Abstract
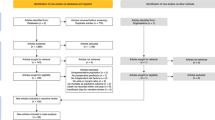
Introduction: To examine prognostic factors that influence complications after hip fracture surgery. To summarize proposed underlying mechanisms for their influence. Methods: We reported according to the Preferred Reporting Items for Systematic Review and Meta-Analysis Scoping Review extension. We searched MEDLINE, Embase, CINAHL, AgeLine, Cochrane Library, and reference lists of retrieved studies for studies of prognostic factor/s of postoperative in-hospital medical complication/s among patients 50 years and older treated surgically for non-pathological closed hip fracture, published in English on January 2008–January 2018. We excluded studies of surgery type or in-hospital medications. Screening was duplicated by two independent reviewers. One reviewer completed the extraction with accuracy checks by the second reviewer. We summarized the extent, nature, and proposed underlying mechanisms for the prognostic factors of complications narratively and in a dependency graph. Results: We identified 44 prognostic factors of in-hospital complications after hip fracture surgery from 56 studies. Of these, we identified 7 patient factors—dehydration, anemia, hypotension, heart rate variability, pressure risk, nutrition, and indwelling catheter use; and 7 process factors—time to surgery, anesthetic type, transfusion strategy, orthopedic versus geriatric/co-managed care, multidisciplinary care pathway, and potentially modifiable during index hospitalization. We identified underlying mechanisms for 15 of 44 factors. The reported association between 12 prognostic factors and complications was inconsistent across studies. Conclusions: Most factors were reported by one study with no proposed underlying mechanism for their influence. Where reported by more than one study, there was inconsistency in reported associations and the conceptualization of complications differed, limiting comparison across studies. It is therefore not possible to be certain whether intervening on these factors would reduce the rate of complications after hip fracture surgery.


Similar content being viewed by others
References
Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C, Epidemiology IOFWGo, Quality of L (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Johansen A, Tsang C, Boulton C, Wakeman R, Moppett I (2017) Understanding mortality rates after hip fracture repair using ASA physical status in the National Hip Fracture Database. Anaesthesia 72:961–966
Sobolev B, Guy P, Sheehan KJ et al (2016) Time trends in hospital stay after hip fracture in Canada, 2004–2012: database study. Arch Osteoporos 11:13
Nordstrom P, Gustafson Y, Michaelsson K, Nordstrom A (2015) Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ 350:h696
Sheehan KJ, Sobolev B, Chudyk A, Stephens T, Guy P (2016) Patient and system factors of mortality after hip fracture: a scoping review. BMC Musculoskelet Disord 17:166
Roche JJ, Wenn RT, Sahota O, Moran CG (2005) Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 331:1374
Silber JH, Williams SV (1992) Hospital and patient characteristics associated with death after surgery—a study of adverse occurrence and failure to rescue. Med Care 30:615–629
Tricco AC, Lillie E, Zarin W et al (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473
Covidence systematic review software. Veritas Health Innovation, Melbourne, Australia Available at www.covidence.org. Accessed 24 April 2019
Westreich D, Greenland S (2013) The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. Am J Epidemiol 177:292–298
Ferrari R (2015) Writing narrative style literature reviews. Medical Writing 24:230–235
Bernthaler A, Mühlberger I, Fechete R, Perco P, Lukas A, Mayer B (2009) A dependency graph approach for the analysis of differential gene expression profiles. Molecular Bio Systems 5:1720–1731
