Abstract
Introduction
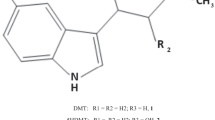
The present study was designed to investigate the rewarding effects induced by tramadol and its active metabolite O-desmethyltramadol (M1) under a neuropathic pain-like state.
Results
In opioid receptor binding and G protein activation, we confirmed that M1, but not tramadol, showed μ-opioid receptor (MOR) agonistic activity. Furthermore, we found that the subcutaneous (s.c.) injection of tramadol and M1 each produced a significant place preference in mice, and these effects were significantly suppressed by pretreatment with the MOR antagonist β-funaltrexamine. The dopamine level in the mouse nucleus accumbens was significantly increased by s.c. injection of either tramadol or M1. Mice with sciatic nerve ligation exhibited a marked decrease in the latency of paw withdrawal in response to a thermal stimulus only on the ipsilateral side. Under these neuropathic pain-like conditions, the rewarding effect induced by s.c. injection of either tramadol or M1 was dramatically inhibited after sciatic nerve ligation. Furthermore, the M1-induced G protein activation in the lower midbrain area was suppressed after sciatic nerve ligation.
Discussion
Our present data support the notion that the rewarding effect induced by tramadol is mediated mainly through metabolism to its active metabolite M1 via MOR. Furthermore, the suppression of the M1-induced G protein activation in the lower midbrain area caused by sciatic nerve ligation may be responsible for inhibiting the rewarding effects induced by s.c. injection of tramadol and M1 under a neuropathic pain-like state.







Similar content being viewed by others
References
Bamigbade TA, Davidson C, Langford RM, Stamford JA (1997) Action of tramadol, its enantiomers and principal metabolite, O-desmethyltramadol, on serotonin (5-HT) efflux and uptake in the rat dosal raphe nucleus. Br J Anaesth 79:352–356
Budd K (1994) Chronic pain-challenge and response. Drugs 47:33–38
Cicero TJ, Adams EH, Geller A, Inciardi JA, Munoz A, Schnoll SH, Senay EC, Woody GE (1999) A postmarketing surveillance program to monitor Ultram (tramadol hydrochloride) abuse in the United States. Drug Alcohol Depend 57:7–22
Desmeules JA, Piguet V, Collart L, Dayer P (1996) Contribution of monoaminergic modulation to the analgesic effect of tramadol. Br J Clin Pharmacol 41:7–12
Driessen B, Reimann W (1992) Interaction of the central analgesic, tramadol, with the uptake and release of 5-hydroxytryptamine in the rat brain in vitro. Br J Pharmacol 105:147–151
Epstein DH, Preston KL, Jasinski DR (2006) Abuse liability, behavioral pharmacology, and physical-dependence potential of opioids in humans and laboratory animals: lesson from tramadol. Biol Psychol 73(1):90–99
Garzon M, Pickel VM (2001) Plasmalemmal m-opioid receptor distribution mainly in nondopaminergic neurons in the rat ventral tegmental area. Synapse 41:311–328
Gibson TP (1996) Pharmacokinetics, efficacy, and safety of analgesia with a focus on tramadol HCl. Am J Med 101:47S–53S
Gillen C, Haurand M, Kobelt DJ, Wnendt S (2000) Affinity, potency and efficacy of tramadol and its metabolites at the cloned human m-opioid receptor. Naunyn-Schmiedebergs Arch Pharmakol 362:116–121
Ide S, Minami M, Ishihara K, Uhl GR, Sora I, Ikeda K (2006) Mu opioid receptor-dependent components in effects of tramadol. Neuropharmacology 51:651–658
Imai S, Narita M, Hashimoto S, Nakamura A, Miyoshi K, Nozaki H, Hareyama N, Takagi T, Suzuki M, Narita M, Suzuki T (2006) Differences in tolerance to anti-hyperalgesic effects between chronic treatment with morphine and fentanyl under the pain-like state. Japanese Journal of Psychopharmacology 26:183–192
Koob GF (1992) Drugs of abuse: anatomy, pharmacology and function of reward pathways. Trends Pharmacol Sci 13(5):177–184
