Abstract
Introduction
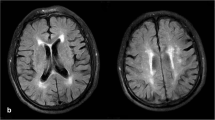
Severity of vascular damage of white matter may predict hemorrhagic transformation (HT). We assess the relationship between leukoaraiosis (LA) severity and the type of hemorrhagic transformation in elderly patients treated with thrombolysis.
Methods
We retrospectively analyzed the clinical data and pretreatment magnetic resonance imaging (MRI) of 180 consecutive ischemic stroke patients aged over 75 years. LA severity was graded according to the Fazekas scale, and acute diffusion-weighted-imaging (DWI) lesion volumes were semi-automatically outlined. Predictors of hemorrhagic infarction (HI) and parenchymal hemorrhage (PH) were identified using logistic regression analysis and exact multinomial logistic analysis.
Results
HT occurred in 31 patients (17 %). Baseline National Institute of Health Stroke Score (NIHSS; p = 0.008), severe LA (p = 0.02), and diffusion lesion volume (p = 0.02) were predictors of HT in univariable logistic regression. Adjusted to lesion volume and baseline NIHSS score, exact multinomial logistic analysis showed that severe LA was the only independent predictor of parenchymal hemorrhage (p = 0.03).
Conclusion
In elderly patients, LA severity better predicts parenchymal hemorrhage than infarct size.

Similar content being viewed by others
Abbreviations
- LA:
-
Leukoaraiosis
- WMH:
-
White matter hyperintensity
- HT:
-
Hemorrhagic transformation
- ICH:
-
Intracerebral hemorrhage
- HI:
-
Hemorrhagic infarction
- PH:
-
Parenchymal hemorrhage
- NIHSS:
-
National Institute of Health Stroke Score
- MRI:
-
Magnetic resonance imaging
- SVD:
-
Small-vessel disease
- CMBs:
-
Cerebral microbleeds
- tPA:
-
Tissue plasminogen activator
References
Bonita R, Anderson CS, Broad JB, Jamrozik KD, Stewart-Wynne EG, Anderson NE (1994) Stroke incidence and case fatality in Australasia. A comparison of the Auckland and Perth population-based stroke registers. Stroke 25:552–7
Marini C, Baldassarre M, Russo T, De Santis F, Sacco S, Ciancarelli I et al (2004) Burden of first-ever ischemic stroke in the oldest old: evidence from a population-based study. Neurology 62:77–81
Di Carlo A, Baldereschi M, Gandolfo C, Candelise L, Ghetti A, Maggi S et al (2003) Stroke in an elderly population: incidence and impact on survival and daily function. Italian Longitudinal Study on Aging. Cerebrovasc Dis 16:141–50
Derex L, Nighoghossian N (2009) Thrombolysis, stroke-unit admission and early rehabilitation in elderly patients. Nat Rev Neurol 5:506–11
Mishra NK, Ahmed N, Andersen G, Egido JA, Lindsberg PJ, Ringleb PA et al (2010) Thrombolysis in very elderly people: controlled comparison of SITS International Stroke Thrombolysis Registry and Virtual International Stroke Trials Archive. BMJ 23:341–c604
Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E et al (2014) Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 384(9958):1929–35
IST-3 collaborative group (2015) Association between brain imaging signs, early and late outcomes, and response to intravenous alteplase after acute ischaemic stroke in the third International Stroke Trial (IST-3): secondary analysis of a randomised controlled trial. Lancet Neurol 14(5):485–96
Ringleb PA, Schwark C, Kohrmann M, Kulkens S, Juttler E, Hacke W et al (2007) Thrombolytic therapy for acute ischaemic stroke in octogenarians: selection by magnetic resonance imaging improves safety but does not improve outcome. J Neurol Neurosurg Psychiatry 78:690–3
Singer OC, Humpich MC, Fiehler J, Albers GW, Lansberg MG, Kastrup A, for the MR Stroke Study Group Investigators et al (2008) Risk for symptomatic intracerebral hemorrhage after thrombolysis assessed by diffusion-weighted magnetic resonance imaging. Ann Neurol 63:52–60
Lansberg MG, Thijs VN, Bammer R, Kemp S, Wijman CA, Marks MP et al (2007) DEFUSE Investigators. Risk factors of symptomatic intracerebral hemorrhage after tPA therapy for acute stroke. Stroke 38:2275–2278
Jung S, Mono ML, Findling O, Fischer U, Galimanis A, Weck A et al (2012) White matter lesions and intra-arterial thrombolysis. J Neurol 7:1331–6
Neumann-Haefelin T, Hoelig S, Berkefeld J, Fiehler J, Gass A, Humpich M et al (2006) Leukoaraiosis is a risk factor for symptomatic intracerebral hemorrhage after thrombolysis for acute stroke. Stroke 37:2463–2466
Arsava EM, Rahman R, Rosand J, Lu J, Smith EE, Rost NS et al (2014) Severity of leukoaraiosis correlates with clinical outcome after ischemic stroke. Neurology 72:1403–1410
Henninger N, Lin E, Baker SP, Wakhloo AK, Takhtani D, Moonis M (2012) Leukoaraiosis predicts poor 90-day outcome after acute large cerebral artery occlusion. Cerebrovasc Dis 33:525–531.15
Pantoni L (2010) Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol 9:689–701
Fiehler J, Albers GW, Boulanger JM, Derex L, Gass A, Hjort N, Group MRSTROKE et al (2007) Bleeding Risk Analysis in Stroke Imaging before ThromboLysis (BRASIL): pooled analysis of T 2 *-weighted magnetic resonance imaging data from 570 patients. Stroke 38:2738–2744
Dannenberg S, Scheitz JF, Rozanski M, Erdur H, Brunecker P, Werring DJ et al (2014) Number of cerebral microbleeds and risk of intracerebral hemorrhage after intravenous thrombolysis. Stroke 10:2900–5
