Abstract
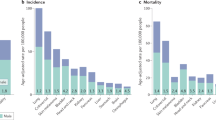
Cancer represents a leading cause of death with continuously increasing incidence worldwide. Many solid cancer types in non-reproductive organs are significantly more frequent and deadly in males compared to females. This sex-biased difference is also present in hematologic malignancies. In this review, we present an overview about sex differences in cancer with a focus on leukemia. We discuss mechanisms potentially underlying the observed sex-biased imbalance in cancer incidence and outcome including sex hormones, sex chromosomes, and immune responses. Besides affecting the pathobiology of cancers, sex differences can also influence drug responses, most notably those to immune checkpoint blockers. Therefore, sex should become a relevant factor in clinical trial design in order to avoid over- or under-treatment of one sex.

Similar content being viewed by others
References
Cronin KA, Ries LA, Edwards BK (2014) The Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute. Cancer 120(Suppl 23):3755–3757
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30
Collaborators, G.B.D.C.o.D et al (2017) Lancet 390(10100):1151–1210
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67(1):7–30
Ma X, Yu H (2006) Global burden of cancer. Yale J Biol Med 79(3–4):85–94
World Health Organization. http://www.who.int/news-room/fact-sheets/detail/cancer
Regitz-Zagrosek V (2012) Sex and gender differences in health. Science & Society Series on Sex and Science. EMBO Rep 13(7):596–603
Kim HI, Lim H, Moon A (2018) Sex differences in cancer: epidemiology, genetics and therapy. Biomol Ther (Seoul) 26(4):335–342
Cook MB, Dawsey SM, Freedman ND, Inskip PD, Wichner SM, Quraishi SM, Devesa SS, McGlynn KA (2009) Sex disparities in cancer incidence by period and age. Cancer Epidemiol Biomark Prev 18(4):1174–1182
Cook MB, McGlynn KA, Devesa SS, Freedman ND, Anderson WF (2011) Sex disparities in cancer mortality and survival. Cancer Epidemiol Biomark Prev 20(8):1629–1637
Edgren G, Liang L, Adami HO, Chang ET (2012) Enigmatic sex disparities in cancer incidence. Eur J Epidemiol 27(3):187–196
Scelo G et al (2017) Variability of sex disparities in cancer incidence over 30 years: the striking case of kidney cancer. Eur Urol Focus
Innos K, Padrik P, Valvere V, Aareleid T (2015) Sex differences in cancer survival in Estonia: a population-based study. BMC Cancer 15:72
Jung KW, Park S, Shin A, Oh CM, Kong HJ, Jun JK, Won YJ (2012) Do female cancer patients display better survival rates compared with males? Analysis of the Korean National Registry data, 2005-2009. PLoS One 7(12):e52457
Radkiewicz C, Johansson ALV, Dickman PW, Lambe M, Edgren G (2017) Sex differences in cancer risk and survival: a Swedish cohort study. Eur J Cancer 84:130–140
Dorak MT, Karpuzoglu E (2012) Gender differences in cancer susceptibility: an inadequately addressed issue. Front Genet 3:268
Bray F, Ferlay J, Laversanne M, Brewster DH, Gombe Mbalawa C, Kohler B, Piñeros M, Steliarova-Foucher E, Swaminathan R, Antoni S, Soerjomataram I, Forman D (2015) Cancer incidence in five continents: inclusion criteria, highlights from volume X and the global status of cancer registration. Int J Cancer 137(9):2060–2071
Torre LA, Siegel RL, Ward EM, Jemal A (2016) Global cancer incidence and mortality rates and trends--an update. Cancer Epidemiol Biomark Prev 25(1):16–27
Global Burden of Disease Cancer, C et al (2018) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol
Crocetti E, Mallone S, Robsahm TE, Gavin A, Agius D, Ardanaz E, Lopez MDC, Innos K, Minicozzi P, Borgognoni L, Pierannunzio D, Eisemann N, Hackl M, Zielonke N, Oberaigner W, van Eycken E, Henau K, Valerianova Z, Dimitrova N, Sekerija M, Zvolský M, Dušek L, Storm H, Engholm G, Mägi M, Aareleid T, Malila N, Seppä K, Velten M, Troussard X, Bouvier V, Launoy G, Guizard AV, Faivre J, Bouvier AM, Arveux P, Maynadié M, Woronoff AS, Robaszkiewicz M, Baldi I, Monnereau A, Tretarre B, Bossard N, Belot A, Colonna M, Molinié F, Bara S, Schvartz C, Lapôtre-Ledoux B, Grosclaude P, Meyer M, Stabenow R, Luttmann S, Eberle A, Brenner H, Nennecke A, Engel J, Schubert- Fritschle G, Kieschke J, Heidrich J, Holleczek B, Katalinic A, Jónasson JG, Tryggvadóttir L, Comber H, Mazzoleni G, Bulatko A, Buzzoni C, Giacomin A, Sutera Sardo A, Mancuso P, Ferretti S, Caldarella A, Manneschi G, Gatta G, Sant M, Amash H, Amati C, Baili P, Berrino F, Bonfarnuzzo S, Botta L, di Salvo F, Foschi R, Margutti C, Meneghini E, Minicozzi P, Trama A, Serraino D, Dal Maso L, de Angelis R, Caldora M, Capocaccia R, Carrani E, Francisci S, Mallone S, Pierannunzio D, Roazzi P, Rossi S, Santaquilani, Tavilla A, Pannozzo F, Natali M, Bonelli L, Vercelli M, Gennaro V, Ricci P, Autelitano M, Randi G, Ponz de Leon M, Marchesi C, Cirilli C, Fusco M, Vitale MF, Usala M, Traina A, Staiti R, Vitale F, Ravazzolo B, Michiara M, Tumino R, Giorgi Rossi P, di Felice E, Falcini F, Iannelli A, Sechi O, Cesaraccio R, Piffer S, Madeddu A, Tisano F, Maspero S, Fanetti AC, Zanetti R, Rosso S, Candela P, Scuderi T, Stracci F, Bianconi F, Tagliabue G, Contiero P, Dei Tos AP, Guzzinati S, Pildava S, Smailyte G, Calleja, Agius D, Johannesen TB, Rachtan J, Gózdz S, Mezyk R, Blaszczyk J, Bebenek M, Bielska-Lasota M, Forjaz de Lacerda G, Bento MJ, Castro C, Miranda A, Mayer-da-Silva A, Nicula F, Coza D, Safaei Diba C, Primic-Zakelj M, Almar E, Ramírez C, Errezola M, Bidaurrazaga J, Torrella-Ramos A, Díaz García JM, Jimenez-Chillaron R, Marcos-Gragera R, Izquierdo Font A, Sanchez MJ, Chang DYL, Navarro C, Chirlaque MD, Moreno-Iribas C, Ardanaz E, Galceran J, Carulla M, Lambe M, Khan S, Mousavi M, Bouchardy C, Usel M, Ess SM, Frick H, Lorez M, Ess SM, Herrmann C, Bordoni A, Spitale A, Konzelmann I, Visser O, Lemmens V, Coleman M, Allemani C, Rachet B, Verne J, Easey N, Lawrence G, Moran T, Rashbass J, Roche M, Wilkinson J, Gavin A, Donnelly C, Brewster DH, Huws DW, White C, Otter R (2015) Survival of patients with skin melanoma in Europe increases further: results of the EUROCARE-5 study. Eur J Cancer 51(15):2179–2190
Rahbari R, Zhang L, Kebebew E (2010) Thyroid cancer gender disparity. Future Oncol 6(11):1771–1779
Lortet-Tieulent J, Renteria E, Sharp L, Weiderpass E, Comber H, Baas P, Bray F, Coebergh JW, Soerjomataram I (2015) Convergence of decreasing male and increasing female incidence rates in major tobacco-related cancers in Europe in 1988-2010. Eur J Cancer 51(9):1144–1163
McCartney G, Mahmood L, Leyland AH, Batty GD, Hunt K (2011) Contribution of smoking-related and alcohol-related deaths to the gender gap in mortality: evidence from 30 European countries. Tob Control 20(2):166–168
Karami S, Colt JS, Stewart PA, Schwartz K, Davis FG, Ruterbusch JJ, Chow WH, Wacholder S, Graubard BI, Purdue MP, Moore LE (2016) A case-control study of occupational sunlight exposure and renal cancer risk. Int J Cancer 138(7):1626–1633
Liu-Smith F, Farhat AM, Arce A, Ziogas A, Taylor T, Wang Z, Yourk V, Liu J, Wu J, McEligot AJ, Anton-Culver H, Meyskens FL (2017) Sex differences in the association of cutaneous melanoma incidence rates and geographic ultraviolet light exposure. J Am Acad Dermatol 76(3):499–505 e3
Anand P, Kunnumakara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, Sung B, Aggarwal BB (2008) Cancer is a preventable disease that requires major lifestyle changes. Pharm Res 25(9):2097–2116
Zahm SH, Fraumeni JF Jr (1995) Racial, ethnic, and gender variations in cancer risk: considerations for future epidemiologic research. Environ Health Perspect 103(Suppl 8):283–286
Clocchiatti A, Cora E, Zhang Y, Dotto GP (2016) Sexual dimorphism in cancer. Nat Rev Cancer 16(5):330–339
Wang M, Wu X, Chai F, Zhang Y, Jiang J (2016) Plasma prolactin and breast cancer risk: a meta- analysis. Sci Rep 6:25998
