Abstract
Background
Postgastrectomy syndrome (PGS) remains a common complication after gastrectomy that affects patients’ quality of life. Although impaired gastrointestinal (GI) function by gastrectomy procedures is thought to be the cause, the precise pathophysiology of PGS is yet to be clarified.
Aim
The aim of this study was to investigate relationships between GI function and various symptoms or alimentary status in patients after gastrectomy.
Methods
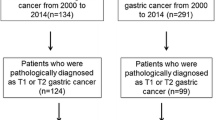
Fifty-one patients who underwent total or distal gastrectomy at least 1 year previously were studied. All patients replied to a questionnaire that asked presence of symptoms (esophageal reflux, nausea, abdominal pain, early satiation, diarrhea, early dumping general, early dumping abdominal, and late dumping symptoms) and alimentary status (change in body weight, food intake per meal, frequency of meals per day). They also underwent assessment of GI function consisting of gastric emptying study by 13C-acetate breath test to examine reservoir capacity and gastric emptying, and water load drink test to evaluate tolerance to volume loading (TVL). The relationships between GI function and each symptom or alimentary status were examined.
Results
The patients with nausea and early dumping general symptoms had significantly smaller reservoir capacity*, the patients with diarrhea and early dumping general symptoms had significantly faster gastric emptying*, and the patients with early satiation and early dumping abdominal symptoms had significantly impaired TVL*. Significant correlations were identified between TVL and body weight changes* or food intake per meal* (* p < 0.05).
Conclusion
Impaired postoperative GI function was closely related to symptoms or worse alimentary status.
Similar content being viewed by others
References
Eagon JC, Miedema BW, Kelly KA (1992) Postgastrectomy syndromes. Surg Clin North Am 72(2):445–465
Tsujimoto H, Sugasawa H, Ono S, Ichikura T, Yamamoto J, Hase K (2010) Has the accuracy of preoperative diagnosis improved in cases of early-stage gastric cancer? World J Surg 34:1840–1846
Nakada K, Ikeda M, Takahashi M, Kinami S, Yoshida M, Uenosono Y, Kawashima Y, Oshio A, Suzukamo Y, Terashima M, Kodera Y (2014) Characteristics and clinical relevance of postgastrectomy syndrome assessment scale (PGSAS)-45: newly developed integrated questionnaires for assessment of daily status and quality of life in postgastrectomy patients. Gastric Cancer. [Epub ahead of print]
Wu CW, Chiou JM, Ko FS, Lo SS, Chen JH, Lui WY, Whang-Peng J (2008) Quality of life after curative gastrectomy for gastric cancer in a randomised controlled trial. Br J Cancer 98(1):54–59
Mine S, Sano T, Tsutsumi K, Murakami Y, Ehara K, Saka M, Hara K, Fukagawa T, Udagawa H, Katai H (2010) Large-scale investigation into dumping syndrome after gastrectomy for gastric cancer. J Am Coll Surg 211(5):628–636
Hayami M, Seshimo A, Miyake K, Shimizu S, Kameoka S (2012) Effects of emptying function of remaining stomach on QOL in postgastrectomy patients. World J Surg 36(2):373–378
Le Blanc-Louvry I, Savoye G, Maillot C, Denis P, Ducrotté P (2003) An impaired accommodation of the proximal stomach to a meal is associated with symptoms after distal gastrectomy. Am J Gastroenterol 98(12):2642–2647
Sanaka M, Nakada K (2010) Stable isotope breath tests for assessing gastric emptying: a comprehensive review. J Smooth Muscle Res 46:267–280
Sanaka M, Nakada K, Nosaka C et al (2007) The Wagner–Nelson method makes the [13C]-breath test comparable to radioscintigraphy in measuring gastric emptying of a solid/liquid mixed meal in humans. Clin Exp Pharmacol Physiol 34:641–644
Kawamura M, Nakada K, Konishi H, Iwasaki T, Murakami K, Mitsumori N, Hanyu N, Omura N, Yanaga K (2014) Assessment of motor function of the remnant stomach by 13C breath test with special reference to gastric local resection. World J Surg 38(11):2898–2903
Nakada K, Ozone M, Harasawa S, Kawasaki N, Hanyu N, Kashiwagi H, Yanaga K (2010) Less invasive “New drink test” enables to detect intolerance to water volume load and illuminate underlying pathophysiology of symptoms in functional dyspepsia. (Abstract). Gut 59 Suppl 3 of A339
Griffith GH, Owen GM, Kirkman S, Shields R (1966) Measurement of rate of gastric emptying using chromium-51. Lancet 1(7449):1244–1245
Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, Maurer AH, McCallum RW, Nowak T, Nusynowitz ML, Parkman HP, Shreve P, Szarka LA, Snape WJ Jr, Ziessman HA (2008) American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol 103(3):753–763
Ghoos YF, Maes BD, Geypens BJ et al (1993) Measurement of gastric emptying rate of solids by means of a Carbon-labeled octanoic acid breath test. Gastroenterology 104:1640–1647
Katsube T, Konno S, Murayama M et al (2007) Gastric emptying after pylorus-preserving gastrectomy: assessment using the 13C-acetic acid breath test. Hepatogastroenterology 54:639–642
Tack J, Caenepeel P, Piessevaux H et al (2003) Assessment of meal induced gastric accommodation by a satiety drinking test in health and in severe functional dyspepsia. Gut 52:1271–1277
Jones MP, Hoffman S, Shah D, Patel K, Ebert CC (2003) The water load test: observations from healthy controls and patients with functional dyspepsia. Am J Physiol Gastrointest Liver Physiol 284(6):896–904
Boeckxstaens GE, Hirsch DP, van den Elzen BD, Heisterkamp SH, Tytgat GN (2001) Impaired drinking capacity in patients with functional dyspepsia: relationship with proximal stomach function. Gastroenterology 121(5):1054–1063
Montaño-Loza A, Schmulson M, Zepeda-Gómez S, Remes-Troche JM, Valdovinos-Diaz MA (2005) Maximum tolerated volume in drinking tests with water and a nutritional beverage for the diagnosis of functional dyspepsia. World J Gastroenterol 11(20):3122–3126
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Konishi, H., Nakada, K., Kawamura, M. et al. Impaired Gastrointestinal Function Affects Symptoms and Alimentary Status in Patients After Gastrectomy. World J Surg 40, 2713–2718 (2016). https://doi.org/10.1007/s00268-016-3613-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3613-z