Abstract
Decreased physical activity is associated with cardiovascular, metabolic and mental health disease. While decreases in physical activity during the COVID-19 pandemic have been described in the general population, there is a paucity of data regarding children with underlying cardiovascular disease. We hypothesized there would be a decrease in physical activity at the onset of the COVID-19 pandemic. Performed a single-center, retrospective cohort study of children aged < 19 years with cardiac rhythm management devices. Patients were included if they had device-measured physical activity data from > 80% of dates from February 3, 2020 through June 30, 2020. Patients with significant neurologic/neuromuscular disease were excluded. We identified 144 patients with a median age of 15.4 years. 47% were female. 34% had congenital heart disease, 20% had cardiomyopathy, 19% had an inherited arrhythmia syndrome and 5% had atrioventricular block without congenital heart disease. 47% of patients had an implantable loop recorder, 29% had a permanent pacemaker and 24% had an implantable cardioverter-defibrillator. We observed a significant decrease in device-measured physical activity from baseline (February 3–March 9), with up to a 21% decrease in physical activity during mid-March through early May. Activity levels returned to pre-pandemic levels in June. Physical activity sharply declined in children with cardiac rhythm management devices at the onset of the COVID-19 pandemic. These data highlight the importance of finding strategies to maintain physical activity during the current pandemic and future public health crises.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has had profound effects on the lives of billions across the globe since its onset in December of 2019. In order to combat the outbreak and slow the spread of disease, social distancing guidelines were implemented and, in many places, shelter in place orders were put in place. Investigators have shown that physical activity declined after the onset of the COVID-19 pandemic in both pediatric and adult populations [1,2,3].
Even prior to the onset of the COVID-19 pandemic, inadequate physical activity was common in the USA with less than one-quarter of school-aged children participating in the recommended 60 min of physical activity daily [4]. Importantly, consequences of decreased physical activity include increased risk of developing cardiovascular and metabolic disease [5,6,7,8,9]. Avoidance of these conditions is likely to be of increased importance in individuals with underlying heart disease.
Many cardiac rhythm management devices (CRMDs) are capable of collecting device-measured physical activity data by utilizing internal accelerometers or detectors of thoracic impedance to detect changes in patient movement which are translated into electronic data and made available to the clinicians managing patients with these devices using proprietary algorithms [10]. Prior studies comparing device-measured physical activity from implanted CRMDs against either previously validated external accelerometers or 6-min walk tests have shown moderate correlation [11,12,13,14,15].
There is a paucity of data regarding how the COVID-19 pandemic and associated restrictions have affected children with cardiovascular disease. We hypothesized there would be a decrease in physical activity in this population related to the onset of the COVID-19 pandemic and the associated “shelter-in-place” (SIP) order in the state of Massachusetts issued on March 24, 2020.
Methods
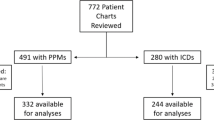
We performed a single-center, retrospective cohort study of children and adolescents aged less than 19 years and followed at Boston Children’s Hospital with CRMDs including permanent pacemakers, implantable cardioverter-defibrillators (ICDs), and implantable loop recorders capable of tracking daily activity level. Patients were included if they had device-measured physical activity data from > 80% of dates across the study period from the start of February 3, 2020 through June 30, 2020. Patients may have had data from < 80% of the study period if their CRMD was implanted or explanted during the study period or if transtelephonic transmissions or device checks were not performed routinely. Patients with neurologic and neuromuscular diseases expected to have a significant impact on physical activity such as hypoxic ischemic encephalopathy or skeletal myopathy were excluded. This study was approved by the Institutional Review Board of our institution with a waiver of informed consent.