Wennbo H, Tornell J (2000) The role of prolactin and growth hormone in breast cancer. Oncogene 19(8):1072–1076
Jacobson EM, Hugo ER, Borcherding DC, Ben-Jonathan N (2011) Prolactin in breast and prostate cancer: molecular and genetic perspectives. Discov Med 11(59):315–324
Silva EG, Mistry D, Li D, Kuerer HM, Atkinson EN, Lopez AN, Shannon R, Hortobagyi GN (2002) Elevated luteinizing hormone in serum, breast cancer tissue, and normal breast tissue from breast cancer patients. Breast Cancer Res Treat 76(2):125–130
Dabizzi S, Noci I, Borri P, Borrani E, Giachi M, Balzi M, Taddei GL, Marchionni M, Scarselli GF, Arcangeli A (2003) Luteinizing hormone increases human endometrial cancer cells invasiveness through activation of protein kinase A. Cancer Res 63(14):4281–4286
Arslan AA et al (2003) Serum follicle-stimulating hormone and risk of epithelial ovarian cancer in postmenopausal women. Cancer Epidemiol Biomark Prev 12(12):1531–1535
Wanderas EH et al (1990) Serum follicle stimulating hormone--predictor of cancer in the remaining testis in patients with unilateral testicular cancer. Br J Urol 66(3):315–317
Zhou J et al (2013) Serum follicle-stimulating hormone level is associated with human epidermal growth factor receptor type 2 and Ki67 expression in post-menopausal females with breast cancer. Oncol Lett 6(4):1128–1132
Mertens-Walker I, Baxter RC, Marsh DJ (2012) Gonadotropin signalling in epithelial ovarian cancer. Cancer Lett 324(2):152–159
Debruyne FM (2004) Gonadotropin-releasing hormone antagonist in the management of prostate cancer. Rev Urol 6(Suppl 7):S25–S32
Yamamoto R, Iishi H, Tatsuta M, Yamamoto T, Koike K, Kanda Y, Miyake A, Tsuji M, Terada N (1995) Correlation between serum prolactin levels and hepatocellular tumorigenesis induced by 3′-methyl-4-dimethylaminoazobenzene in mice. Br J Cancer 72(1):17–21
Handler MZ, Ross AL, Shiman MI, Elgart GW, Grichnik JM (2012) Potential role of human growth hormone in melanoma growth promotion. Arch Dermatol 148(10):1179–1182
Lea RW, Dawson T, Martinez-Moreno CG, el-Abry N, Harvey S (2015) Growth hormone and cancer: GH production and action in glioma? Gen Comp Endocrinol 220:119–123
Farzaneh S, Zarghi A (2016) Estrogen receptor ligands: a review (2013-2015). Sci Pharm 84(3):409–427
Lu NZ, Wardell SE, Burnstein KL, Defranco D, Fuller PJ, Giguere V, Hochberg RB, McKay L, Renoir JM, Weigel NL, Wilson EM, McDonnell DP, Cidlowski JA (2006) International Union of Pharmacology. LXV. The pharmacology and classification of the nuclear receptor superfamily: glucocorticoid, mineralocorticoid, progesterone, and androgen receptors. Pharmacol Rev 58(4):782–797
Vannucchi G, de Leo S, Perrino M, Rossi S, Tosi D, Cirello V, Colombo C, Bulfamante G, Vicentini L, Fugazzola L (2015) Impact of estrogen and progesterone receptor expression on the clinical and molecular features of papillary thyroid cancer. Eur J Endocrinol 173(1):29–36
Skjefstad K, Richardsen E, Donnem T, Andersen S, Kiselev Y, Grindstad T, Hald SM, al-Shibli K, Bremnes RM, Busund LT, al-Saad S (2015) The prognostic role of progesterone receptor expression in non-small cell lung cancer patients: gender-related impacts and correlation with disease-specific survival. Steroids 98:29–36
Simon MS, Chlebowski RT, Wactawski-Wende J, Johnson KC, Muskovitz A, Kato I, Young A, Hubbell FA, Prentice RL (2012) Estrogen plus progestin and colorectal cancer incidence and mortality. J Clin Oncol 30(32):3983–3990
Naugler WE, Sakurai T, Kim S, Maeda S, Kim K, Elsharkawy AM, Karin M (2007) Gender disparity in liver cancer due to sex differences in MyD88-dependent IL-6 production. Science 317(5834):121–124
Yeh SH, Chen PJ (2010) Gender disparity of hepatocellular carcinoma: the roles of sex hormones. Oncology 78(Suppl 1):172–179
Li Z, Tuteja G, Schug J, Kaestner KH (2012) Foxa1 and Foxa2 are essential for sexual dimorphism in liver cancer. Cell 148(1–2):72–83