Lemberg KK, Kontinen VK, Siiskonen AO, Viljakka KM, Yli-Kauhaluoma JT, Korpi ER, Kalso EA (2006) Antinociception by spinal and systemic oxycodone: why dose the route make a difference. Anesthesiology 105:801–812
Lintz W, Erlacin S, Frankus E, Uragg H (1981) Biotransformation of tramadol in man and animal. Arzneimittelforschung 31:1932–1943 (author’s translation)
Lintz W, Barth H, Becker R, Frankus E, Schmidt-Bothelt E (1998) Pharmacokinetics of tramadol and bioavailability of enteral tramadol formulations. 2nd communication: drops with ethanol. Arzneimittelforschung 48:436–447
Liu ZM, Zhou WH, Lian Z, Mu Y, Ren ZH, Cao JQ, Cai ZJ (1999) Drug dependence and abuse potential of tramadol. Zhongguo Yaoli Xuebao 20:52–54
Malmberg A, Basbaum AI (1998) Partial sciatic nerve injury in the mouse as a model of neuropathic pain: behavioral and neuroanatomical correlates. Pain 76:215–222
Mattia C, Coluzzi F (2005) Tramadol. Focus on musculoskeletal and neuropathic pain. Minerva Anestesiol 71:565–584
Mayer DJ, Mao J, Holt J, Price DD (1999) Cellular mechanisms of neuropathic pain, morphine tolerance, and their interactions. Proc Natl Acad USA 96:7731–7736
Narita M, Yajima Y, Aoki T, Ozaki S, Narita M, Mizoguchi H, Tseng LF, Suzuki T (2000) Up-regulation of the TrkB receptor in mice injured by the partial ligation of the sciatic nerve. Eur J Pharmacol 401:187–190
Narita M, Mizoguchi H, Suzuki T, Narita M, Dun NJ, Imai S, Yajima Y, Nagase H, Suzuki T, Tseng LF (2001a) Enhanced mu-opioid responses in the spinal cord of mice lacking protein kinase Cgamma isoform. J Biol Chem 276:15409–15414
Narita M, Funada M, Suzuki T (2001b) Regulation of opioid dependence by opioid receptor types. Pharmacol Ther 89:1–15
Narita M, Kishimoto Y, Ise Y, Yajima Y, Misawa K, Suzuki T (2005a) Direct evidence for the involvement of the mesolimbic kappa-opioid system in the morphine-induced rewarding effect under an inflammatory pain-like state. Neuropsychopharmacology 30:111–118
Narita M, Usui A, Narita M, Niikura K, Nozaki H, Khotib J, Nagumo Y, Yajima Y, Suzuki T (2005b) Protease-activated receptor-1 and platelet-derived growth factor in spinal cord neurons are implicated in neuropathic pain after nerve injury. J Neurosci 25:10000–10009
Narita M, Nakamura A, Ozaki M, Imai S, Miyoshi K, Suzuki M, Suzuki T (2007) Comparative pharmacological profiles of morphine and oxycodone under a neuropathic pain-like state in mice: evidence for less sensitivity to morphine. Neuropsycopharmacology 33:1097–1112
Nestler EJ (1996) Under siege: the brain on opiates. Neuron 16:897–900
Nichols ML, Michael DB, Ossipov MH, Lai J, Porreca F (1995) Regulation of morphine antiallodynic efficacy by cholecystokinin in a model of neuropathic pain in rats. J Pharmacol Exp Ther 275:1339–1345
Oe K, Narita M, Imai S, Shibasaki M, Kubota C, Kasukawa A, Hamaguchi M, Yajima Y, Yamazaki M, Suzuki T (2004) Inhibition of the morphine-induced rewarding effect by direct activation of spinal protein kinase C in mice. Psychopharmacology 177:55–60
Ozaki S, Narita M, Narita M, Iino M, Sugita J, Matsumura Y, Suzuki T (2002) Suppression of the morphine-induced rewarding effect in the rat with neuropathic pain: implication of the reduction in m-opioid receptor functions in the ventral tegmental area. J Neurochem 82:1192–1198
Ozaki S, Narita M, Narita M, Iino M, Miyoshi K, Suzuki T (2003) Suppression of the morphine-induced rewarding effect and G-protein activation in the lower midbrain following nerve injury in the mouse: involvement of G-protein-coupled receptor kinase2. Neuroscience 116:89–97
Ozaki S, Narita M, Narita M, Ozaki M, Khotib J, Suzuki T (2004) Role of extracellular signal-regulated kinase in the ventaral tegmental area in the suppression of the morphine-induced rewarding effect in mice with sciatic nerve ligation. J Neurochem 88:1389–1397