Kistler EA, Nicholas JA, Kates SL, Friedman SM (2015) Frailty and short-term outcomes in patients with hip fracture. Geriatr Orthop Surg Rehabil 6:209–214
Ryan DJ, Yoshihara H, Yoneoka D, Egol KA, Zuckerman JD (2015) Delay in hip fracture surgery: an analysis of patient-specific and hospital-specific risk factors. J Orthop Trauma 29:343–348
Eren Z, Ulucay C, Kaspar EC, Altintas F, Kantarci G (2012) Acute kidney injury after hip fracture surgery among aging population: evaluation of incidence and covariates. Eur Geriatr Med 3:345–348
Deschodt M, Braes T, Flamaing J, Detroyer E, Broos P, Haentjens P, Boonen S, Milisen K (2012) Preventing delirium in older adults with recent hip fracture through multidisciplinary geriatric consultation. J Am Geriatr Soc 60:733–739
Cohn MR, Levack AE, Trivedi NN, Villa JC, Wellman DS, Lyden JP, Lorich DG, Lane JM (2017) The hip fracture patient on warfarin: evaluating blood loss and time to surgery. J Orthop Trauma 31:407–413
Bennet SJ, Berry OM, Goddard J, Keating JF (2010) Acute renal dysfunction following hip fracture. Injury 41:335–338
Baumgarten M, Rich SE, Shardell MD et al (2012) Care-related risk factors for hospital-acquired pressure ulcers in elderly adults with hip fracture. J Am Geriatr Soc 60:277–283
Adunsky A, Nenaydenko O, Koren-Morag N, Puritz L, Fleissig Y, Arad M (2015) Perioperative urinary retention, short-term functional outcome and mortality rates of elderly hip fracture patients. Geriatr Gerontol Int 15:65–71
Freter S, Koller K, Dunbar M, MacKnight C, Rockwood K (2017) Translating delirium prevention strategies for elderly adults with hip fracture into routine clinical care: a pragmatic clinical trial. J Am Geriatr Soc 65:567–573
Guo Y, Zhang Y, Jia P et al (2017) Preoperative serum metabolites are associated with postoperative delirium in elderly hip-fracture patients. J Gerontol A Biol Sci Med Sci 72:1689–1696
Ji MH, Shen JC, Gao R, Liu XY, Yuan HM, Dong L, Wu J, Feng SW, Li WY, Yang JJ (2013) Early postoperative cognitive dysfunction is associated with higher cortisol levels in aged patients following hip fracture surgery. J Anesth 27:942–944
Juliebo V, Bjoro K, Krogseth M, Skovlund E, Ranhoff AH, Wyller TB (2009) Risk factors for preoperative and postoperative delirium in elderly patients with hip fracture. J Am Geriatr Soc 57:1354–1361
Lindholm C, Sterner E, Romanelli M et al (2008) Hip fracture and pressure ulcers—the Pan-European Pressure Ulcer Study—intrinsic and extrinsic risk factors. Int Wound J 5:315–328
Love AL, Cornwell PL, Whitehouse SL (2013) Oropharyngeal dysphagia in an elderly post-operative hip fracture population: a prospective cohort study. Age Ageing 42:782–785
Mazzola P, Ward L, Zazzetta S, Broggini V, Anzuini A, Valcarcel B, Brathwaite JS, Pasinetti GM, Bellelli G, Annoni G (2017) Association between preoperative malnutrition and postoperative delirium after hip fracture surgery in older adults. J Am Geriatr Soc 65:1222–1228
Nie H, Zhao B, Zhang YQ, Jiang YH, Yang YX (2012) Pain and cognitive dysfunction are the risk factors of delirium in elderly hip fracture Chinese patients. Arch Gerontol Geriatr 54:e172–e174
Oh ES, Sieber FE, Leoutsakos JM, Inouye SK, Lee HB (2016) Sex differences in hip fracture surgery: preoperative risk factors for delirium and postoperative outcomes. J Am Geriatr Soc 64:1616–1621
Radinovic K, Milan Z, Markovic-Denic L, Dubljanin-Raspopovic E, Jovanovic B, Bumbasirevic V (2014) Predictors of severe pain in the immediate postoperative period in elderly patients following hip fracture surgery. Injury 45:1246–1250
Scholtens RM, de Rooij SE, Vellekoop AE, Vrouenraets BC, van Munster BC (2016) Preoperative CSF melatonin concentrations and the occurrence of delirium in older hip fracture patients: a preliminary study. PLoS One 11:e0167621
