Abstract
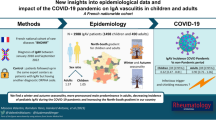
The impact of the COVID-19 pandemic, and implemented restrictions on the frequency of pediatric rheumatic diseases remain unknown, while they have probably prevented common infections in children. We present the effects of the COVID-19 on our pediatric rheumatology practice in a main referral center. We retrospectively reviewed the medical records of patients presenting to pediatric rheumatology department in 4 years before March 2020 and compared it to the pandemic year (March 2020–March 2021). Since there was an overall decrease in patient numbers, we calculated the percentage according to the total number of that year. A total of 32,333 patients were evaluated. The mean annual number of patients decreased by 42% during the COVID-19 pandemic. When follow-up visits (25,156) were excluded, there were 2818 new diagnoses of rheumatic diseases. In the pre-pandemic period, familial Mediterranean fever (FMF) (n = 695, 28.1%) was the most frequent, whereas in the pandemic period multisystem inflammatory syndrome in children (MIS-C) (n = 68, 19.2%) was the most common diagnosis. There were no significant differences in the percentages of juvenile idiopathic arthritis, autoimmune diseases, rare autoinflammatory diseases, and other vasculitides. However, there was a significant decrease in patients diagnosed with FMF, IgA vasculitis (IgAV), acute rheumatic fever (ARF), classic Kawasaki disease (KD), and macrophage activation syndrome (MAS) (all p < 0.05). During the pandemic year, the percentage of most common diseases did not differ. On the other hand, we suggest that the decreases in IgAV, KD (classic), and MAS, which parallels the decrease in ARF, confirm the role of infections in the pathogenesis for these diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronavirus disease (COVID-19) infection emerged from Wuhan, China, in late December 2019 and spread around the world in a short period [1]. The World Health Organization (WHO) has declared the COVID-19 a global pandemic on March 11, 2020 [2]. It has affected people of all ages, all over the world. The true incidence of COVID-19 infection in children is not known due to insufficient testing and asymptomatic infection. As of September 23, 2021, more than 5,7 million cases associated with SARS-CoV-2 in children were reported from the American Academy of Pediatrics and the Children’s Hospital Association and children represented 16.0% of all cases [3]. Children also made up 0.00–0.27% of all COVID-19 deaths [3]. In Turkey, there have been 7,039,500 confirmed cases of COVID-19, including 63,166 deaths, reported to WHO between 3 January 2020 and 27 September 2021 [4]. However, there are limited data related to the epidemiology of COVID-19 infection among children in our country.
Our views about the impact of COVID-19 infection on children have changed over time. In the early stages of the pandemic, children were thought to be less susceptible to COVID-19 infection and have mild symptoms, unlike the disease course in adults [5, 6]. However, subsequently, it became apparent that children could develop a very severe multisystem inflammatory syndrome [7, 8]. In a systematic review of the clinical course of COVID-19 in pediatric patients, the asymptomatic disease was present in 14.2%, mild 36.3%, moderate in 46.0%, severe in 2.1%, and critical disease in 1.2 percent [9]. The rate of asymptomatic infection in children and adolescents (younger than 20 years) has been reported between 14.6 and 42% [10]. In those with symptoms of COVID-19, fever (46–64.2%) and cough (32–55.9%) are the leading symptoms [10, 11].
COVID-19 has also led to dramatic changes in our daily life such as wearing masks, social distancing, quarantine, and curfews. These measures seem to have resulted in decreased transmission of other infectious agents. In a study from Singapore, the influenza frequency in the COVID-19 period was compared with the frequency in three preceding years: a remarkable decrease was found in the COVID-19 period and suggested that the spread of viral infections could be reduced with the measures taken [12]. Moreover, it was reported in another study that a decrease in hospital admissions was observed not only in influenza infections but also in infections with other respiratory viruses [13].
