Abstract
Purpose
The aim of this study was to evaluate the frequency of chromosomal abnormalities in thyroid cancer patients before and after radioactive iodine administration in order to assess cytogenetic particularity in Polynesian thyroid cancer patients.
Methods
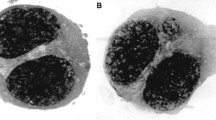
Chromosomal abnormalities were studied in 30 Polynesian patients with differentiated thyroid cancer, prior to and 4 days after 131I administration. Unstable chromosomal abnormalities were counted in peripheral blood lymphocytes using a conventional cytogenetic method. Peripheral blood was irradiated in vitro at different doses (0.5, 1 and 2 Gy) in order to establish the dose-response of the lymphocytes. Control groups were composed of 50 European thyroid cancer patients before and after first administration of 131I, and of ten European healthy donors. In addition, in vitro irradiation assays were performed at different doses (0.5, 1 and 2 Gy).
Results
The relative risk of spontaneous dicentrics before any radiation treatment was 2.9 (95% CI 1.7–5.1) times higher among Polynesian thyroid patients than among European thyroid cancer patients. After in vitro irradiation, the rise in frequency of dicentrics was similar in the Polynesian thyroid cancer group and the European thyroid patients and healthy donors. Four days after administration of 3.7 GBq 131I, the relative risk for a dicentric per cell was 1.3 (95% CI 1.0–1.5) times higher in Polynesian than in European patients. This can be explained by higher 131I retention in Polynesian compared with European patients. The results obtained revealed an increased frequency of cytogenetic abnormalities in Polynesian thyroid cancer patients compared with European control patients.
Conclusion
These preliminary findings are compatible with possible previous environmental aggression and therefore imply a need for further investigations on larger series including, in particular, French Polynesian healthy donors. In addition to French Polynesians, Maori and Hawaiian control groups could be useful.
Similar content being viewed by others
References
Parkin DM, Whelan SL, Ferlay J, Raymond L, Young J. Cancer incidence in five continents, vol VII, IARC Scientific Publications No. 143. Lyon: IARC; 1997.
de Vathaire F, Le Vu B, Vathaire CC. Thyroid cancer in French Polynesia between 1985 and 1995: influence of atmospheric nuclear bomb tests performed at Mururoa and Fangataufa between 1966 and 1974. Cancer Causes Control 2000;11:59–63.
Nagataki S, Nystrom E. Epidemiology and primary prevention of thyroid cancer (review). Thyroid 2002;12(10):889–96. DOI 10.1089/105072502761016511
Anderson D, Francis AJ, Godbert P, Jenkinson PC, Butterworth KR. Chromosome aberrations (CA), sister-chromatid exchanges (SCE) and mitogen-induced blastogenesis in cultured peripheral lymphocytes from 48 control individuals sampled 8 times over 2 years. Mutat Res 1991;250:467–76. DOI 10.1016/0027-2107(91)90203-Z
M’Kacher R, Legal JD, Schlumberger M, Voisin P, Aubert B, Gaillard N, Parmentier C. Biological dosimetry in patients treated with iodine-131 for differentiated thyroid carcinoma. J Nucl Med 1996;37(11):1860–4.
Albertini RJ, Anderson D, Douglas GR, Hagmar L, Hemminki K, Merlo F, et al. IPCS guidelines for the monitoring of genotoxic effects of carcinogens in humans. International Programme on Chemical Safety. Mutat Res 2000;463:111–72. DOI 10.1016/S1383-5742(00)00049-1
Lloyd DC, Purrott RJ, Reeder EJ. The incidence of unstable chromosome aberrations in peripheral blood lymphocytes from unirradiated and occupationally exposed people. Mutat Res 1980;72:523–32. DOI 10.1016/0027-5107(80)90123-2
Evans HJ, Buckton KE, Hamilton GE, Carothers A. Radiation-induced chromosome aberrations in nuclear-dockyard workers. Nature 1979;277:531–4.
Balakrishnan S, Rao S-B. Cytogenetic analysis of peripheral blood lymphocytes of occupational workers exposed to low levels of ionizing radiation. Mutat Res 1999;442:37–42. DOI 10.1016/S1383-5718(99)00056-X
Cigarran S, Barquinero J-F, Barrios L, Ribas M, Egozcue J, Caballin M-R. Cytogenetic analyses by fluorescence in situ hybridization (FISH) in hospital workers occupationally exposed to low levels of ionizing radiation. Radiat Res 2001;155:417–23.