Gratz PP, El-Koussy M, Hsieh K, von Arx S, Mono ML, Heldner MR (2014) Preexisting cerebral microbleeds on susceptibility-weighted magnetic resonance imaging and post-thrombolysis bleeding risk in 392 patients. Stroke 6:1684–8
Curtze S, Melkas S, Sibolt G, Haapaniemi E, Mustanoja S, Putaala J et al (2015) Cerebral computed tomography-graded white matter lesions are associated with worse outcome after thrombolysis in patients with stroke. Stroke 6:1554–60
Curtze S, Haapaniemi E, Melkas S, Mustanoja S, Putaala J, Sairanen T et al (2015) White matter lesions double the risk of post-thrombolytic intracerebral hemorrhage. Stroke 8:2149–55
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R et al (2013) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 8:822–38
Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D et al (1998) Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet 352:1245–1251
Hirji KF, Mehta CR, Patel NR (1987) Computing distributions for exact logistic regression. J Am Stat Assoc 82:1110–1117
Kaffashian S, Tzourio C, Zhu YC, Mazoyer B, Debette S (2016) Differential effect of white-matter lesions and covert brain infarcts on the risk of ischemic stroke and intracerebral hemorrhage. Stroke 47(7):1923–1925
Whiteley WN, Slot KB, Fernandes P, Sandercock P, Wardlaw J (2012) Risk factors for intracranial hemorrhage in acute ischemic stroke patients treated with recombinant tissue plasminogen activator: a systematic review and meta-analysis of 55 studies. Stroke 43(11):2904–9.2
Derex L, Hermier M, Adeleine P, Pialat JB, Wiart M, Berthezène Y et al (2005) Clinical and imaging predictors of intracerebral haemorrhage in stroke patients treated with intravenous tissue plasminogen activator. J Neurol Neurosurg Psychiatry 1:70–5
Kahles T, Foerch C, Sitzer M, Schroeter M, Steinmetz H, Rami A et al (2005) Tissue plasminogen activator mediated blood–brain barrier damage in transient focal cerebral ischemia in rats: relevance of interactions between thrombotic material and thrombolytic agent. Vasc Pharmacol 43:254–259
Albers GW, Thijs VN, Wechsler L, for the DEFUSE Investigators et al (2006) Magnetic resonance imaging profiles predict clinical response to early reperfusion: the Diffusion and Perfusion Imaging Evaluation For Understanding Stroke Evolution (DEFUSE) study. Ann Neurol 60:508–517
Henninger N, LinE HDC, LehmanLL TD, Selim M et al (2013) Leukoaraiosis and sex predict the hyperacute ischemic core volume. Stroke 44:61–67
Bivard A, Cheng X, Lin LT, Levi C, Spratt N, Kleinig T, O’Brien B, Butcher K et al (2016) Global white matter hypoperfusion on CT predicts larger infarcts and hemorrhagic transformation after acute ischemia. CNS Neurosci Ther 22(3):238–43
Shoamanesh A, Kwok CS, Lim PA, Benavente OR (2013) Post-thrombolysis intracranial hemorrhage risk of cerebral microbleeds in acute stroke patients: a systematic review and meta-analysis. Int J Stroke 5:348–56
Charidimou A, Shoamanesh A, Wilson D, Gang Q, Fox Z, Jäger HR, Benavente OR, Werring DJ (2015) Cerebral micro bleeds and postthrombolysis intracerebral hemorrhage risk: updated meta-analysis. Neurology 11:927–4
Tsivgoulis G, Zand R, Katsanos AH, Turc G, Nolte CH, Jung S et al (2016) Risk of symptomatic intracerebral hemorrhage after intravenous thrombolysis in patients with acute ischemic stroke and high cerebral microbleed burden: a meta-analysis. JAMA Neurol 73(6):675–83
Seet RC, Rabinstein AA (2012) Symptomatic intracranial hemorrhage following intravenous thrombolysis for acute ischemic stroke: a critical review of case definitions. Cerebrovasc Dis 2:106–14
Nogueira RC, Bor-Seng-Shu E, Saeed NP, Teixeira MJ, Panerai RB, Robinson TG (2016) Meta-analysis of vascular imaging features to predict outcome following intravenous rtPA for acute ischemic stroke. Front Neurol 7:77
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM et al (2016) Endovascular thrombectomy after large vessel ischaemic stroke: a meta-analysis of individual patient data from five randomized trials. Lancet 387(10029):1723–31
Shi ZS, Loh Y, Liebeskind DS, Saver JL, Gonzalez NR, Tateshima S, Jahan R, Feng L, Vespa PM, Starkman S et al (2012) Leukoaraiosis predicts parenchymal hematoma after mechanical thrombectomy in acute ischemic stroke. Stroke 43(7):1806–11
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that all human studies have been approved [data from a regional emergency stroke network health registry in the Rhône Valley, France—RESUVAL Stroke Network—with 5 stroke units (one academic stroke unit and 4 non-academic stroke units), covering a population of 3 million people authorized by the French Ministry of Healthcare, Registration number E-2012-069] and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We declare that all patients gave informed consent prior to inclusion in this study.
Conflict of interest
We declare that we have no conflict of interest.
Rights and permissions
About this article
Cite this article
Nighoghossian, N., Abbas, F., Cho, TH. et al. Impact of leukoaraiosis on parenchymal hemorrhage in elderly patients treated with thrombolysis. Neuroradiology 58, 961–967 (2016). https://doi.org/10.1007/s00234-016-1725-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-016-1725-7