Keng VW, Largaespada DA, Villanueva A (2012) Why men are at higher risk for hepatocellular carcinoma? J Hepatol 57(2):453–454
McMichael AJ, Potter JD (1980) Reproduction, endogenous and exogenous sex hormones, and colon cancer: a review and hypothesis. J Natl Cancer Inst 65(6):1201–1207
Farhana L, Nangia-Makker P, Arbit E, Shango K, Sarkar S, Mahmud H, Hadden T, Yu Y, Majumdar APN (2016) Bile acid: a potential inducer of colon cancer stem cells. Stem Cell Res Ther 7(1):181
Lawrence T, Hageman T, Balkwill F (2007) Cancer. Sex, cytokines, and cancer. Science 317(5834):51–52
Yu CP, Ho JY, Huang YT, Cha TL, Sun GH, Yu DS, Chang FW, Chen SP, Hsu RJ (2013) Estrogen inhibits renal cell carcinoma cell progression through estrogen receptor-beta activation. PLoS One 8(2):e56667
Passarelli MN, Phipps AI, Potter JD, Makar KW, Coghill AE, Wernli KJ, White E, Chan AT, Hutter CM, Peters U, Newcomb PA (2013) Common single-nucleotide polymorphisms in the estrogen receptor beta promoter are associated with colorectal cancer survival in postmenopausal women. Cancer Res 73(2):767–775
Stanley JA, Aruldhas MM, Chandrasekaran M, Neelamohan R, Suthagar E, Annapoorna K, Sharmila S, Jayakumar J, Jayaraman G, Srinivasan N, Banu SK (2012) Androgen receptor expression in human thyroid cancer tissues: a potential mechanism underlying the gender bias in the incidence of thyroid cancers. J Steroid Biochem Mol Biol 130(1–2):105–124
Lee ML, Chen GG, Vlantis AC, Tse GMK, Leung BCH, van Hasselt CA (2005) Induction of thyroid papillary carcinoma cell proliferation by estrogen is associated with an altered expression of Bcl-xL. Cancer J 11(2):113–121
Pearce MS, Parker L (2001) Childhood cancer registrations in the developing world: still more boys than girls. Int J Cancer 91(3):402–406
Wan TS (2014) Cancer cytogenetics: methodology revisited. Ann Lab Med 34(6):413–425
Slavney A, Arbiza L, Clark AG, Keinan A (2016) Strong constraint on human genes escaping X-inactivation is modulated by their expression level and breadth in both sexes. Mol Biol Evol 33(2):384–393
Carrel L, Willard HF (2005) X-inactivation profile reveals extensive variability in X-linked gene expression in females. Nature 434(7031):400–404
Minajigi A, Froberg JE, Wei C, Sunwoo H, Kesner B, Colognori D, Lessing D, Payer B, Boukhali M, Haas W, Lee JT (2015) Chromosomes. A comprehensive Xist interactome reveals cohesin repulsion and an RNA-directed chromosome conformation. Science 349(6245):aab2276
Bellott DW, Hughes JF, Skaletsky H, Brown LG, Pyntikova T, Cho TJ, Koutseva N, Zaghlul S, Graves T, Rock S, Kremitzki C, Fulton RS, Dugan S, Ding Y, Morton D, Khan Z, Lewis L, Buhay C, Wang Q, Watt J, Holder M, Lee S, Nazareth L, Alföldi J, Rozen S, Muzny DM, Warren WC, Gibbs RA, Wilson RK, Page DC (2014) Mammalian Y chromosomes retain widely expressed dosage-sensitive regulators. Nature 508(7497):494–499
Walport LJ, Hopkinson RJ, Vollmar M, Madden SK, Gileadi C, Oppermann U, Schofield CJ, Johansson C (2014) Human UTY(KDM6C) is a male-specific N-methyl lysyl demethylase. J Biol Chem 289(26):18302–18313
van Haaften G, Dalgliesh GL, Davies H, Chen L, Bignell G, Greenman C, Edkins S, Hardy C, O'Meara S, Teague J, Butler A, Hinton J, Latimer C, Andrews J, Barthorpe S, Beare D, Buck G, Campbell PJ, Cole J, Forbes S, Jia M, Jones D, Kok CY, Leroy C, Lin ML, McBride DJ, Maddison M, Maquire S, McLay K, Menzies A, Mironenko T, Mulderrig L, Mudie L, Pleasance E, Shepherd R, Smith R, Stebbings L, Stephens P, Tang G, Tarpey PS, Turner R, Turrell K, Varian J, West S, Widaa S, Wray P, Collins VP, Ichimura K, Law S, Wong J, Yuen ST, Leung SY, Tonon G, DePinho RA, Tai YT, Anderson KC, Kahnoski RJ, Massie A, Khoo SK, Teh BT, Stratton MR, Futreal PA (2009) Somatic mutations of the histone H3K27 demethylase gene UTX in human cancer. Nat Genet 41(5):521–523