Device-measured physical activity data were abstracted from databases kept by the CRMD manufacturers (Medtronic Inc., Minneapolis, Minnesota and Boston Scientific, Natick, Massachusetts) or CRMD reports available through our internal electronic medical record in hours of device-measured physical activity per day. Some devices included in this study had a maximum daily device-measured physical activity of 8 h. We additionally collected information regarding the type of CRMD implanted and demographic information including age, sex, body mass index (BMI), and state of residence. We also collected cardiovascular disease-specific information including the nature of cardiovascular disease which we broadly classified as structural congenital heart disease (CHD), cardiomyopathy, atrioventricular conduction disturbances without associated CHD, and inherited arrhythmia syndromes. Patients who did not have a disease process described by any of the aforementioned categories were categorized as ‘other’.
The study period was divided into five time periods defined as follows: Baseline (February 2 through March 9), Pre-SIP (March 10 through March 23), Early SIP (March 24 through April 6), Late SIP (April 7 through May 4) and June (June 1 through June 30) (Fig. 1). These dates were chosen to correspond with Massachusetts social distancing guidance to assess changes in physical activity before and after SIP orders were given. The primary outcome was hours per day of device-measured physical activity in each time period compared to the baseline period and this relationship was assessed using the paired Student’s t tests. We compared the proportion of patients with < 2 h of daily device-measured physical activity at baseline to each of the subsequent time periods using Chi-squared tests. We also performed a sub-analysis of children less than 6 years of age using Wilcoxon signed-rank tests. We compared differences in device-measured physical activity in patients with elevated body mass index (BMI; BMI ≥ 85%ile) with those with non-elevated BMIs, between male and female patients and between Massachusetts residents and non-Massachusetts New England residents using Wilcoxon rank-sum tests. Finally, in the subset of patients with activity data available from February through June in 2019, 2020 and 2021, we compared 2020 levels of activity with 2019 and 2021 levels of activity. We also compared activity levels from the baseline period in 2019 with the subsequent 2019 time periods and activity levels from the baseline period in 2021 with subsequent 2021 time periods using paired Student’s t tests. Statistical analyses were performed using Stata 16 statistical software (Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC).
Results
We identified 180 patients who met inclusion criteria. Of this group, 30 had insufficient device-measured physical activity data and six had significant neurologic or neuromuscular comorbidities and were excluded. This left 144 patients whose characteristics are summarized in Table 1. We observed statistically significant declines in device-measured physical activity from baseline in each of the subsequent time periods beginning in the pre-SIP period through the late SIP period with recovery of activity in June (Fig. 2A). The maximal decline in device-measured physical activity occurred in the early SIP period with a median 21% decrease in activity from baseline levels (interquartile range 2–37%; p < 0.001). There was a statistically significant increase in the number of patients with < 2 h of device-measured physical activity per day in each period compared to the baseline period (Fig. 2B). In a sub-analysis of children < 6 years of age, we found no statistically significant change in device-measured physical activity from baseline aside from an increase in June.
Children and adolescents who had elevated BMI were statistically significantly less active than those who had non-elevated BMI at baseline and during every subsequent time period (Fig. 3). There was no statistically significant difference in device-measured physical activity in males compared to females and no statistically significant difference in device-measured physical activity between residents of Massachusetts and residents of other New England states during any time period.
A subset of patients additionally had activity data available from the same time periods in 2019 and 2021 (Fig. 4). These patients were statistically significantly less active in 2020 compared to the corresponding time periods in 2019 in each of the study periods. They were also statistically significantly less active in 2020 compared to 2021 in early SIP, late SIP, and June and were also less active in the pre-SIP period, though this narrowly missed statistical significance (p = 0.07). There were no statistically significant differences in activity levels between 2019 and 2021. In 2019 and 2021, these patients exhibited no statistically significant change in activity from baseline during any of the subsequent time periods aside from an increase in activity during June during both years.
Discussion
In this study of activity in children and adolescents with CRMDs at the onset of the COVID-19 pandemic in the USA, we found statistically significant declines in device-measured physical activity, a validated measure of physical activity [11,12,13,14,15], and a threefold increase in the number of patients with < 2 h of daily device-measured physical activity. Preschool-aged children < 6 years of age did not experience a decline in device-measured physical activity. Children with elevated BMI were less active than those with non-elevated BMI during each of the study periods and there was no difference in activity between girls and boys.