Shin JE, Kyeong S, Lee JS, Park JY, Lee WS, Kim JJ, Yang KH (2016) A personality trait contributes to the occurrence of postoperative delirium: a prospective study. BMC Psychiatry 16:371
Tobu S, Noguchi M, Hashikawa T, Uozumi J (2014) Risk factors of postoperative urinary retention after hip surgery for femoral neck fracture in elderly women. Geriatr Gerontol Int 14:636–639
Ulucay C, Eren Z, Kaspar EC, Ozler T, Yuksel K, Kantarci G, Altintas F (2012) Risk factors for acute kidney injury after hip fracture surgery in the elderly individuals. Geriatr Orthop Surg Rehabil 3:150–156
van der Zanden V, Beishuizen SJ, Scholtens RM, de Jonghe A, de Rooij SE, van Munster BC (2016) The effects of blood transfusion on delirium incidence. J Am Med Dir Assoc 17:748–753
Van Grootven B, Detroyer E, Devriendt E, Sermon A, Deschodt M, Flamaing J, Dubois C, Milisen K (2016) Is preoperative state anxiety a risk factor for postoperative delirium among elderly hip fracture patients? Geriatr Gerontol Int 16:948–955
Wu Y, Shi Z, Wang M, Zhu Y, Li C, Li G, Marcantonio ER, Xie Z, Shen Y (2015) Different MMSE score is associated with postoperative delirium in young-old and old-old adults. PLoS One 10:e0139879
Batsis JA, Huddleston JM, Melton LJ 3rd, Huddleston PM, Larson DR, Gullerud RE, McMahon MM (2009) Body mass index (BMI) and risk of noncardiac postoperative medical complications in elderly hip fracture patients: a population-based study. J Hosp Med 4:E1–E9
Dawson-Bowling S, Chettiar K, Cottam H, Worth R, Forder J, Fitzgerald-O'Connor I, Walker D, Apthorp H (2008) Troponin T as a predictive marker of morbidity in patients with fractured neck of femur. Injury 39:775–780
Dubljanin-Raspopovic E, Markovic-Denic L, Matanovic D, Grajic M, Krstic N, Bumbasirevic M (2012) Is pre-fracture functional status better than cognitive level in predicting short-term outcome of elderly hip fracture patients. Arch Med Sci 8:115–122
van Wissen J, van Stijn MF, Doodeman HJ, Houdijk AP (2016) Mini nutritional assessment and mortality after hip fracture surgery in the elderly. J Nutr Health Aging 20:964–968
Manaqibwala MI, Butler KA, Sagebien CA (2014) Complications of hip fracture surgery on patients receiving clopidogrel therapy. Arch Orthop Trauma Surg 134:747–753
Anbar R, Beloosesky Y, Cohen J, Madar Z, Weiss A, Theilla M, Koren Hakim T, Frishman S, Singer P (2014) Tight calorie control in geriatric patients following hip fracture decreases complications: a randomized, controlled study. Clin Nutr 33:23–28
Coventry LS, Nguyen A, Karahalios A, Roshan-Zamir S, Tran P (2017) Comparison of 3 different perioperative care models for patients with hip fractures within 1 health service. Geriatr Orthop Surg Rehabil 8:87–93
Koskderelioglu A, Onder O, Gucuyener M, Altay T, Kayali C, Gedizlioglu M (2017) Screening for postoperative delirium in patients with acute hip fracture: assessment of predictive factors. Geriatr Gerontol Int 17:919–924
Bliemel C, Lechler P, Oberkircher L, Colcuc C, Balzer-Geldsetzer M, Dodel R, Ruchholtz S, Buecking B (2015) Effect of preexisting cognitive impairment on in-patient treatment and discharge management among elderly patients with hip fractures. Dement Geriatr Cogn Disord 40:33–43
Bliemel C, Oberkircher L, Eschbach DA, Lechler P, Balzer-Geldsetzer M, Ruchholtz S, Buecking B (2015) Impact of Parkinson's disease on the acute care treatment and medium-term functional outcome in geriatric hip fracture patients. Arch Orthop Trauma Surg 135:1519–1526
Chuang CH, Pinkowsky GJ, Hollenbeak CS, Armstrong AD (2010) Medicine versus orthopaedic service for hospital management of hip fractures. Clin Orthop Relat Res 468:2218–2223
Ernst G, Watne LO, Frihagen F, Wyller TB, Dominik A, Rostrup M (2017) Decreases in heart rate variability are associated with postoperative complications in hip fracture patients. PLoS One 12:e0180423