Paxinos G, Franklin KBJ (2001) The mouse brain in stereotaxic coordinates, 2nd edn. Academic, San Diego
Peckham ME, Traynor JR (2006) Comparison of the antinociceptive response to morphine and morphine-like compounds in male and female Sprague–Dawley rats. J Pharmacol Exp Ther 316:1195–1201
Radbruch L, Grond S, Lehmann KA (1996) A risk-benefit assessment of tramadol in the management of pain. Drug Safety 15:8–29
Raffa RB (1996) A novel approach to the pharmacology of analgesics. Am J Med 101:40S–46S
Raffa RB (2008) Basic pharmacology relevant to drug abuse assessment: tramadol as example. J Clin Pharm Ther 33:101–108
Raffa RB, Friderichs E, Reimann W (1992) Opioid and nonpooioid components independently contribute to the mechanism of action of tramadol, an atypical opioid analgesic. J Pharmacol Exp Ther 260:275–285
Sagata K, Minami K, Yanagihara N (2002) Tramadol inhibits norepinephrine transporter function at desipramine-binding sites in cultured bovine adrenal medullary cells. Anesth Analg 94:901–906
Seltzer Z, Dubner R, Shi Y (1990) A novel behavioral model of neuropathic pain disorders produced in rats by partial sciatic nerve injury. Pain 43:205–218
Sprague JE, Leifheit M, Selken J, Milks MM, Kinder DH, Nichols DE (2002) In vivo microdialysis and conditioned place preference studies in rats are consistent with abuse potential of tramadol. Synapse 43:118–121
Suzuki T (1996) Conditioned place preference in mice. Methods Find Exp Clin Pharmacol 18:75–83
Suzuki T, Kishimoto Y, Misawa M (1996) Formaline- and carrageenan-induced inflammation attenuates place preferences produced by morphine, methamphetamine and cocaine. Life Sci 59:1667–1674
Suzuki T, Kishimoto Y, Misawa M, Nagase H, Takeda F (1999) Role of the kappa-opioid system in the attenuation of the morphine-induced place preference under chronic pain. Life Sci 64:PL1–PL7
Suzuki T, Kishimoto Y, Ozaki S, Narita M (2001) Mechanism of opioid dependence and interaction between opioid receptors. Eur J Pain 5(Suppl A):63–65
Tzschentke TM, Bruckman W, Friderichs E (2002) Lack of sensitization during place conditioning in rats is consistent with the low abuse potential of tramadol. Neurosci Lett 23:25–28
Vaccarino AL, Marek P, Kest B, Ben-Eliyasu S, Couret LC Jr, Kao B, Liebeskind JC (1993) Morphine failes to produce tolerance when administered in the presence of formalin pain in rats. Brain Res 627:287–290
WHO Expert Committee on Drug Dependence (2006) World Health Organ Tech Rep Ser 942:1–21, 23–24
Yanagita T (1978) Drug dependence potential of 1-(m-methoxyphenyl)-2-dimethylaminomethyl)-cyclohexan-1-ol hydrochroride (tramadol) tasted in monkeys. Arzneimittelforschung 28:158–163
Yates WR, Nguyen MH, Warnock JK (2001) Tramadol dependence with no history of substance abuse. Am J Psychiatry 158:964
Zacny JP (2005) Profiling the subjective, psychomotor, and physiological effects of tramadol in recreational drug users. Drug Alcohol Depend 80:273–278
Acknowledgments
This work was supported in part by grants from the Ministry of Health, Labor and Welfare and the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Disclosure/conflict of interest
The authors declare that, except for the income received from their primary employer, no financial support or compensation has been received from any individual or corporate entity over the past 3 years for research or professional service and there are no personal financial holdings that could be perceived as constituting a potential conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Nakamura, A., Narita, M., Miyoshi, K. et al. Changes in the rewarding effects induced by tramadol and its active metabolite M1 after sciatic nerve injury in mice. Psychopharmacology 200, 307–316 (2008). https://doi.org/10.1007/s00213-008-1180-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-008-1180-1