Dalgliesh GL, Furge K, Greenman C, Chen L, Bignell G, Butler A, Davies H, Edkins S, Hardy C, Latimer C, Teague J, Andrews J, Barthorpe S, Beare D, Buck G, Campbell PJ, Forbes S, Jia M, Jones D, Knott H, Kok CY, Lau KW, Leroy C, Lin ML, McBride DJ, Maddison M, Maguire S, McLay K, Menzies A, Mironenko T, Mulderrig L, Mudie L, O’Meara S, Pleasance E, Rajasingham A, Shepherd R, Smith R, Stebbings L, Stephens P, Tang G, Tarpey PS, Turrell K, Dykema KJ, Khoo SK, Petillo D, Wondergem B, Anema J, Kahnoski RJ, Teh BT, Stratton MR, Futreal PA (2010) Systematic sequencing of renal carcinoma reveals inactivation of histone modifying genes. Nature 463(7279):360–363
Shriver SP, Bourdeau HA, Gubish CT, Tirpak DL, Davis ALG, Luketich JD, Siegfried JM (2000) Sex-specific expression of gastrin-releasing peptide receptor: relationship to smoking history and risk of lung cancer. J Natl Cancer Inst 92(1):24–33
Hewagama A, Gorelik G, Patel D, Liyanarachchi P, Joseph McCune W, Somers E, Gonzalez-Rivera T, The Michigan Lupus Cohort, Strickland F, Richardson B (2013) Overexpression of X-linked genes in T cells from women with lupus. J Autoimmun 41:60–71
le Sage C, Nagel R, Egan DA, Schrier M, Mesman E, Mangiola A, Anile C, Maira G, Mercatelli N, Ciafrè SA, Farace MG, Agami R (2007) Regulation of the p27(Kip1) tumor suppressor by miR-221 and miR-222 promotes cancer cell proliferation. EMBO J 26(15):3699–3708
Wallrapp C, Hähnel S, Boeck W, Soder A, Mincheva A, Lichter P, Leder G, Gansauge F, Sorio C, Scarpa A, Gress TM (2001) Loss of the Y chromosome is a frequent chromosomal imbalance in pancreatic cancer and allows differentiation to chronic pancreatitis. Int J Cancer 91(3):340–344
Noveski P, Madjunkova S, Sukarova Stefanovska E, Matevska Geshkovska N, Kuzmanovska M, Dimovski A, Plaseska-Karanfilska D (2016) Loss of Y chromosome in peripheral blood of colorectal and prostate cancer patients. PLoS One 11(1):e0146264
Minner S, Kilgué A, Stahl P, Weikert S, Rink M, Dahlem R, Fisch M, Höppner W, Wagner W, Bokemeyer C, Terracciano L, Simon R, Sauter G, Wilczak W (2010) Y chromosome loss is a frequent early event in urothelial bladder cancer. Pathology 42(4):356–359
Kido T, Lau YF (2015) Roles of the Y chromosome genes in human cancers. Asian J Androl 17(3):373–380
Murakami S, Chishima S, Uemoto H, Sakamoto E, Sato T, Kurabe N, Kawasaki Y, Shibata T, Akiyama H, Tashiro F (2014) The male-specific factor Sry harbors an oncogenic function. Oncogene 33(23):2978–2986
Kido T, Lo RCL, Li Y, Lee J, Tabatabai ZL, Ng IOL, Lau YFC (2014) The potential contributions of a Y-located protooncogene and its X homologue in sexual dimorphisms in hepatocellular carcinoma. Hum Pathol 45(9):1847–1858
Delbridge ML, Longepied G, Depetris D, Mattei MG, Disteche CM, Marshall Graves JA, Mitchell MJ (2004) TSPY, the candidate gonadoblastoma gene on the human Y chromosome, has a widely expressed homologue on the X - implications for Y chromosome evolution. Chromosom Res 12(4):345–356
Ali RH et al (2014) Gender-associated genomic differences in colorectal cancer: clinical insight from feminization of male cancer cells. Int J Mol Sci 15(10):17344–17365
Zheng L, Wang Y, Schabath MB, Grossman HB, Wu X (2003) Sulfotransferase 1A1 (SULT1A1) polymorphism and bladder cancer risk: a case-control study. Cancer Lett 202(1):61–69
Mollerup S, Berge G, Bæra R, Skaug V, Hewer A, Phillips DH, Stangeland L, Haugen A (2006) Sex differences in risk of lung cancer: expression of genes in the PAH bioactivation pathway in relation to smoking and bulky DNA adducts. Int J Cancer 119(4):741–744
Hollstein M, Sidransky D, Vogelstein B, Harris C (1991) p53 mutations in human cancers. Science 253(5015):49–53
Kure EH, Ryberg D, Hewer A, Phillips DH, Skaug V, Bæera R, Haugen A (1996) p53 mutations in lung tumours: relationship to gender and lung DNA adduct levels. Carcinogenesis 17(10):2201–2205
Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, Sasaki H, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M (2004) EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304(5676):1497–1500
Yang SH, Mechanic LE, Yang P, Landi MT, Bowman ED, Wampfler J, Meerzaman D, Hong KM, Mann F, Dracheva T, Fukuoka J, Travis W, Caporaso NE, Harris CC, Jen J (2005) Mutations in the tyrosine kinase domain of the epidermal growth factor receptor in non-small cell lung cancer. Clin Cancer Res 11(6):2106–2110
Nelson HH, Christiani DC, Mark EJ, Wiencke JK, Wain JC, Kelsey KT (1999) Implications and prognostic value of K-ras mutation for early-stage lung cancer in women. J Natl Cancer Inst 91(23):2032–2038
Planchard D, Loriot Y, Goubar A, Commo F, Soria JC (2009) Differential expression of biomarkers in men and women. Semin Oncol 36(6):553–565
Zhang YL, Yuan JQ, Wang KF, Fu XH, Han XR, Threapleton D, Yang ZY, Mao C, Tang JL (2016) The prevalence of EGFR mutation in patients with non-small cell lung cancer: a systematic review and meta-analysis. Oncotarget 7(48):78985–78993
Cui G, Liu D, Li W, Fu X, Liang Y, Li Y, Shi W, Chen X, Zhao S (2017) A meta-analysis of the association between BRAF mutation and nonsmall cell lung cancer. Medicine (Baltimore) 96(14):e6552
Mohamad N, Jayalakshmi P, Rhodes A, Liam CK, Tan JL, Yousoof S, Rajadurai P (2017) Anaplastic lymphoma kinase (ALK) mutations in patients with adenocarcinoma of the lung. Br J Biomed Sci 74(4):176–180
Rossi G, Jocollé G, Conti A, Tiseo M, Zito Marino F, Donati G, Franco R, Bono F, Barbisan F, Facchinetti F (2017) Detection of ROS1 rearrangement in non-small cell lung cancer: current and future perspectives. Lung Cancer (Auckl) 8:45–55
Fullwood MJ, Liu MH, Pan YF, Liu J, Xu H, Mohamed YB, Orlov YL, Velkov S, Ho A, Mei PH, Chew EGY, Huang PYH, Welboren WJ, Han Y, Ooi HS, Ariyaratne PN, Vega VB, Luo Y, Tan PY, Choy PY, Wansa KDSA, Zhao B, Lim KS, Leow SC, Yow JS, Joseph R, Li H, Desai KV, Thomsen JS, Lee YK, Karuturi RKM, Herve T, Bourque G, Stunnenberg HG, Ruan X, Cacheux-Rataboul V, Sung WK, Liu ET, Wei CL, Cheung E, Ruan Y (2009) An oestrogen-receptor-alpha-bound human chromatin interactome. Nature 462(7269):58–64
Atala A (2015) Re: brain feminization requires active repression of masculinization via DNA methylation. J Urol 194(6):1823–1824
Boyne DJ, Friedenreich CM, McIntyre JB, Stanczyk FZ, Courneya KS, King WD (2017) Endogenous sex hormone exposure and repetitive element DNA methylation in healthy postmenopausal women. Cancer Causes Control 28(12):1369–1379
Sugathan A, Waxman DJ (2013) Genome-wide analysis of chromatin states reveals distinct mechanisms of sex-dependent gene regulation in male and female mouse liver. Mol Cell Biol 33(18):3594–3610
Wingelhofer B, Neubauer HA, Valent P, Han X, Constantinescu SN, Gunning PT, Müller M, Moriggl R (2018) Implications of STAT3 and STAT5 signaling on gene regulation and chromatin remodeling in hematopoietic cancer. Leukemia 32:1713–1726
Sarter B, Long TI, Tsong WH, Koh WP, Yu MC, Laird PW (2005) Sex differential in methylation patterns of selected genes in Singapore Chinese. Hum Genet 117(4):402–403
Vaissiere T, Hung RJ, Zaridze D, Moukeria A, Cuenin C, Fasolo V, Ferro G, Paliwal A, Hainaut P, Brennan P, Tost J, Boffetta P, Herceg Z (2009) Quantitative analysis of DNA methylation profiles in lung cancer identifies aberrant DNA methylation of specific genes and its association with gender and cancer risk factors. Cancer Res 69(1):243–252
Donninger H, Vos MD, Clark GJ (2007) The RASSF1A tumor suppressor. J Cell Sci 120(Pt 18):3163–3172
Gabory A, Attig L, Junien C (2009) Sexual dimorphism in environmental epigenetic programming. Mol Cell Endocrinol 304(1–2):8–18
Klein SL, Flanagan KL (2016) Sex differences in immune responses. Nat Rev Immunol 16(10):626–638
Fish EN (2008) The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol 8(9):737–744