Childhood rheumatic diseases are multisystem disorders characterized by acute and chronic inflammation of the musculoskeletal system, vessels, and skin. The association between infections and rheumatic diseases has long been known [14]. Infectious agents may play a role in the etiology and act as triggers for the rheumatic diseases. On the other hand, infections are a major cause of morbidity and mortality in patients receiving heavy immunosuppressive treatments for their rheumatic diseases [15, 16]. During the pandemic, the course of COVID-19 in patients with rheumatic diseases, how it affects the course of the disease, and how the treatment should be regulated have been a serious concern for physicians. Extensive studies have been carried out on these issues [17, 18]. However, the impact of the COVID-19 pandemic and the implemented restrictions on the frequency and course of pediatric rheumatic diseases remain unknown. We have aimed to investigate the effect of the COVID-19 pandemic on the prevalence of pediatric rheumatic diseases in our referral center.
Methods
We retrospectively reviewed medical records of patients presenting to the Department of Pediatric Rheumatology in Hacettepe University, Ankara, Turkey, between February 2016 and March 2021. Inclusion criteria were: (1) children younger than 18 years of age, (2) all new patients with a confirmed rheumatic disease diagnosis within the aforementioned time periods. If the diagnosis was not confirmed, the patient was excluded. Agreed-upon classification criteria were used for the diagnosis of pediatric rheumatic diseases. All MIS-C patients met the criteria suggested by the Center for Disease Control (CDC) and the WHO clinical case definition criteria [19, 20]. All patients were evaluated and diagnosed by our pediatric rheumatology team. The inpatient data, such as macrophage activation syndrome (MAS) and multisystem inflammatory syndrome in children (MIS-C), were also reviewed. Patients who were followed up with a provisional diagnosis of rheumatic disease were excluded. The demographic features of the patients were assessed. Patients with concomitant rheumatic diagnoses such as familial Mediterranean fever (FMF) and IgA vasculitis (IgAV) were included in both diagnostic categories. Patients were divided into two groups according to the year of diagnosis (February 2016 to February 2020; and March 2020 to February 2021). The COVID-19 pandemic period was designated as between March 2020 and February 2021. The mean number per year was calculated for the newly diagnosed patients in the pre-pandemic 4-year period (2016–2020) compared with the number of patients diagnosed in the pandemic era (2020–2021).
Statistical analysis
Statistical analyses were performed using the SPSS version 20.0 package program. Descriptive statistics were presented as frequency, percentage, mean, and standard deviation (SD). The variables were investigated using visual (histograms, probability plots) and analytical methods (Kolmogorov–Smirnov/ Shapiro–Wilk’s test) to determine whether they are normally distributed. The Mann–Whitney U test was used to test age differences. The chi-square test was used to compare the frequencies of newly diagnosed patients in the pre-pandemic and pandemic period. For diseases in which a significant difference was found in chi-square analysis, the logistic regression model was used to estimate the effect of pandemic on the frequency of newly diagnosed patients with rheumatic disease. The odds ratios (ORs) and 95% confidence intervals (CIs) were calculated by logistic regression analysis by selecting the reference year 2020–2021. A p value of less than 0.05 was considered to show a statistically significant result.
Results
A total of 32,333 patients presented to our pediatric rheumatology department between February 2016 and March 2021. The annual distribution of patients according to the years was demonstrated in Fig. 1. The total number of patients during the COVID-19 pandemic year was lower than the annual numbers in the previous years (Fig. 1). The annual mean number of patients decreased by 42% during the pandemic period (7060 patients/year vs. 4090 patients/pandemic year).
25,156 out of 32,333 (77.8%) were recurrent visits. After excluding the recurrent visits, 7177 pediatric patients (3679 female, 51.2%) with a mean age of 8.64 ± 4.84 years were included in the study.
In the 5-year period between 2016 and 2021, a total of 2717 patients were diagnosed with 2818 new diagnoses of rheumatic diseases. During the COVID-19 pandemic period, 345 patients were newly diagnosed with 353 rheumatic diseases. There was no significant difference regarding the age and gender distributions of the newly diagnosed patients between the pre-pandemic and pandemic eras (p = 0.206 and p = 0.963, respectively).
During these 5 years (2016–2021), the most commonly diagnosed rheumatic disease was FMF in 750 patients (26.6%), followed by IgAV in 406 (14.4%) and juvenile idiopathic arthritis (JIA) in 383 (13.5%) patients (Supplementary Table 1). In the pre-pandemic period that was studied (2016–2020), the top three most frequently diagnosed rheumatic diseases were FMF (n = 695, 28.1%), IgAV (n = 380, 15.4%), and JIA (n = 343, 13.9%). In the pandemic period, MIS-C (n = 68, 19.2%), FMF (n = 55, 15.5%), and periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis (PFAPA) syndrome (n = 45, 12.7%) were the most commonly diagnosed rheumatic diseases.