These findings need to be viewed in the context of both the global COVID-19 pandemic as well as local burden of disease and local response to the pandemic. For reference, the World Health Organization declared COVID-19 a pandemic on March 1, 2020 [16] and a SIP order went into effect in Massachusetts, where a majority our study population resided, on March 24. Schools in Massachusetts were closed for in-person instruction on March 16 and remained closed through June 29. At the start of our study period, the 7-day average of new daily confirmed SARS-CoV-2 cases in Massachusetts was 0 cases per day, peaked at nearly 2500 in late April and fell to approximately 200 by the end of our study period in late June 2020 [17].
We observed a clear decline in physical activity level that corresponded with an increasing local burden of COVID-19 cases and a subsequent increase in physical activity as COVID-19 cases declined. This observation has important local and national implications about responses to surges in COVID-19 infections and future pandemics. Given that the local increase in COVID-19 cases largely coincided with the Massachusetts SIP order, it is difficult to differentiate the roles played by local burden of disease and SIP guidelines in the reduction of device-measured physical activity we observed. It is worth noting, however, that there was a statistically significant decline in device-measured physical activity in the 2 weeks preceding the SIP order, suggesting family response to the burden of COVID-19 disease contributed to a decrease in physical activity independent of the SIP order—a response which may have been exaggerated in the families of children with cardiac disease. Additionally, we found no statistically significant reduction in device-measured physical activity in patients living in Massachusetts compared to other states in New England where COVID-19 infections were not as widespread [17], demonstrating the impact of the pandemic on physical activity across state lines and in places with variable burdens of COVID-19 disease.
In contrast to what we observed in 2020, there was no decline in device-measured physical activity from the designated baseline period to subsequent time periods in 2019, suggesting the changes we observed in 2020 are not explained by seasonal variation in physical activity level. Indeed, device-measured physical activity levels in this subset of patients were significantly lower in each time period in 2020 compared to 2019 including during the defined baseline period. Thus, behavioral modification leading to decreased physical activity likely predated the start of our study period and the decline in 2020 activity from “baseline” levels may have been even more dramatic than our analysis suggests. Interestingly, activity levels in the subset of patients for whom we abstracted 2021 device-measured physical activity level data were no different than their levels in 2019, suggesting the impact of the ongoing COVID-19 pandemic on decreasing activity levels has waned over time.
The impact of physical activity on health in children is well-established with diminished physical activity linked to a host of cardiovascular and metabolic diseases [5,6,7,8,9] and childhood obesity linked to stigmatization, bullying, lower self-esteem, increased frequency of anxiety and depression and increased likelihood of adulthood obesity [18,19,20,21]. Additionally, childhood physical activity has been shown to be a predictor of physical activity in adulthood [22]. Previous studies of children with underlying heart disease have reported rates of elevated BMI similar to the approximately 1 in 3 we found in the present study and thus this is an important issue for this population [21, 23,24,25,26]. Heart rhythm disturbances have been found to be risk factors for obesity possibly secondary to restricted activity secondary to increased risk (or perceived risk) with exercise [26]. Prior work in adults with CRMDs has demonstrated a beneficial impact of physical activity on secondary prevention of life-threatening arrhythmic events and reduction in ICD shocks [27,28,29]. These previously demonstrated associations highlight the negative impact of the reduction in device-measured physical activity observed in our study population.
Limitations of our study include its relatively small number of patients and retrospective nature. The device-measured physical activity data collected by CRMDs is binary in nature and thus does not discriminate between activity which barely meets the threshold for classification considered to be “active” and intense activity which far exceeds this threshold. Furthermore, the precise threshold and equivalent level of physical activity is not made available by the device manufacturers. These thresholds are additionally modifiable and it is possible that patients had different thresholds programmed. However, it is not our general practice to modify the activity threshold from the default setting and thus it is unlikely that this contributed to measured variations in activity between patients or in the same patient over time in a meaningful way. This analysis did not include the secondary peaks in COVID-19 infections seen in late 2020, but did include data from the same time periods in 2021.
