Abstract
Objectives
To evaluate whether visual assessment of T2-weighted imaging (T2WI) or an apparent diffusion coefficient (ADC) could predict lymphovascular invasion (LVI) status in cases with clinically node-negative invasive breast cancer.
Materials and methods
One hundred and thirty-six patients with 136 lesions underwent MRI. Visual assessment of T2WI, tumour-ADC, peritumoral maximum-ADC and the peritumour-tumour ADC ratio (the ratio between them) were compared with LVI status of surgical specimens.
Results
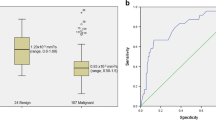
No significant relationship was found between LVI and T2WI. Tumour-ADC was significantly lower in the LVI-positive (n = 77, 896 ± 148 × 10−6 mm2/s) than the LVI-negative group (n = 59, 1002 ± 163 × 10−6 mm2/s; p < 0.0001). Peritumoral maximum-ADC was significantly higher in the LVI-positive (1805 ± 355 × 10−6 mm2/s) than the LVI-negative group (1625 ± 346 × 10−6 mm2/s; p = 0.0003). Peritumour-tumour ADC ratio was significantly higher in the LVI-positive (2.05 ± 0.46) than the LVI-negative group (1.65 ± 0.40; p < 0.0001). Receiver operating characteristic curve analysis revealed that the area under the curve (AUC) of the peritumour-tumour ADC ratio was the highest (0.81). The most effective threshold for the peritumour-tumour ADC ratio was 1.84, and the sensitivity, specificity, positive predictive value and negative predictive value were 77 % (59/77), 76 % (45/59), 81 % (59/73) and 71 % (45/63), respectively.
Conclusions
We suggest that the peritumour-tumour ADC ratio can assist in predicting LVI status on preoperative imaging.
Key points
• Tumour ADC was significantly lower in LVI-positive than LVI-negative breast cancer.
• Peritumoral maximum-ADC was significantly higher in LVI-positive than LVI-negative breast cancer.
• Peritumour-tumour ADC ratio was significantly higher in LVI-positive breast cancer.
• Diagnostic performance of the peritumour-tumour ADC ratio was highest for positive LVI.
• Peritumour-tumour ADC ratio showed higher diagnostic ability in postmenopausal than premenopausal patients.




Similar content being viewed by others
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- DWI:
-
Diffusion-weighted imaging
- Her2:
-
Human epidermal growth factor receptor 2
- LVI:
-
Lymphovascular invasion
- MRI:
-
Magnetic resonance imaging
- NOS:
-
Not otherwise specified
- T2WI:
-
T2-weighted imaging
- ROI:
-
Region of interest
References
Rosen P (2014) Rosen’s breast pathology, 4th edn. Lippincott Williams & Wilkins, Philadelphia
Rosen PP (1983) Tumor emboli in intramammary lymphatics in breast carcinoma: pathologic criteria for diagnosis and clinical significance. Pathol Annu 18:215–232
Liljegren G, Holmberg L, Bergh J et al (1999) 10-Year results after sector resection with or without postoperative radiotherapy for stage I breast cancer: a randomized trial. J Clin Oncol 17:2326–2326
Lee AHS, Pinder SE, Macmillan RD et al (2006) Prognostic value of lymphovascular invasion in women with lymph node negative invasive breast carcinoma. Eur J Cancer 42:357–362
Rosen PP, Saigo PE, Braun DW Jr et al (1981) Predictors of recurrence in stage I (T1N0M0) breast carcinoma. Ann Surg 193:15
Matsuda N, Hayashi N, Ohde S et al (2014) A nomogram for predicting locoregional recurrence in primary breast cancer patients who received breast-conserving surgery after neoadjuvant chemotherapy: A Nomogram for LRR in Breast Cancer. J Surg Oncol n/a–n/a. doi:10.1002/jso.23586
Ugras S, Stempel M, Patil S, Morrow M (2014) Estrogen Receptor, Progesterone Receptor, and HER2 Status Predict Lymphovascular Invasion and Lymph Node Involvement. Ann Surg Oncol. doi:10.1245/s10434-014-3851-y
Caudle AS, Yu T-K, Tucker SL et al (2012) Local-regional control according to surrogate markers of breast cancer subtypes and response to neoadjuvant chemotherapy in breast cancer patients undergoing breast conserving therapy. Breast Cancer Res 14:R83
De Mascarel I, Bonichon F, Durand M et al (1998) Obvious peritumoral emboli: an elusive prognostic factor reappraised. Multivariate analysis of 1320 node-negative breast cancers. Eur J Cancer 34:58–65
Kurosumi (2011) Pathological tumor response to neoadjuvant chemotherapy using anthracycline and taxanes in patients with triple-negative breast cancer. Exp Ther Med. doi:10.3892/etm.2011.212
Lin P-H, Yeh M-H, Liu L-C et al (2013) Clinical and pathologic risk factors of tumor recurrence in patients with node-negative early breast cancer after mastectomy: Risk Factors of Recurrence in NNBC. J Surg Oncol 108:352–357
Chue KM, Yong WS, Thike AA et al (2014) Predicting the likelihood of additional lymph node metastasis in sentinel lymph node positive breast cancer: validation of the Memorial Sloan-Kettering Cancer Centre (MSKCC) nomogram. J Clin Pathol 67:112–119