There were significant differences regarding the annual numbers of newly diagnosed patients with FMF, IgAV, Kawasaki disease (KD), MAS, MIS-C, acute rheumatic fever (ARF), and chronic non-bacterial osteomyelitis (CNO) (Fig. 2). The presence of the COVID-19 pandemic was negatively associated with the frequency of newly diagnosed patients with FMF, IgAV, KD, and ARF (odds ratios (OR) = 1.8; 95% (confidence intervals) CI = 1.3–2.4, OR = 2.0; 95% CI = 1.3–3.2, OR = 4.7; 95% CI = 1.1–20.7, and OR = 6.0; 95% CI = 1.4–25.8, respectively) (Table 1). There were no cases of MAS during the pandemic year. The diagnosis of MIS-C is present only in the pandemic period since it is a COVID-19 associated disease. Of note, 36 out of 68 MIS-C patients (52.9%) had Kawasaki-like features (conjunctival injection, cervical lymphadenopathy, skin rash, changes in extremities, and oral mucosal involvement), whereas only two patients were diagnosed with (classic) KD after March 2020. On the other hand, there was a significant increase in newly diagnosed CNO patients (p = 0.003).
Discussion
This is the first study addressing the COVID-19 pandemic effect on the frequency of newly diagnosed patients in pediatric rheumatology. In this study, we retrospectively assessed the prevalence of rheumatic diseases over a 5-year period in a tertiary referral center in Turkey and demonstrated significant decreases in the numbers of newly diagnosed patients with IgAV, KD, MAS, ARF, and FMF during the COVID-19 pandemic year, compared to previous four years.
During the COVID-19 period, many measures have been implemented, including the use of masks, social distancing, travel restrictions, quarantine practices, and curfews. As a result of a meta-analysis, it was found that the use of masks had a significant protective effect not only for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), but also for influenza viruses and SARS [21]. As a result of all these measures, the transmission of other infectious agents has also been largely prevented, as stated by Soo et al. [12]. This may have led to a decrease in the prevalence of some rheumatic diseases, which are triggered or associated with infections, as well.
In our study, we showed that clinic visits decreased by approximately 40% during the COVID-19 period. In a study evaluating pediatric hospital admissions in 2020 compared with the prior decade, including 49 United States hospitals, it was reported that the admissions decreased by 45.4% in April 2020 compared to the previous years [22]. During the COVID-19 pandemic, a 32% reduction in hospital admissions through emergency services was also reported [23].
The most frequent disease in the pediatric rheumatology departments of Turkey has always been FMF, since the prevalence rate is at least 1/1073 [24]. However, in the pandemic period, the number of new admissions of FMF has drastically decreased, while MIS-C was the most common disease in the pandemic period. Our department serves as a referral center in pediatric rheumatology and we used to get a large number of cases for second opinion and confirmation (due to inconclusive genetic data) in autoinflammatory diseases including FMF. The reason for the decrease in FMF may be because of the lower referral from other centers and the decrease in hospital visits during the pandemic [25]. On the other hand, the percentages of other common diseases such as JIA, autoimmune diseases, and other rare autoinflammatory diseases, albeit scarce, have not changed.
The most frequent pediatric rheumatic disease over the world is JIA: chronic arthritis (23.3%) constituted the most frequent group in the registry of the Canadian Association of Pediatric Rheumatology [26]. In a prospective multicenter study conducted at pediatric rheumatology centers in southern New England, the most common rheumatic disease was juvenile idiopathic arthritis (53%) [27] similar to the reports from other Western countries [28,29,30]. JIA has been the second most frequent disease in our pediatric rheumatology practice. In the pandemic period, JIA moved to become the third common disease to be diagnosed because of the increasing cases with MIS-C.
In the pandemic period, the number of newly diagnosed IgAV patients significantly decreased as well. Preceding infections, especially upper respiratory tract infections, are reported in approximately 50% of children with IgAV [31, 32]. Thus, the decrease in the frequency of upper respiratory tract infections other than COVID-19 due to pandemic restrictions could be the primary reason for the decrease in the diagnostic rate of IgAV. The same could be true for ARF since it is associated with group A streptococcal infections.
