Abstract
Background
Brain Trauma Foundation (BTF) guidelines recommend intracranial pressure (ICP) monitoring in patients who sustained severe traumatic brain injury (TBI). Compliance to BTF guidelines is variable, and the effect of ICP monitoring on outcomes remains a controversial issue. The purpose of this study was to assess guidelines compliance in patients who sustain a severe TBI and to analyze the effect of ICP monitoring on outcomes.
Methods
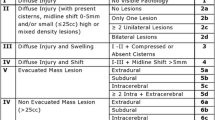
Trauma Quality Improvement Program database study, which included patients with isolated severe blunt head trauma (head Abbreviated Injury Scale ≥3 with Glasgow Coma Scale <9). Patients with severe extracranial injuries excluded. Analyzed variables were demographics, comorbidities, mechanism of injuries, head injury specifics, AIS for each body area, Injury Severity Score, admission vital signs, placement of ICP catheter and craniectomy. Multivariate analysis was used to identify independent predictors for outcomes, overall and in the groups of patients with head AIS 3, 4 or 5.
Results
During the study period 13,188 patients with isolated severe TBI met the BTF guidelines for ICP monitoring. An ICP catheter was placed in 1519 (11.5%) patients. Stepwise logistic regression analysis identified age ≥65 years, hypotension on admission, AIS 4 and AIS 5 as independent predictors for mortality. ICP monitoring was not an independent protective variable in terms of mortality (OR 1.12; 95% CI, 0.983–1.275; p = 0.088). Overall, ICP monitor placement was independently associated with increased overall complications (OR 2.089; 95% CI, 1.85–2.358; p < 0.001), infectious complications (OR 2.282; 95% CI, 2.015–2.584; p < 0.001) and poor functional independence (OR 1.889; 95% CI, 1.575–2.264; p < 0.001). Sub analysis of the groups of patients with head AIS 3, 4, and 5 failed to show any protective effect of ICP monitors against mortality. In the group of patients with head AIS 4, ICP placement was an independent predictor of mortality (OR 2206; 95% CI, 1652–2948; p < 0.001).
Conclusions
Compliance with the BTF guidelines for ICP monitoring is poor. ICP monitoring does not have any survival benefit in patients with isolated severe blunt TBI and is associated with more complications and increased utilization of hospital resources.
Similar content being viewed by others
Introduction
One of the main target goals in the management of severe traumatic brain injury (TBI) is to maintain an adequate cerebral blood flow and oxygenation by preventing and treating timely any intracranial hypertension (IH) [1, 2]. IH may lead to secondary brain injury with serious effects on neurologic functional outcomes and higher mortality rates [3, 4].
Intracranial pressure (ICP) monitoring in severe TBI is recommended in the Brain Trauma Foundation (BTF) guidelines. The guidelines recommend ICP monitoring in patients with GCS < 9 and an abnormal head CT scan or in patients with a normal CT scan and two out of the following three conditions: age >40 years, unilateral/bilateral motor posturing and systolic blood pressure <90 mmHg [5].
Compliance with the BTF guidelines varies from country to country and hospital to hospital with previous studies reporting compliance from 9.6 to 75% [2, 6–14]. The effect of ICP monitoring on outcomes remains a controversial issue, with some studies showing no effect, others showing improved outcomes and others showing worse outcomes [2, 6–14]. In many institutions, the decision of whether or not and in what setting to use ICP monitoring is left to physician’s judgement [6].
The purpose of this study was to use a high-quality trauma database to assess compliance with BTF ICP monitoring guidelines and evaluate the effect of compliance on outcomes. In order to avoid the complexities of evaluating outcomes in multitrauma, we restricted the analysis to patients with isolated severe head trauma. By excluding patients with severe associated extracranial injuries, it is possible to get more meaningful conclusions on survival, complications, functional outcomes and hospital resources utilization following severe TBI.
Methods
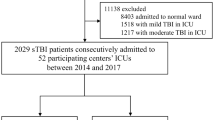
This study was based on the Trauma Quality Improvement Program (TQIP) database. TQIP is an American College of Surgeons detailed trauma database, with strict data quality control entered by participating trauma centers. After institutional review board approval, all adult patients (≥16 years old) with isolated severe blunt TBI who met the TBF criteria for ICP monitoring during a 2-year period (2013–2014) were included. Isolated severe TBI was defined as head Abbreviated Injury Scale (AIS) 3 or higher excluding patients with extracranial body part AIS 3 or higher. Patients transferred from outside hospitals and those that died upon arrival were excluded.
Variables extracted were demographics, comorbidities, mechanism of injury, injury specifics (epidural, subdural, subarachnoid, intracranial hemorrhage and diffuse axonal injury), AIS for each body area, Injury Severity Score (ISS), vital signs in the emergency department, ICP monitoring and type, compliance with BTF guidelines and craniectomy. Outcomes included in-hospital mortality, complications, ventilation days, intensive care unit (ICU) and hospital length of stay (HLOS), and functional independence at discharge.