Kato S, Sato T, Watanabe T, Takemasa S, Masuhiro Y, Ohtake F, Matsumoto T (2005) Function of nuclear sex hormone receptors in gene regulation. Cancer Chemother Pharmacol 56(Suppl 1):4–9
Heldring N, Pike A, Andersson S, Matthews J, Cheng G, Hartman J, Tujague M, Ström A, Treuter E, Warner M, Gustafsson JÅ (2007) Estrogen receptors: how do they signal and what are their targets. Physiol Rev 87(3):905–931
Kovats S (2015) Estrogen receptors regulate innate immune cells and signaling pathways. Cell Immunol 294(2):63–69
Buskiewicz IA, Huber SA, Fairweather D (2016) Sex hormone receptor expression in the immune system. Sex Differ Physiol
Sader MA, McGrath KCY, Hill MD, Bradstock KF, Jimenez M, Handelsman DJ, Celermajer DS, Death AK (2005) Androgen receptor gene expression in leucocytes is hormonally regulated: implications for gender differences in disease pathogenesis. Clin Endocrinol 62(1):56–63
Foo YZ, Nakagawa S, Rhodes G, Simmons LW (2017) The effects of sex hormones on immune function: a meta-analysis. Biol Rev Camb Philos Soc 92(1):551–571
Arango Duque G, Descoteaux A (2014) Macrophage cytokines: involvement in immunity and infectious diseases. Front Immunol 5:491
Gabriele L, Buoncervello M, Ascione B, Bellenghi M, Matarrese P, Carè A (2016) The gender perspective in cancer research and therapy: novel insights and on-going hypotheses. Ann Ist Super Sanita 52(2):213–222
Weinstein Y, Ran S, Segal S (1984) Sex-associated differences in the regulation of immune responses controlled by the MHC of the mouse. J Immunol 132(2):656–661
Roved J, Westerdahl H, Hasselquist D (2017) Sex differences in immune responses: hormonal effects, antagonistic selection, and evolutionary consequences. Horm Behav 88:95–105
Bhutia SK et al (2013) Autophagy: cancer’s friend or foe? Adv Cancer Res 118:61–95
Lista P, Straface E, Brunelleschi S, Franconi F, Malorni W (2011) On the role of autophagy in human diseases: a gender perspective. J Cell Mol Med 15(7):1443–1457
Barros RP, Gustafsson JA (2011) Estrogen receptors and the metabolic network. Cell Metab 14(3):289–299
Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB (2010) Oxidative stress, inflammation, and cancer: how are they linked? Free Radic Biol Med 49(11):1603–1616
Nosrati A, Wei ML (2014) Sex disparities in melanoma outcomes: the role of biology. Arch Biochem Biophys 563:42–50
Damian DL, Patterson CRS, Stapelberg M, Park J, Barnetson RSC, Halliday GM (2008) UV radiation-induced immunosuppression is greater in men and prevented by topical nicotinamide. J Investig Dermatol 128(2):447–454
Mearadji B, Penning C, Vu MK, van der Schaar PJ, van Petersen AS, Kamerling IMC, Masclee AAM (2001) Influence of gender on proximal gastric motor and sensory function. Am J Gastroenterol 96(7):2066–2073
Saif MW, Syrigos K, Mehra R, Mattison LK, Diasio RB (2007) Dihydropyrimidine dehydrogenase deficiency (Dpd) in Gi malignancies: experience of 4-years. Pak J Med Sci 23(6):832–839
Joerger M et al (2006) Quantitative effect of gender, age, liver function, and body size on the population pharmacokinetics of Paclitaxel in patients with solid tumors. Clin Cancer Res 12(7 Pt 1):2150–2157
Brahmer JR, Dahlberg SE, Gray RJ, Schiller JH, Perry MC, Sandler A, Johnson DH (2011) Sex differences in outcome with bevacizumab therapy: analysis of patients with advanced-stage non-small cell lung cancer treated with or without bevacizumab in combination with paclitaxel and carboplatin in the Eastern Cooperative Oncology Group Trial 4599. J Thorac Oncol 6(1):103–108
Janelsins MC, Tejani MA, Kamen C, Peoples AR, Mustian KM, Morrow GR (2013) Current pharmacotherapy for chemotherapy-induced nausea and vomiting in cancer patients. Expert Opin Pharmacother 14(6):757–766
Neves H, Kwok HF (2015) Recent advances in the field of anti-cancer immunotherapy. BBA Clin 3:280–288