Similar to IgAV, KD has also decreased in the last year. Several microbes are capable of producing superantigens which cause excessive activation of the immune system. Superantigens have been implicated in the pathogenesis of Kawasaki disease [33, 34]. The prevalence of classic KD decreased during the pandemic period probably due to protective measures and reduced transmission. On the other hand, the accompanying features of “Kawasaki-like” disease and toxic shock syndrome in MIS-C patients have raised the question of whether the superantigen-mediated response has a role in the pathogenesis. Porritt et al. reported the immune system activation in MIS-C patients related to the superantigenic immune response [35]. The presence of ''Kawasaki-like disease'' in approximately half of the MIS-C patients in our study might support this hypothesis.
Infection diseases are known to induce MAS attacks. In a multicenter study from 33 countries, 34.1% of the MAS patients were triggered by an infection agent [36]. In another study, infections were reported in seven of 12 MAS patients (58.3%), indicating the importance of the triggering role of infections in the development of MAS [37]. In our study, we observed a significant decrease in the prevalence of MAS in the pandemic period, excluding the clinical features of MIS-C patients similar to MAS. It is thus tempting to speculate that infections are important triggers in MAS and therefore, they were decreased to the decrease of common infections due to the restrictions imposed during the pandemic.
The rate of diagnosis of CNO has increased during the last year, possibly due to our increased awareness and an ongoing project for CNO. This project has led the orthopedic surgeons and other centers to refer their CNO patients to our department.
This study has some limitations. It is a retrospective study. And, our results may not reflect the distribution of pediatric rheumatic disease in general population since this is a single-center study. A point of concern is that a certain portion of the decrease of frequency of some specific diagnoses may be attributed to a decrease for the referral rate and/or that some diseases with less severe expression, may have been overlooked. Furthermore, long-term follow-up of these patients might be more appropriate to reveal the actual changes in the prevalence of the rheumatic diseases. Despite these limitations, ours is the first study evaluating the results of COVID-19 pandemic on rheumatic disease prevalence. We believe that this study would provide valuable information about the effect of preventing the spread of infections on rheumatic diseases and shed light on the pathogenesis of some rheumatic diseases.
Conclusion
During the COVID-19 period, the overall number of outpatients has decreased, and MIS-C has become the most frequent cause of admission. We suggest that the significant decrease in ARF, IgAV, classic KD and MAS is indirect evidence for the role of pathogens in the pathogenesis and/or triggers for these diseases.
References
Wu Y-C, Chen C-S, Chan Y-J (2020) The outbreak of COVID-19: an overview. J Chin Med Assoc 83:217. https://doi.org/10.1097/JCMA.0000000000000270
WHO (2020a) Director General’s Opening Remarks at the Media Briefing on COVID19 on 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
American Academy of Pediatrics (2021) Children and COVID-19: State Data Report, A joint report from the American Academy of Pediatrics and the Children’s Hospital Association. Version: 23 September 2021. https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/
World Health Organization (2020) Turkey: WHO Coronavirus disease (COVID-19) dashboard. https://covid19.who.int/region/euro/country/tr