The study population was stratified according to ICP monitoring device placement: patients subjected to ICP and those not undergoing ICP monitoring.
Statistical analysis
Categorical variables were reported as percentages while continuous variables were reported as medians with interquartile range (IQR). Continuous variables were also dichotomized using clinically relevant cutoff points. Univariate analysis was performed to compare for differences between two groups (mortality vs. no mortality and type of ICP monitoring). The Mann–Whitney U test was used to compare medians for continuous data points while Fisher exact or Pearson’s Chi-squared test were used to compare proportions for categorical variables.
Risk factors variables with p < 0.2 on univariate analysis were included into a forward stepwise logistic regression to identify independent predictors for overall mortality. Multicollinearity testing was performed to identify correlation between variables. The accuracy of the test was calculated using the area under the curve with 95% confidence interval. Variables with p < 0.05 were considered significant. All statistical analysis was performed using SPSS for windows version 23.0 (SPSS Inc. Chicago, IL).
Results
During the study period, 13,188 patients with isolated severe blunt TBI met the BTF guidelines for ICP monitoring. Overall, 1519 patients (11.5%) underwent ICP monitoring and the remaining 11,669 (88.5%) had no ICP monitor placed. In the group with ICP monitoring, 2.9% of patients had head AIS 3, 30.4% had an AIS 4, and 66.7% had an AIS 5 (Table 1).
Demographics, vital signs on admission, comorbid conditions, ISS, types and severity of head injuries, need for craniectomy and venous thromboembolism (VTE) prophylaxis for the two study groups were compared. In the group of patients with ICP monitoring, there were significantly fewer patients who were ≥65 years old (14.2 vs. 34.9%, p < 0.001), a lower incidence of comorbid conditions (40.0 vs. 50.5%, p < 0.001), fewer patients with hypotension on admission (2.3 vs. 3.5%, p = 0.012), a lower incidence of head AIS 3 or 4 but a higher incidence of head AIS 5 and a higher craniectomy rate (Table 1).
The overall 30-day mortality was 32.8%. The unadjusted mortality was similar in the two groups (31.8% inn the ICP group vs. 32.3%, in the no ICP group p = 0.756). A significantly higher prevalence of systemic complications (46.0 vs. 26.0%, p < 0.001), infectious complications (39.8 vs. 19.8%, p < 0.001) and thromboembolic events (10.9 vs. 6.2%, p < 0.001) was recorded in the group with ICP monitoring. Patients with ICP monitoring also had significantly more ventilator days and longer ICU and hospital length of stay (p < 0.001). Good functional independence outcome score at discharge was lower in the ICP group (16.6 vs. 29.7%, p < 0.001) (Table 2).
Forward stepwise logistic regression analysis identified age ≥65 years, head AIS 4 and 5, hypotension on admission and fall injury mechanism as independent factors associated with mortality. Placement of an ICP monitor had no significant effect on mortality, although there was a trend toward increased mortality in patients with monitor placement (OR 1.12; 95% CI, 0.983–1.275; p = 0.088; Table 3). Subgroup analysis done on patients with head AIS 3, 4 and 5, respectively, also showed age ≥65 years, hypotension on admission and fall mechanism to be independent risks factors for mortality. ICP placement was not significantly associated with mortality in AIS 3 and AIS 5 subgroups. In the subgroup of patients with head AIS 4, however, ICP placement had two times higher chance of mortality (OR 2.206; 95% CI, 1.652–2.948; p < 0.001).
ICP monitoring was found to be an independent risk factor for systemic complication (OR 2.089; 95% CI, 1.850–2.358; p < 0.001), infectious complication (OR 2.282; 95% CI, 2.015–2.584; p < 0.001) and poor functional independence (OR 1.889; 95% CI, 1.575–2.264; p < 0.001).
In an additional subgroup analysis, excluding patients who underwent craniectomy within the first 24 h, placement of an ICP monitor continued to have no effect on mortality (OR 1.015; 95% CI, 0.865–1.192; p = 0.852) and remained an independent risk factor for systemic complications (OR 2.223; 95% CI, 1.924–2.568; p < 0.001), infectious complications (OR 2.393; 95% CI, 2.063–2.775; p < 0.001), and poor functional independence outcomes (OR 1.968; 95% CI, 1.60–2.42; p < 0.001).
Discussion
ICP monitoring has become the recommended standard of care in the management of severe head trauma, in both children and adults. It is recommended by the Brain Trauma Foundation guidelines and endorsed by the American Association of Neurological Surgeons (AANS) [5].
