Abstract
Background
Tranexamic acid (TXA), delivered intravenously or topically, has been shown to reduce blood loss, the need for transfusion, and relevant healthcare costs when administered in primary standard total hip arthroplasty (THA). Whether the same is true of oral TXA is unclear, the purpose of this study was to determine if oral tranexamic acid is equivalent to intravenous TXA in the case of patients undergoing THA via the direct anterior approach.
Methods
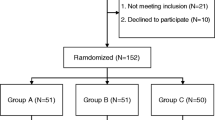
In this prospective randomized controlled trial, 120 patients undergoing primary THA by the direct anterior approach were randomized to receive oral TXA (two doses of 20 mg/kg), intravenous TXA (two doses of 15 mg/kg), or no TXA. Primary outcomes were haemoglobin drop, haematocrit levels, total blood loss, intra-operative blood loss, need for transfusion, and volume transfused. Secondary outcomes included thromboembolic events, wound complications, the length of post-operative hospital stay, and 30-day readmission.
Results
Demographic characteristics were similar among the three patient groups (p > 0.05, n = 40 per group). Haemoglobin drop, haematocrit levels, total blood loss, and intra-operative blood loss were similar in the oral and intravenous groups (p > 0.05), and significantly smaller than in the control group (p < 0.05). Transfusions were given to significantly fewer patients in the oral group (3%) and intravenous group (6%) than in the control group (27%, p = 0.01). Costs of TXA and transfusions were significantly lower in the oral group than the intravenous group (p < 0.05). The three groups were similar in thromboembolic events, wound complications, the length of post-operative hospital stay, and 30-day readmission (p > 0.05).
Conclusion
Oral TXA shows similar efficacy and safety as intravenous TXA for reducing haemoglobin drop, haematocrit levels, total blood loss, and transfusion rate following THA by the direct anterior approach. Therefore, the much less-expensive oral formulation may be superior to the intravenous form.





Similar content being viewed by others
References
Laupacis A, Bourne R, Rorabeck C, Feeny D, Wong C, Tugwell P, Leslie K, Bullas R (1993) The effect of elective total hip replacement on health-related quality of life. J Bone Joint Surg Am 75:1619–1626
Kurtz SM, Ong KL, Lau E, Bozic KJ (2014) Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am 96:624–630. https://doi.org/10.2106/jbjs.m.00285
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89:780–785. https://doi.org/10.2106/jbjs.f.00222
Kim JL, Park JH, Han SB, Cho IY, Jang KM (2017) Allogeneic blood transfusion is a significant risk factor for surgical-site infection following Total hip and knee arthroplasty: a meta-analysis. J Arthroplast 32:320–325. https://doi.org/10.1016/j.arth.2016.08.026
Kim C, Park SS, Davey JR (2015) Tranexamic acid for the prevention and management of orthopedic surgical hemorrhage: current evidence. J Blood Med 6:239–244. https://doi.org/10.2147/jbm.s61915
Toy PT, Kaplan EB, McVay PA, Lee SJ, Strauss RG, Stehling LC (1992) Blood loss and replacement in total hip arthroplasty: a multicenter study. The preoperative autologous blood donation study group. Transfusion 32:63–67
Carson JL, Duff A, Poses RM, Berlin JA, Spence RK, Trout R, Noveck H, Strom BL (1996) Effect of anaemia and cardiovascular disease on surgical mortality and morbidity. Lancet (London, England) 348:1055–1060. https://doi.org/10.1016/s0140-6736(96)04330-9
Ponnusamy KE, Kim TJ, Khanuja HS (2014) Perioperative blood transfusions in orthopaedic surgery. J Bone Joint Surg Am 96:1836–1844. https://doi.org/10.2106/jbjs.n.00128
Nielsen CS, Jans O, Orsnes T, Foss NB, Troelsen A, Husted H (2016) Combined intra-articular and intravenous tranexamic acid reduces blood loss in Total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. J Bone Joint Surg Am 98:835–841. https://doi.org/10.2106/jbjs.15.00810
Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM (2014) A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J 96-b:1005–1015. https://doi.org/10.1302/0301-620x.96b8.33745
Sharrock NE, Mineo R, Urquhart B, Salvati EA (1993) The effect of two levels of hypotension on intraoperative blood loss during total hip arthroplasty performed under lumbar epidural anesthesia. Anesth Analg 76:580–584
Sharrock NE, Salvati EA (1996) Hypotensive epidural anesthesia for total hip arthroplasty: a review. Acta Orthop Scand 67:91–107
Okamoto S, Hijikata-Okunomiya A, Wanaka K, Okada Y, Okamoto U (1997) Enzyme-controlling medicines: introduction. Semin Thromb Hemost 23:493–501. https://doi.org/10.1055/s-2007-996127
Camarasa Godoy MA, Serra-Prat M, Palomera Fanegas E (2008) Effectiveness of tranexamic acid in routine performance of total knee replacement surgery. Rev Esp Anestesiol Reanim 55:75–80
Jansen AJ, Andreica S, Claeys M, D'Haese J, Camu F, Jochmans K (1999) Use of tranexamic acid for an effective blood conservation strategy after total knee arthroplasty. Br J Anaesth 83:596–601
Alshryda S, Sarda P, Sukeik M, Nargol A, Blenkinsopp J, Mason JM (2011) Tranexamic acid in total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Br Vol 93:1577–1585. https://doi.org/10.1302/0301-620x.93b12.26989