Wang Z, Zhou Q, Wang C, Shi Q, Lu S, Ma Y et al (2020) Clinical characteristics of children with COVID-19: a rapid review and meta-analysis. Ann Transl Med 8: 620. https://doi.org/10.21037/atm-20-3302
Alessandro M, Elisabetta R, Chiara Z, Giorgia B, Marco DS, Andrea D (2021) Coronavirus Disease 2019 (COVID-19) in children and/or adolescents: a meta-analysis. Pediatr Res 89:733–737. https://doi.org/10.1038/s41390-020-1015-2
Kaushik S, Aydin SI, Derespina KR, Bansal PB, Kowalsky S, Trachtman R et al (2020) Multisystem inflammatory syndrome in children associated with severe acute respiratory syndrome coronavirus 2 infection (MIS-C): a multi-institutional study from New York City. J Pediatr 224:24–29. https://doi.org/10.1016/j.jpeds.2020.06.045
Radia T, Williams N, Agrawal P, Harman K, Weale J, Cook J et al (2021) Multi-system inflammatory syndrome in children & adolescents (MIS-C): A systematic review of clinical features and presentation. Paediatr Respir Rev 38:51–57. https://doi.org/10.1016/j.prrv.2020.08.001
de Souza TH, Nadal JA, Nogueira RJ, Pereira RM, Brandão MB (2020) Clinical manifestations of children with COVID-19: a systematic review. Pediatr pulmonol 55:1892–1899. https://doi.org/10.1002/ppul.24885
Viner RM, Ward JL, Hudson LD, Ashe M, Patel SV, Hargreaves D et al (2021) Systematic review of reviews of symptoms and signs of COVID-19 in children and adolescents. Arch Dis Child 106:802–807. https://doi.org/10.1136/archdischild-2020-320972
Yasuhara J, Kuno T, Takagi H, Sumitomo N (2020) Clinical characteristics of COVID-19 in children: a systematic review. Pediatr Pulmonol 55:2565–2575. https://doi.org/10.1002/ppul.24991
Soo RJJ, Chiew CJ, Ma S, Pung R, Lee V (2020) Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg Infect Dis 26:1933. https://doi.org/10.3201/eid2608.201229
Tan J, Conceicao E, Sim X, Wee L, Aung M, Venkatachalam I (2020) Public health measures during COVID-19 pandemic reduced hospital admissions for community respiratory viral infections. J Hosp Infect 106:387–389. https://doi.org/10.1016/j.jhin.2020.07.023
Amital H, Govoni M, Maya R, Meroni PL, Ori B, Shoenfeld Y et al (2008) Role of infectious agents in systemic rheumatic diseases. Clin Exp Rheumatol 26:27–32
Cusick MF, Libbey JE, Fujinami RS (2012) Molecular mimicry as a mechanism of autoimmune disease. Clin Rev Allergy Immunol 42:102–111. https://doi.org/10.1007/s12016-011-8294-7
Segal BH, Sneller MC (1997) Infectious complications of immunosuppressive therapy in patients with rheumatic diseases. Rheum Dis Clin North Am 23:219–237. https://doi.org/10.1016/s0889-857x(05)70327-6
Ciurea A, Papagiannoulis E, Bürki K, Von Loga I, Micheroli R, Möller B et al (2021) Impact of the COVID-19 pandemic on the disease course of patients with inflammatory rheumatic diseases: results from the Swiss clinical quality management cohort. Ann Rheum Dis 80:238–241. https://doi.org/10.1136/annrheumdis-2020-218705
Wahezi DM, Lo MS, Rubinstein TB, Ringold S, Ardoin SP, Downes KJ et al (2020) American College of Rheumatology Guidance for the Management of Pediatric Rheumatic Disease During the COVID-19 Pandemic: Version 1. Arthritis Rheumatol 72:1809–1819. https://doi.org/10.1002/art.41455
Centers for Disease Control and Prevention. Multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease 2019 (COVID-19). https://emergency.cdc.gov/han/2020/han00432.asp. 14 May 2020
World Health Organization (2020) Multisystem inflammatory syndrome in children and adolescents with COVID-19: scientific brief. https://www.who.int/publications-detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19. Accessed 30 Aug 2020.