Baugnet-Mahieu L, Lemaire M, Leonard E-D, Leonard A, Gerber G-B. Chromosome aberrations after treatment with radioactive iodine for thyroid cancer. Radiat Res 1994;140:429–31.
Finnon P, Moquet JE, Edwards AA, Lloyd DC. The 60Co gamma ray dose-response for chromosomal aberrations in human lymphocytes analysed by FISH; applicability to biological dosimetry. Int J Radiat Biol 1999;75:1215–22. DOI 10.1080/095530099139368
Durante M, Bonassi S, George K, Cucinotta FA. Risk estimation based on chromosomal aberrations induced by radiation. Radiat Res 2001;156:662–7.
Breslow NE, Day NE. Statistical methods in cancer research. Vol 1. The analysis of case-control studies. Lyon: International Agency for Research on Cancer; 1981.
Venzon DJ, Moolgavkar SH. A method for computing profile-likelihood-based confidence intervals. Appl Stat 1988;37:87–94.
Bauchinger M. Quantification of low-level radiation exposure by conventional chromosome aberration analysis. Mutat Res 1995;339:177–89.
Bonassi S, Hagmar L, Stromberg U, Montagud AH, Tinnerberg H, Forni A, et al. Chromosomal aberrations in lymphocytes predict human cancer independently of exposure to carcinogens. European Study Group on Cytogenetic Biomarkers and Health. Cancer Res 2000;60(6):1619–25.
Obe G, Pfeiffer P, Savage JR, Johannes C, Goedecke W, Jeppesen P, et al. Chromosomal aberrations: formation, identification and distribution. Mutat Res 2002;504:17–36. DOI 10.1016/S0027-5107(02)00076-3
Vodicka P, Kumar R, Stetina R, Sanyal S, Soucek P, Haufroid V, et al. Genetic polymorphisms in DNA repair genes and possible links with DNA repair rates, chromosomal aberrations and single strand breaks in DNA. Carcinogenesis 2004;25(5):757–63.
Bolognesi C. Genotoxicity of pesticides: a review of human biomonitoring studies. Mutat Res 2003;543:251–72. DOI 10.1016/S1383-5742(03)00015-2
Rupa DS, Reddy PP, Reddi OS. Frequencies of chromosomal aberrations in smokers exposed to pesticides in cotton fields. Mutat Res 1989;222:37–41. DOI 10.1016/0165-1218(89)90033-5
Vijayalaxmi, Evans HJ. In vivo and in vitro effects of cigarette smoke on chromosomal damage and sister-chromatid exchange in human peripheral blood lymphocytes. Mutat Res 1982;92:321–32. DOI 10.1016/00227-5107(82)90234-2
Littlefield LG, Joiner EE. Analysis of chromosome aberrations in lymphocytes of long-term heavy smokers. Mutat Res 1986;170:145–50. DOI 10.1016/0165-1218(86)90028-5
Wang LE, Bondy ML, de Andrade M, Strom SS, Wang X, Sigurdson A, et al. Gender difference in smoking effect on chromosome sensitivity to gamma radiation in a healthy population. Radiat Res 2000;154:20–7.
M’Kacher R, Légal JD, Schlumberger M, Aubert B, Béron-Gaillard N, Gaussen A, Parmentier C. Sequential biological dosimetry after a single treatment with iodine-131 for differentiated thyroid carcinoma. J Nucl Med 1997;38:377–80.
Acknowledgements
This work was funded by grants from Electricité de France (EDF) 98-04 and Institut Gustave Roussy CCR# 98-25. The authors thank the nurses, technologists and secretaries for their support and participation in this study. We are grateful to Prof. Martin Schlumberger (Department of Nuclear Medicine) for clinical data and to Nadine Béron-Gaillard for her efficient collaboration. We are indebted to Mrs. Corinne Ridgway for reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Violot, D., M’kacher, R., Adjadj, E. et al. Evidence of increased chromosomal abnormalities in French Polynesian thyroid cancer patients. Eur J Nucl Med Mol Imaging 32, 174–179 (2005). https://doi.org/10.1007/s00259-004-1662-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-004-1662-2