Foss NB, Kristensen MT, Jensen PS, Palm H, Krasheninnikoff M, Kehlet H (2009) The effects of liberal versus restrictive transfusion thresholds on ambulation after hip fracture surgery. Transfusion 49:227–234
Gold A, Sever R, Lerman Y, Salai M, Justo D (2012) Admission Norton scale scores (ANSS) and postoperative complications following hip fracture surgery in the elderly. Arch Gerontol Geriatr 55:173–176
Hirose J, Mizuta H, Ide J, Nakamura E, Takada K (2008) E-PASS for predicting postoperative risk with hip fracture: a multicenter study. Clin Orthop Relat Res 466:2833–2841
Hirose J, Mizuta H, Ide J, Nomura K (2008) Evaluation of estimation of physiologic ability and surgical stress (E-PASS) to predict the postoperative risk for hip fracture in elder patients. Arch Orthop Trauma Surg 128:1447–1452
Hossain FS, Rambani R, Ribee H, Koch L (2013) Is discontinuation of clopidogrel necessary for intracapsular hip fracture surgery? Analysis of 102 hemiarthroplasties. J Orthop Traumatol 14:171–177
Judd KT, Christianson E (2015) Expedited operative care of hip fractures results in significantly lower cost of treatment. Iowa Orthop J 35:62–64
Kalmet PH, Koc BB, Hemmes B et al (2016) Effectiveness of a multidisciplinary clinical pathway for elderly patients with hip fracture: a multicenter comparative cohort study. Geriatr Orthop Surg Rehabil 7:81–85
Katrancha ED, Zipf J, Abrahams N, Schroeder R (2017) Retrospective evaluation of the impact of a geriatric trauma institute on fragility hip fracture patient outcomes. Orthop Nurs 36:330–334
Kempegowda H, Richard R, Borade A et al (2017) Obesity is associated with high perioperative complications among surgically treated intertrochanteric fracture of the femur. J Orthop Trauma 31:352–357
Kim BH, Lee S, Yoo B, Lee WY, Lim Y, Kim MC, Yon JH, Kim KM (2015) Risk factors associated with outcomes of hip fracture surgery in elderly patients. Korean J Anesthesiol 68:561–567
Koval KJ, Rust CL, Spratt KF (2011) The effect of hospital setting and teaching status on outcomes after hip fracture. AmJ Orthop(BelleMead NJ) 40:19–28
Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM (2009) Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg Br 91:922–927
Mazzola P, De Filippi F, Castoldi G, Galetti P, Zatti G, Annoni G (2011) A comparison between two co-managed geriatric programmes for hip fractured elderly patients. Aging Clin Exp Res 23:431–436
Menzies IB, Mendelson DA, Kates SL, Friedman SM (2012) The impact of comorbidity on perioperative outcomes of hip fractures in a geriatric fracture model. Geriatr Orthop Surg Rehabil 3:129–134
Pimlott BJ, Jones CA, Beaupre LA, Johnston DW, Majumdar SR (2011) Prognostic impact of pre-operative albumin on short-term mortality and complications in patients with hip fracture. Arch Gerontol Geriatr 53:90–94
Switzer JA, Bennett RE, Wright DM, Vang S, Anderson CP, Vlasak AJ, Gammon SR (2013) Surgical time of day does not affect outcome following hip fracture fixation. Geriatr Orthop Surg Rehabil 4:109–116
Tsuda Y, Yasunaga H, Horiguchi H, Ogawa S, Kawano H, Tanaka S (2015) Association between dementia and postoperative complications after hip fracture surgery in the elderly: analysis of 87,654 patients using a national administrative database. Arch Orthop Trauma Surg 135:1511–1517
Verbeek DO, Ponsen KJ, Goslings JC, Heetveld MJ (2008) Effect of surgical delay on outcome in hip fracture patients: a retrospective multivariate analysis of 192 patients. Int Orthop 32:13–18
Vidan MT, Sanchez E, Gracia Y, Maranon E, Vaquero J, Serra JA (2011) Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med 155:226–233
Guay J, Parker MJ, Gajendragadkar PR, Kopp S (2016) Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev 2:CD000521
McInnes E, Jammali-Blasi A, Bell-Syer S, Dumville JC, Middleton V, Cullum N (2015) Support for pressure ulcer prevention. Cochrane Library. 9: CD001735