Yang ZG, Chen WP, Wu LD (2012) Effectiveness and safety of tranexamic acid in reducing blood loss in total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am 94:1153–1159. https://doi.org/10.2106/jbjs.k.00873
Li J, Zhang Z, Chen J (2016) Comparison of efficacy and safety of topical versus intravenous tranexamic acid in total hip arthroplasty: a meta-analysis. Medicine (Baltimore) 95:e4689. https://doi.org/10.1097/md.0000000000004689
Irwin A, Khan SK, Jameson SS, Tate RC, Copeland C, Reed MR (2013) Oral versus intravenous tranexamic acid in enhanced-recovery primary total hip and knee replacement: results of 3000 procedures. Bone Joint J 95-b:1556–1561. https://doi.org/10.1302/0301-620x.95b11.31055
Kayupov E, Fillingham YA, Okroj K, Plummer DR, Moric M, Gerlinger TL, Della Valle CJ (2017) Oral and intravenous tranexamic acid are equivalent at reducing blood loss following Total hip arthroplasty: a randomized controlled trial. J Bone Joint Surg Am 99:373–378. https://doi.org/10.2106/jbjs.16.00188
Christensen CP, Jacobs CA (2015) Comparison of patient function during the first six weeks after direct anterior or posterior Total hip arthroplasty (THA): a randomized study. J Arthroplast 30:94–97. https://doi.org/10.1016/j.arth.2014.12.038
Post ZD, Orozco F, Diaz-Ledezma C, Hozack WJ, Ong A (2014) Direct anterior approach for total hip arthroplasty: indications, technique, and results. J Am Acad Orthop Surg 22:595–603. https://doi.org/10.5435/jaaos-22-09-595
Zhao HY, Kang PD, Xia YY, Shi XJ, Nie Y, Pei FX (2017) Comparison of early functional recovery after Total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. J Arthroplast 32:3421–3428. https://doi.org/10.1016/j.arth.2017.05.056
Irisson E, Hemon Y, Pauly V, Parratte S, Argenson JN, Kerbaul F (2012) Tranexamic acid reduces blood loss and financial cost in primary total hip and knee replacement surgery. Orthop Traumatol Surg Res 98:477–483. https://doi.org/10.1016/j.otsr.2012.05.002
Lozano M, Basora M, Peidro L, Merino I, Segur JM, Pereira A, Salazar F, Cid J, Lozano L, Mazzara R, Macule F (2008) Effectiveness and safety of tranexamic acid administration during total knee arthroplasty. Vox Sang 95:39–44. https://doi.org/10.1111/j.1423-0410.2008.01045.x
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58:277–280
Nadler SB, Hidalgo JH, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51:224–232
Liu X, Zhang X, Chen Y, Wang Q, Jiang Y, Zeng B (2011) Hidden blood loss after total hip arthroplasty. J Arthroplast 26:1100–1105.e1101. https://doi.org/10.1016/j.arth.2010.11.013
Lin ZX, Woolf SK (2016) Safety, efficacy, and cost-effectiveness of tranexamic acid in orthopedic surgery. Orthopedics 39:119–130. https://doi.org/10.3928/01477447-20160301-05
Hardy JF, Belisle S (1997) Natural and synthetic antifibrinolytics: inert, poisonous or therapeutic agents? Can J Anaesth 44:913–917. https://doi.org/10.1007/bf03011960
Zhang LK, Ma JX, Kuang MJ, Zhao J, Wang Y, Lu B, Sun L, Ma XL (2017) Comparison of oral versus intravenous application of tranexamic acid in total knee and hip arthroplasty: a systematic review and meta-analysis. Int J Surg (London, England) 45:77–84. https://doi.org/10.1016/j.ijsu.2017.07.097
Yuan X, Li B, Wang Q, Zhang X (2017) Comparison of 3 routes of administration of tranexamic acid on primary unilateral total knee arthroplasty: a prospective, randomized, controlled study. J Arthroplast 32:2738–2743. https://doi.org/10.1016/j.arth.2017.03.059
Pilbrant A, Schannong M, Vessman J (1981) Pharmacokinetics and bioavailability of tranexamic acid. Eur J Clin Pharmacol 20:65–72
Zohar E, Ellis M, Ifrach N, Stern A, Sapir O, Fredman B (2004) The postoperative blood-sparing efficacy of oral versus intravenous tranexamic acid after total knee replacement. Anesth Analg 99:1679–1683, table of contents. https://doi.org/10.1213/01.ane.0000136770.75805.19
Tuttle JR, Ritterman SA, Cassidy DB, Anazonwu WA, Froehlich JA, Rubin LE (2014) Cost benefit analysis of topical tranexamic acid in primary total hip and knee arthroplasty. J Arthroplast 29:1512–1515. https://doi.org/10.1016/j.arth.2014.01.031
Gillette BP, Maradit Kremers H, Duncan CM, Smith HM, Trousdale RT, Pagnano MW, Sierra RJ (2013) Economic impact of tranexamic acid in healthy patients undergoing primary total hip and knee arthroplasty. J Arthroplast 28:137–139. https://doi.org/10.1016/j.arth.2013.04.054
Xie J, Ma J, Yao H, Yue C, Pei F (2016) Multiple boluses of intravenous tranexamic acid to reduce hidden blood loss after primary total knee arthroplasty without tourniquet: a randomized clinical trial. J Arthroplast 31:2458–2464. https://doi.org/10.1016/j.arth.2016.04.034
Funding
This research did not receive financial support from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhao, H., Xiang, M., Xia, Y. et al. Efficacy of oral tranexamic acid on blood loss in primary total hip arthroplasty using a direct anterior approach: a prospective randomized controlled trial. International Orthopaedics (SICOT) 42, 2535–2542 (2018). https://doi.org/10.1007/s00264-018-3846-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3846-6