of appendicitis: experience with 200 helical appendiceal CT examinations. J Comput Assist Tomogr 21:686–692
Choi D, Park H, Lee YR et al (2003) The most useful findings for diagnosing acute appendicitis on contrast-enhanced helical CT. Acta Radiol 44:574–582
Ives EP, Sung S, McCue P, Durrani H, Halpern EJ (2008) Independent predictors of acute appendicitis on CT with pathologic correlation. Acad Radiol 15:996–1003
Van Randen A, Lameris W, van Es HW et al (2010) Profiles of US and CT imaging features with a high probability of appendicitis. Eur Radiol 20:1657–1666
Godwin BD, Drake FT, Simianu VV et al (2015) A novel reporting system to improve accuracy in appendicitis imaging. Am J Roentgenol 204:1212–1219
Eshed I, Halshtok O, Erlich Z et al (2011) Differentiation between right tubo-ovarian abscess and appendicitis using CT-a diagnostic challenge. Clin Radiol 66:1030–1035
Hiller N, Fux T, Finkelstein A, Mezeh H, Simanovsky N (2016) CT differentiation between tubo-ovarian and appendiceal origin of right lower quadrant abscess: CT, clinical, and laboratory correlation. Emerg Radiol 23:133–139
Quentin R, Verdon R (2012) Microbiologic basis of diagnosis and treatment of pelvic inflammatory disease. J Gynecol Obstet Biol Reprod 41:850–863
Cabarrus M, Sun YL, Courtier JL, Stengel JW, Coakley FV, Webb EM (2013) The prevalence and patterns of intraluminal air in acute appendicitis at CT. Emerg Radiol 20:51–56
Hong HS, Cho HS, Woo JY et al (2016) Intra-Appendiceal Air at CT: Is It a Useful or a Confusing Sign for the Diagnosis of Acute Appendicitis? Korean J Radiol 17:39–46
Rothrock SG, Green SM, Dobson M, Colucciello SA, Simmons CM (1995) Misdiagnosis of appendicitis in nonpregnant women of childbearing age. J Emerg Med 13:1–8
Kim MY, Lee YM, Suh CH, Kim JM (2007) Computed tomographic features of appendiceal serositis in pelvic inflammatory disease: comparison with pathological findings. J Comput Assist Tomogr 31:104–108
Kılınçer A, Akpınar E, Erbil B et al (2017) A new technique for the diagnosis of acute appendicitis: abdominal CT with compression to the right lower quadrant. Eur Radiol. https://doi.org/10.1007/s00330-016-4728-1
Nikolaidis P, Hwang CM, Miller FH, Papanicolaou N (2004) The nonvisualized appendix: incidence of acute appendicitis when secondary inflammatory changes are absent. AJR 183:889–892
Ganguli S, Raptopoulos V, Komlos F, Siewert B, Kruskal JB (2006) Right lower quadrant pain: value of the nonvisualized appendix in patients at multidetector CT. Radiology 241:175–180
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Patrice Taourel.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Funding
The authors state that this work has not received any funding.
Statistics and biometry
Dr Molinari Nicolas kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
El Hentour, K., Millet, I., Pages-Bouic, E. et al. How to differentiate acute pelvic inflammatory disease from acute appendicitis ? A decision tree based on CT findings. Eur Radiol 28, 673–682 (2018). https://doi.org/10.1007/s00330-017-5032-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5032-4