Devereaux, P.J (2013) HIP fracture Accelerated surgical TreaTment And Care tracK (HIP ATTACK) trial. ClinicalTrialsgov identifier: NCT01344343
Moran CG, Wenn RT, Sikand M, Taylor AM (2005) Early mortality after hip fracture: is delay before surgery important? JBone Joint SurgAm 87:483–489
Carson JL, Sieber F, Cook DR et al (2015) Liberal versus restrictive blood transfusion strategy: 3-year survival and cause of death results from the FOCUS randomised controlled trial. Lancet 385:1183–1189
Sheehan K, Williamson L, Alexander J, Filliter C, Sobolev B, Guy P, Bearne L, Sackley C (2017) Prognostic factors of functional outcome after hip fracture surgery: a systematic review. Age Ageing 47(5):661–670
Chaves PH, Semba RD, Leng SX, Woodman RC, Ferrucci L, Guralnik JM, Fried LP (2005) Impact of anemia and cardiovascular disease on frailty status of community-dwelling older women: the Women's Health and Aging Studies I and II. J Gerontol A Biol Sci Med Sci 60:729–735
Grigoryan KV, Javedan H, Rudolph JL (2014) Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma 28:e49–e55
Agency for Healthcare R, Quality (2015) AHRQ quality indicators: guide to patient safety indicators. Version 5.0. Agency for Healthcare Research and Quality, Rockville, MD
Chatterton BD, Moores TS, Ahmad S, Cattell A, Roberts PJ (2015) Cause of death and factors associated with early in-hospital mortality after hip fracture. Bone Joint J 97-B:246–251
Boereboom FT, Raymakers JA, Duursma SA (1992) Mortality and causes of death after hip fractures in The Netherlands. Neth J Med 41:4–10
Smith TO, Cooper A, Peryer G, Griffiths R, Fox C, Cross J (2017) Factors predicting incidence of post-operative delirium in older people following hip fracture surgery: a systematic review and meta-analysis. Int J Geriatr Psychiatry 32:386–396
Caillet P, Klemm S, Ducher M, Aussem A, Schott AM (2015) Hip fracture in the elderly: a re-analysis of the EPIDOS study with causal Bayesian networks. PLoSOne 10:e0120125
Sheehan KJ, Sobolev B, Guy P (2017) Mortality by timing of hip fracture surgery: factors and relationships at play. J Bone Joint Surg Am 99:e106
American College of Surgeons National Surgical Quality Improvement Program. (2018) https://www.facs.org/quality-programs/acs-nsqip. Accessed 24 April 2019
Levac D, Colquhoun H, O'Brien KK (2010) Scoping studies: advancing the methodology. Implement Sci 5:69
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Boris Sobolev and Pierre Guy report receiving grants from the Canadian Institutes of Health Research related to this work. Pierre Guy reports receiving grants from the Natural Sciences and Engineering Research Council of Canada, the Canadian Foundation for Innovation, and the British Columbia Specialists Services Committee for work regarding hip fracture care, outside the submitted work. He has also received fees from the BC Specialists Services Committee (for a provincial quality improvement project on redesign of hip fracture care) and from Stryker Orthopaedics (as a product development consultant), outside the submitted work. He is a board member and shareholder in Traumis Surgical Systems Inc. and a board member for the Canadian Orthopaedic Foundation. He also serves on the speakers’ bureaus of AOTrauma North America and Stryker Canada. Katie Jane Sheehan received funding from the National Institute for Health Research (NIHR) outside of the submitted work. Evan Guerrero, David Tainter, Brian Dial, Rhian Milton-Cole, James A Blair, James Alexander, Priti Swamy, Lisa Kuramoto, and Janet Pruv Bettger have no conflicts of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Sheehan, K., Guerrero, E., Tainter, D. et al. Prognostic factors of in-hospital complications after hip fracture surgery: a scoping review. Osteoporos Int 30, 1339–1351 (2019). https://doi.org/10.1007/s00198-019-04976-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04976-x