In conclusion, we found levels of device-measured physical activity in school-aged children and adolescents with CRMDs declined in excess of 20% after the onset of the COVID-19 pandemic and institution of SIP guidelines. This decline in activity was not explained by seasonal variation in activity level and persisted for several months. Children < 6 years of age appear spared from this decline and there were no differences between girls and boys. These findings have significant implications given the demonstrated benefits of physical activity on cardiovascular and overall health in the general population, and in this population of children with underlying cardiac conditions in particular, as well as the ongoing nature of the COVID-19 pandemic and potential for future public health crises with similar effects. These data add to the evidence that the implications of the COVID-19 pandemic reach multiple areas of daily life.
Data Availability
Data are available upon request.
Code Availability
Not applicable.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- CRMDs:
-
Cardiac rhythm management devices
- ICD:
-
Implantable cardioverter-defibrillator
- CHD:
-
Congenital heart disease
- BMI:
-
Body mass index
- SIP:
-
Shelter in place
- WHO:
-
World Health Organization
References
Castañeda-Babarro A, Arbillaga-Etxarri A, Gutiérrez-Santamaría B, Coca A (2020) Physical activity change during COVID-19 confinement. Int J Environ Res Public Health 17(18):6878
Dunton GF, Do B, Wang SD (2020) Early effects of the COVID-10 pandemic on physical activity and sedentary behavior in children living in the US. BMC Public Health 20(1):1351
Tison GH, Avram R, Kuhar P, Abreau S, Marcus GM, Pletcher MJ et al (2020) Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann Intern Med 173(9):767–770
Child and Adolescent Health Measurement Initiative (CAHMI) (2016) Data resource center for child and adolescent health. 2016 National survey of children’s health: child and family health measures and subgroups
Centers for Disease Control and Prevention (2010) The association between school based physical activity, including physical education, and academic performance. US Department of Health and Human Services, Atlanta
Physical Activity Guidelines Advisory Committee (2018) 2018 Physical Activity Guidelines Advisory Committee Scientific Report. US Dept of Health and Human Services, Washington
Loprinzi PD, Lee I, Andersen RE, Crespo CJ, Smit E (2015) Association of concurrent healthy eating and regular physical activity with cardiovascular disease risk factors in US youth. Am J Health Promot 30(1):2–8
Cuenca-Garcia M, Ortega FB, Ruiz JR, Gonzalez-Gross M, Labayen I, Jago R et al (2014) Combined influence of healthy diet and active lifestyle on cardiovascular disease risk factors in adolescents. Scand J Med Sci Sports 24(3):553–562
Kriska A, Delahanty L, Edelstein S, Amodei N, Chadwick J, Copeland K et al (2013) Sedentary behavior and physical activity in youth with recent onset of type 2 diabetes. Pediatrics 131(3):e850–e856
AJMC Staff. A Timeline of COVID-19 Developments in 2020 (2020) AJMC website. https://www.mass.gov/orgs/department-of-public-health. Accessed 8 Dec 2020
Vegh EM, Kandala J, Orencole M, Upadhyay GA, Sharma A, Miller A et al (2014) Device-measured physical activity versus six-minute walk test as a predictor of reverse remodeling and outcome after cardiac resynchronization therapy for heart failure. Am J Cardiol 113:1523–1528
Kadhiresan VA, Pastore J, Auricchio A, Sack S, Doelger A, Girouard S et al (2002) A novel method—the activity log index—for monitoring physical activity of patients with heart failure. Am J Cardiol 89:1435–1437
Pressler A, Danner M, Esefeld K, Haller B, Scherr J, Schömig A et al (2013) Validity of cardiac implantable electronic devices in assessing daily physical activity. Int J Cardiol 168:1127–1130