Liang M, Gao L, Cheng C, Zhou Q, Uy JP, Heiner K et al (2020) Efficacy of face mask in preventing respiratory virus transmission: a systematic review and meta-analysis. Travel Med Infect Dis 36:101751. https://doi.org/10.1016/j.tmaid.2020.101751
Pelletier JH, Rakkar J, Au AK, Fuhrman D, Clark RS, Horvat CM (2021) Trends in US pediatric hospital admissions in 2020 compared with the decade before the COVID-19 pandemic. JAMA Netw Open 4:e2037227–e2037227. https://doi.org/10.1001/jamanetworkopen.2020.37227
Nourazari S, Davis SR, Granovsky R, Austin R, Straff DJ, Joseph JW et al (2021) Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med 42:203–210. https://doi.org/10.1016/j.ajem.2020.11.029
Cobankara V, Fidan G, Turk T, Zencir M, Colakoglu M, Ozen S (2004) The prevalence of familial Mediterranean fever in the Turkish province of Denizli: a field study with a zero patient design. Clin Exp Rheumatol 22:27-S30
Portincasa P, Scaccianoce G, Palasciano G (2013) Familial mediterranean fever: a fascinating model of inherited autoinflammatory disorder. Eur J Clin Invest 43:1314–1327. https://doi.org/10.1111/eci.12170
Malleson P, Fung M, Rosenberg A (1996) The incidence of pediatric rheumatic diseases: results from the Canadian Pediatric Rheumatology Association Disease Registry. J Rheumatol 23:1981–1987
Denardo B, Tucker L, Miller L, Szer I, Schaller J (1994) Demography of a regional pediatric rheumatology patient population. Affiliated Children’s Arthritis Centers of New England. J Rheumatol 21:1553–1561
Symmons D, Jones M, Osborne J, Sills J, Southwood T, Woo P (1996) Pediatric rheumatology in the United Kingdom: data from the British Pediatric Rheumatology Group National Diagnostic Register. J Rheumatol 23:1975–1980
Bowyer S, Roettcher P (1996) Pediatric rheumatology clinic populations in the United States: results of a 3 year survey. Pediatric Rheumatology Database Research Group. J Rheumatol 23:1968–1974
Huemer C, Huemer M, Dorner T, Falger J, Schacherl H, Bernecker M et al (2001) Incidence of pediatric rheumatic diseases in a regional population in Austria. J Rheumatol 28:2116–2119
Gökçe Ş, Dörtkardeşler BE, Aslan A (2021) Demographic, epidemiologic and clinical analyses of paediatric patients hospitalized with Henoch-Schonlein Purpura: a retrospective study. J Pediatr Res 8:35–41. https://doi.org/10.4274/jpr.galenos.2020.93695
Carapetis JR, McDonald M, Wilson NJ (2005) Acute rheumatic fever. Lancet 366:155–168. https://doi.org/10.1016/S0140-6736(18)30999-1
Leung DY, Schlievert PM (2021) Kawasaki syndrome: role of superantigens revisited. FEBS J 288:1771–1777. https://doi.org/10.1111/febs.15512
Yeung RS (2004) The etiology of Kawasaki disease: a superantigen-mediated process. Prog Pediatr Cardiol 19:115–122. https://doi.org/10.1016/j.ppedcard.2004.08.004
Porritt RA, Paschold L, Rivas MN, Cheng MH, Yonker LM, Chandnani H et al (2020) Identification of a unique TCR repertoire, consistent with a superantigen selection process in Children with Multi-system Inflammatory Syndrome. bioRxiv. https://doi.org/10.1101/2020.11.09.372169
Minoia F, Davì S, Horne A, Demirkaya E, Bovis F, Li C et al (2014) Clinical features, treatment, and outcome of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a multinational, multicenter study of 362 patients. Arthritis Rheumatol 66:3160–3169. https://doi.org/10.1002/art.38802
Miettunen PM, Narendran A, Jayanthan A, Behrens EM, Cron RQ (2011) Successful treatment of severe paediatric rheumatic disease-associated macrophage activation syndrome with interleukin-1 inhibition following conventional immunosuppressive therapy: case series with 12 patients. Rheumatology 50:417–419. https://doi.org/10.1093/rheumatology/keq218
Funding
No external funding for this manuscript. Financial disclosure: the authors have indicated they have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Contributions
All authors (SO, YB, EDB, OB, YO, UKA, EA, MKC, ZB, and SS) contributed to the study conception and design. Material preparation, data collection and analysis were performed by UKA, EA, MKC, ZB, SS, YO, OB, and EDB. The first draft of the manuscript was written by UKA and all authors (SO, YB, EDB, OB, YO, EA, MKC, ZB, and SS) reviewed the manuscript. All authors (SO, YB, EDB, OB, YO, UKA, EA, MKC, ZB, and SS) read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The other authors have indicated they have no potential conflicts of interest to disclose.
Ethics statement
This study has been approved by the Hacettepe University Ethics Commission (Approval Number: GO 21/670) and was conducted in accordance with the Declaration of Helsinki. Informed consent was not obtained from patients due to its retrospective nature.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kaya Akca, U., Atalay, E., Cuceoglu, M.K. et al. Impact of the COVID-19 pandemic on the frequency of the pediatric rheumatic diseases. Rheumatol Int 42, 51–57 (2022). https://doi.org/10.1007/s00296-021-05027-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-021-05027-7