The theoretical rationale for ICP monitoring is to maintain adequate cerebral blood flow and oxygenation by preventing or treating intracranial hypertension in a timely fashion. This, in turn, should decrease the risk of secondary brain injury and improve survival and neurologic functional outcomes. The extensively publicized relationship between intracranial hypertension and poor outcomes has led to the widespread use of ICP > 20 mmHg as the threshold for therapeutic interventions to lower the intracranial pressure. ICP monitoring can not only drive intervention, but also allow for evaluation of the response to various therapeutic pressure lowering interventions.
Despite the theoretical benefits and the recommendations by the various professional organizations, the compliance with ICP monitoring guidelines remains erratic and generally low and varies from 9.6 to 75% [2, 6–14]. In the current study, only 11.5% of patients who met the BTF guidelines underwent ICP monitoring. These findings indicate a significant reluctance by physicians to follow the guidelines. Although ICP monitoring device placement was exceedingly low, the rate of placement did increase with increasing severity of head injury with an ICP monitor placed in 3.0% of patients AIS 3, 9.9% AIS 4 and 14.4% AIS 5. One possible explanation is that, based on the judgement of the neurosurgeon, the potential risks of invasive monitoring may outweigh the benefits. This may be especially true in patients with moderately severe head injury and improving or increasingly evaluable mental status. Another explanation is that these data include a significant number of nonsurvivable injuries in which the treating physician may choose against monitor placement due to futility. However, the very low rate of ICP monitor placement in survivable injuries would not support this conclusion (2.8% of patients AIS 3, 9.9% of patients AIS 4). The most likely explanation for the low compliance is that, despite the universal recommendations and guidelines, the treating physicians are not convinced about the clinical value of routine ICP monitoring.
The role of ICP monitoring in improving outcomes is controversial and has been challenged by some studies. Some retrospective and prospective observational studies report improved outcomes with ICP monitoring. Farahvar et al. [2] in study of 2134 patients with severe TBI, as defined by GCS < 9, reported that patients managed with ICP monitoring had lower mortality at 2 weeks than those treated without an ICP monitor. Similarly, in a retrospective, trauma registry study from Canada, Lane et al. reported that ICP monitoring was associated with significantly improved survival [15]. These results were supported by a prospective, observational study including 166 older TBI patients with GCS < 9 on admission that showed that ICP monitoring was associated with decreased in-hospital mortality and improved 6-month functional outcomes [6]. In a multicenter trauma registry study of 844 patients with severe TBI, the authors reported that ICP monitoring was associated with an 8.3% point reduction in the risk-adjusted mortality rate [12] and a 2010 meta-analysis found that patients with ICP monitoring had a 12% lower mortality rate and 6% more favorable outcomes when compared with patients without ICP monitoring [16].
Despite the evidence in support of ICP monitoring, several authors have challenged these findings, reporting no benefit or even worse outcomes in the setting of monitor placement. Cremer et al. [7] in a retrospective analysis from the Netherlands concluded that patients managed with ICP monitors had prolonged mechanical ventilation and increased levels of therapy intensity, without evidence of improved outcome. Shafi et al. [8] in a NTDB analysis (1994–2001) reported that ICP monitoring in accordance with BTF guidelines was associated with worsening of survival and the authors cautioned against the use of ICP monitoring as a quality benchmark. Haddad et al. in a retrospective analysis of 477 with severe TBI concluded that overall ICP monitoring was not associated with reduced hospital mortality and there was a significant increase in mechanical ventilation duration, need for tracheostomy and ICU length of stay. Furthermore, in the group of patients with GCS 7–8, ICP monitoring was associated with a significant increase in in-hospital mortality [11]. In a prospective observational study in the Los Angeles regional trauma system, which includes 14 trauma centers, the rates of compliance with ICP monitoring ranged by center from 9.6 to 65.2%. There was no correlation between BTF guidelines compliance rates with ICP monitoring and mortality [9]. The only randomized study on this topic was performed in Bolivia and Ecuador with the support of the National Institutes of Health. In this multicenter, controlled trial, 324 patients with severe TBI were randomly assigned to ICP-guided therapy group or to a no ICP monitor group, in which treatment was based on imaging and clinical examination. The primary outcome was survival and functional status at 3 and 6 months. The authors found that ICP monitor-guided therapy was not superior to care based on imaging and clinical examination [13].
In the present study, logistic regression analysis failed to show any outcome benefit associated with ICP monitoring. This finding was confirmed in the subgroups of patients with head AIS 3, 4, and 5. Furthermore, in the subgroup of patients with head AIS 4, ICP placement was associated with significantly increased mortality. Our analysis also showed that ICP monitoring was an independent risk factor for systemic complications, infectious complications, and poor functional independence.
In the ICP monitor group, there was a higher incidence of craniectomy within 24 h of admission and it can be argued that these patients were potentially more severely injured than the patients with no ICP monitoring. In order to eliminate this potential bias, we performed another analysis after exclusion of patients with craniectomy within 24 h of admission. Again, ICP monitoring was not protective against mortality and was still an independent risk factor for systemic complications, infectious complications and poor functional independence outcomes.