Rosen DF (1982) Pathologic predictors of recurrence in stage 1 (TINOMO) breast cancer. Am J Clin Pathol 78:817–820
Fisher ER, Anderson S, Redmond C, Fisher B (1993) Pathologic findings from the National Surgical Adjuvant Breast Project protocol B-06. 10-year pathologic and clinical prognostic discriminants. Cancer 71:2507–2514
Reynders A, Brouckaert O, Smeets A et al (2014) Prediction of non-sentinel lymph node involvement in breast cancer patients with a positive sentinel lymph node. Breast 23:453–459
Verheuvel NC, van den Hoven I, Ooms HWA et al (2014) The Role of Ultrasound-Guided Lymph Node Biopsy in Axillary Staging of Invasive Breast Cancer in the Post-ACOSOG Z0011 Trial Era. Ann Surg Oncol. doi:10.1245/s10434-014-4071-1
Galimberti V, Bernard F, Cole UV (2013) Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23–01): a phase 3 randomised controlled trial. Lancet Oncol 14:297–305
Viale G, Maiorano E, Pruneri G et al (2005) Predicting the Risk for Additional Axillary Metastases in Patients With Breast Carcinoma and Positive Sentinel Lymph Node Biopsy. Ann Surg 241:319–325
Uematsu T, Kasami M, Watanabe J (2013) Is evaluation of the presence of prepectoral edema on T2-weighted with fat-suppression 3 T breast MRI a simple and readily available noninvasive technique for estimation of prognosis in patients with breast cancer? Breast Cancer. doi:10.1007/s12282-013-0440-z
Sugahara T, Korogi Y, Kochi M et al (1999) Usefulness of diffusion-weighted MRI with echo-planar technique in the evaluation of cellularity in gliomas. J Magn Reson Imaging JMRI 9:53–60
Mori N, Ota H, Mugikura S et al (2013) Detection of invasive components in cases of breast ductal carcinoma in situ on biopsy by using apparent diffusion coefficient MR parameters. Eur Radiol 23:2705–2712
Asao C, Korogi Y, Kitajima M et al (2005) Diffusion-weighted imaging of radiation-induced brain injury for differentiation from tumor recurrence. Am J Neuroradiol 26:1455–1460
Tien RD, Felsberg GJ, Friedman H et al (1994) MR imaging of high-grade cerebral gliomas: value of diffusion-weighted echoplanar pulse sequences. AJR Am J Roentgenol 162:671–677
Mori N, Ota H, Mugikura S et al (2014) Luminal-type breast cancer: correlation of apparent diffusion coefficients with the Ki-67 labeling index. Radiology 274:66–73
Sunil L, Ian E, Stuart S (2012) World Health Organization Classification of Tumors of the Breast. IARC. http://apps.who.int/bookorders/anglais/detart1.jsp?codlan=1&codcol=70&codcch=4004
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Gudlaugsson E, Skaland I, Undersrud E et al (2011) D2-40/p63 defined lymph vessel invasion has additional prognostic value in highly proliferating operable node negative breast cancer patients. Mod Pathol 24:502–511
Ramakrishnan R, Khan SA, Badve S (2002) Morphological changes in breast tissue with menstrual cycle. Mod Pathol 15:1348–1356
Mussurakis S (1997) Dynamic MR imaging of invasive breast cancer: correlation with tumour grade and other histological factors. Br Inst Radiol 70:446–451
Braithwaite AC, Dale BM, Boll DT, Merkle EM (2009) Short-and midterm reproducibility of apparent diffusion coefficient measurements at 3.0-T diffusion-weighted imaging of the Abdomen1. Radiology 250:459–465
Sioshansi S, Ehdaivand S, Cramer C et al (2012) Triple negative breast cancer is associated with an increased risk of residual invasive carcinoma after lumpectomy. Cancer 118:3893–3898
Torabi R, Hsu C-H, Patel PN et al (2013) Predictors of margin status after breast-conserving operations in an underscreened population. Langenbecks Arch Surg 398:455–462
Bogner W, Gruber S, Pinker K et al (2009) Diffusion-weighted MR for differentiation of breast lesions at 3.0 T: how does selection of diffusion protocols affect diagnosis? 1. Radiology 253:341–351
Onishi N, Kanao S, Kataoka M et al (2014) Apparent diffusion coefficient as a potential surrogate marker for Ki-67 index in mucinous breast carcinoma: ADC as a Marker for Ki-67 Index in MBC. J Magn Reson Imaging n/a–n/a. doi:10.1002/jmri.24615
Acknowledgements
The authors thank Tatsuo Nagasaka, RT, Kazuomi Yamanaka, RT, Hironobu Sasaki, RT, Tomoyoshi Kimura, RT, of Tohoku University Hospital, Sendai, Japan, for their excellent technical assistance and kind support. The scientific guarantor of this publication is Shoki Takahashi. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. Methodology: retrospective, diagnostic, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mori, N., Mugikura, S., Takasawa, C. et al. Peritumoral apparent diffusion coefficients for prediction of lymphovascular invasion in clinically node-negative invasive breast cancer. Eur Radiol 26, 331–339 (2016). https://doi.org/10.1007/s00330-015-3847-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3847-4