Conforti F et al (2018) Sex as a predictor of response to cancer immunotherapy. Lancet Oncol 19(8):380–381
Wu Y, Ju Q, Jia K, Yu J, Shi H, Wu H, Jiang M (2018) Correlation between sex and efficacy of immune checkpoint inhibitors (PD-1 and CTLA-4 inhibitors). Int J Cancer 143(1):45–51
Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J, Lister TA, Bloomfield CD (2000) The World Health Organization classification of hematological malignancies report of the Clinical Advisory Committee Meeting, Airlie House, Virginia, November 1997. Mod Pathol 13(2):193–207
Derolf AR, Kristinsson SY, Andersson TML, Landgren O, Dickman PW, Bjorkholm M (2009) Improved patient survival for acute myeloid leukemia: a population-based study of 9729 patients diagnosed in Sweden between 1973 and 2005. Blood 113(16):3666–3672
Ober C, Loisel DA, Gilad Y (2008) Sex-specific genetic architecture of human disease. Nat Rev Genet 9(12):911–922
Cartwright RA, Gurney KA, Moorman AV (2002) Sex ratios and the risks of haematological malignancies. Br J Haematol 118(4):1071–1077
Hossain MJ, Xie L (2015) Sex disparity in childhood and young adult acute myeloid leukemia (AML) survival: evidence from US population data. Cancer Epidemiol 39(6):892–900
Canner J, Alonzo TA, Franklin J, Freyer DR, Gamis A, Gerbing RB, Lange BJ, Meshinchi S, Woods WG, Perentesis J, Horan J (2013) Differences in outcomes of newly diagnosed acute myeloid leukemia for adolescent/young adult and younger patients: a report from the Children’s Oncology Group. Cancer 119(23):4162–4169
Spitz MR, Sider JG, Johnson CC, Butler JJ, Pollack ES, Newell GR (1986) Ethnic patterns of Hodgkin’s disease incidence among children and adolescents in the United States, 1973-82. J Natl Cancer Inst 76(2):235–239
Radivoyevitch T, Jankovic GM, Tiu RV, Saunthararajah Y, Jackson RC, Hlatky LR, Gale RP, Sachs RK (2014) Sex differences in the incidence of chronic myeloid leukemia. Radiat Environ Biophys 53(1):55–63
Rosenberg PS, Wilson KL, Anderson WF (2012) Are incidence rates of adult leukemia in the United States significantly associated with birth cohort? Cancer Epidemiol Biomark Prev 21(12):2159–2166
Do TN, Ucisik-Akkaya E, Davis CF, Morrison BA, Dorak MT (2010) An intronic polymorphism of IRF4 gene influences gene transcription in vitro and shows a risk association with childhood acute lymphoblastic leukemia in males. Biochim Biophys Acta 1802(2):292–300
Shahrabi S, Khodadi E, Saba F, Shahjahani M, Saki N (2018) Sex chromosome changes in leukemia: cytogenetics and molecular aspects. Hematology 23(3):139–147
Bolufer P, Collado M, Barragan E, Cervera J, Calasanz MJ, Colomer D, Roman-Gomez J, Sanz MA (2007) The potential effect of gender in combination with common genetic polymorphisms of drug-metabolizing enzymes on the risk of developing acute leukemia. Haematologica 92(3):308–314
Acknowledgements
S.L. is supported by a Heisenberg professorship and by the Schwerpunktprogramm mbone from the DFG (LO1863-4/1, SL1863/5-1), by the Landesforschungsförderung Hamburg (consortium sexual dimorphism in the immune system) and by the Margarethe Clemens Stiftung. I.B.B. is supported by the Schwerpunktprogramm mbone from the DFG (BE6658/1-1) and by the Landesforschungsförderung Hamburg (consortium sexual dimorphism in the immune system). M.E.V.D. is supported by the Landesforschungsförderung Hamburg (consortium sexual dimorphism in the immune system).
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is a contribution to the special issue on Sex differences in immunity – Guest Editors: Hanna Lotter and Marcus Altfeld
Rights and permissions
About this article
Cite this article
Ben-Batalla, I., Vargas-Delgado, M.E., Meier, L. et al. Sexual dimorphism in solid and hematological malignancies. Semin Immunopathol 41, 251–263 (2019). https://doi.org/10.1007/s00281-018-0724-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-018-0724-7