The current study has the usual limitations of all databank-based studies. However, it has some unique strengths, including the high quality of the TQIP databank and most importantly the exclusion of patients with associated severe extracranial injuries, making comparisons of head injury-related outcomes more reliable. All previously published series included patients with major extracranial injuries. This is a major limitation in the assessment of head trauma-related mortality, complications and ICU and hospital length of stay.
This study adds support to the recommendations of other authors that a large, well-planned randomized study should be performed in the USA. The suggestion that it would not be ethical to include a control group without ICP monitoring is not scientific or sound. In view of the major significance of head trauma in terms of deaths, permanent disabilities, utilization of hospital resources and costs, our professional organizations should support a more rigorous scientific validation of the current national guidelines.
In conclusion, compliance with the Brain Trauma Foundation guidelines for ICP monitoring is poor. ICP monitoring does not seem to have any survival benefit in patients with isolated severe TBI and is associated with more complications and increased utilization of hospital resources. Good-quality randomized studies are warranted.
References
Mendelson AA, Gillis C, Henderson WR et al (2012) Intracranial pressure monitors in traumatic brain injury: a systematic review. Can J Neurol Sci 39:571–576
Farahvar A, Gerber LM, Chiu YL et al (2012) Increased mortality in patients with severe traumatic brain injury treated without intracranial pressure monitoring. J Neurosurg 117:729–734
Lobato RD, Sarabia R, Rivas JJ et al (1986) Normal computerized tomography scans in severe head injury. Prognostic and clinical management implications. J Neurosurg 65:784–789
Narayan RK, Kishore PR, Becker DP et al (1982) Intracranial pressure: to monitor or not to monitor? A review of our experience with severe head injury. J Neurosurg 56:650–659
Bratton SL, Chestnut RM, Ghajar J et al (2007) Guidelines for the management of severe traumatic brain injury. VI. Indications for intracranial pressure monitoring. J Neurotrauma 24(Suppl 1):S37–S44
You W, Feng J, Tang Q et al (2016) Intraventricular intracranial pressure monitoring improves the outcome of older adults with severe traumatic brain injury: an observational, prospective study. BMC Anesthesiol 16:35
Cremer OL, van Dijk GW, van Wensen E et al (2005) Effect of intracranial pressure monitoring and targeted intensive care on functional outcome after severe head injury. Crit Care Med 33:2207–2213
Shafi S, Diaz-Arrastia R, Madden C et al (2008) Intracranial pressure monitoring in brain-injured patients is associated with worsening of survival. J Trauma 64:335–340
Dawes AJ, Sacks GD, Cryer HG et al (2015) Compliance with evidence-based guidelines and interhospital variation in mortality for patients with severe traumatic brain injury. JAMA Surg 150:965–972
Agrawal D, Raghavendran K, Schaubel DE et al (2016) A propensity score analysis of the impact of invasive intracranial pressure monitoring on outcomes after severe traumatic brain injury. J Neurotrauma 33:853–858
Haddad S, Aldawood AS, Alferayan A et al (2011) Relationship between intracranial pressure monitoring and outcomes in severe traumatic brain injury patients. Anaesth Intensive Care 39:1043–1050
Dawes AJ, Sacks GD, Cryer HG et al (2015) Intracranial pressure monitoring and inpatient mortality in severe traumatic brain injury: a propensity score-matched analysis. J Trauma Acute Care Surg 78:492–501
Chesnut RM, Temkin N, Carney N et al (2012) A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med 367:2471–2781
Talving P, Karamanos E, Teixeira PG et al (2013) Intracranial pressure monitoring in severe head injury: compliance with Brain Trauma Foundation guidelines and effect on outcomes: a prospective study. J Neurosurg 119:1248–1254
Lane PL, Skoretz TG, Doig G et al (2000) Intracranial pressure monitoring and outcomes after traumatic brain injury. Can J Surg 43:442–448
Stein SC, Georgoff P, Meghan S et al (2010) Relationship of aggressive monitoring and treatment to improved outcomes in severe traumatic brain injury. J Neurosurg 112:1105–1112
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors deny any potential conflicts of interest.
Additional information
The original version of this article was revised: Lydia Lam’s given and family names were interchanged.
An erratum to this article is available at http://dx.doi.org/10.1007/s00268-017-3913-y.
Rights and permissions
About this article
Cite this article
Aiolfi, A., Benjamin, E., Khor, D. et al. Brain Trauma Foundation Guidelines for Intracranial Pressure Monitoring: Compliance and Effect on Outcome. World J Surg 41, 1543–1549 (2017). https://doi.org/10.1007/s00268-017-3898-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-3898-6