Shoemaker MJ, Cartwright K, Hanson K, Serba D, Dickinson MG, Kowalk A (2017) Concurrent validity of daily activity data from Medtronic ICD/CRT devices and the actigraph GT3X triaxial accelerometer: a pilot study. Cardiopulm Phys Ther J 28:3–11
Rosman L, Lampert R, Sears SF, Burg MM (2018) Measuring physical activity with implanted cardiac devices: a systematic review. J Am Heart Assoc 7(11):e008663
Kawabata M, Fantoni C, Regoli F, Raffa S, Pastori F, Fratini S et al (2007) Activity monitoring in heart failure patients with cardiac resynchronization therapy. Circ J 71:1885–1892
Center for Disease Control and Prevention (2020) CDC COVID Data Tracker. https://covid.cdc.gov/covid-datatracker/#cases_casesper100klast7days. Accessed 8 Dec 2020
Morrison KM, Shin S, Tarnopolsky M, Taylor VH (2015) Association of depression and health related quality of life with body composition in children and youth with obesity. J Affect Disord 172:18–23
Halfon N, Kandyce L, Slusser W (2013) Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of US children aged 10 to 17. Acad Pediatr 13(1):6–13
Beck AR (2016) Psychosocial aspects of obesity. NASN Sch Nurse 31(1):23–27
Simmonds M, Llewellyn A, Owen CG, Woolacott N (2016) Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev 17(2):95–107
Telama R, Yang X, Viikari J, Valimaki I, Wanne O, Raitakari O (2005) Physical activity from childhood to adulthood: a 21-year tracking study. Am J Prev Med 28(3):267–273
Barbiero SM, Sica CDA, Schuh DS et al (2014) Overweight and obesity in children with congenital heart disease: combination of risks for the future? BMC Pediatr 14:271
Cohen MS (2012) Clinical practice: the effect of obesity in children with congenital heart disease. Eur J Pediatr 171:1145–1150
Tamayo C, Manlhiot C, Patterson K, Lalani S, McCrindle BW (2015) Longitudinal evaluation of the prevalence of overweight/obesity in children with congenital heart disease. Can J Cardiol 31(2):117–123
Steele JM, Preminger TJ, Erenberg FG, Wang L, Dell K, Alsaied T et al (2019) Obesity trends in children, adolescents, and young adults with congenital heart disease. Congenit Heart Dis 14(4):517–524
Darden D, Richardson C, Jackson EA (2013) Physical activity and exercise for secondary prevention among patients with cardiovascular disease. Curr Cardiovasc Risk Rep 7:411–416
Lampert R (2017) No further question: cardiac rehabilitation benefits patients with implantable-cardioverter defibrillators: insurers, are you listening? JACC Clin Electrophysiol 3:127–128
Pandey A, Parashar A, Moore C, Ngo C, Salahuddin U, Bhargava M et al (2017) Safety and efficacy of exercise training in patients with an implantable cardioverter-defibrillator: a meta-analysis. JACC Clin Electrophysiol 3:117–126
Funding
No specific funding/support.
Author information
Authors and Affiliations
Contributions
RP: Participated study concept/design, in data collection, analysis and interpretation and authored the first draft. MC, ML: Participated in data collection and critical revision of the article and approval of the article. DM, KS, NG, SF: Provided critical revision of the article and approval of the article. JT, MA: Participated in study concept/design, provided critical revision of the article and approval of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relative to this article to disclose.
Ethical Approval
This study was completed after obtaining a waiver of exemption from the Institutional Review Board at Boston Children’s Hospital.
Consent to Participate
Not applicable.
Consent for Publication
All authors provide consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Przybylski, R., Craig, M., Lippmann, M. et al. Activity During the COVID-19 Pandemic in Children with Cardiac Rhythm Management Devices. Pediatr Cardiol 43, 784–789 (2022). https://doi.org/10.1007/s00246-021-02787-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02787-8