Abstract
Summary
Delayed discharges represent an inefficient use of acute hospital beds. Social isolation and referral to a public-funded rehabilitation unit were significant predictors of delayed discharges while admission from an institution was a protective factor for older hip fracture patients. Preventing delays could save between 11.2 and 30.7 % of total hospital costs for this patient group.
Introduction
Delayed discharges of older patients from acute care hospitals are a major challenge for administrative, humanitarian, and economic reasons. At the same time, older people are particularly vulnerable to social isolation which has a detrimental effect on their health and well-being with cost implications for health and social care services. The purpose of the present study was to determine the impact and costs of social isolation on delayed hospital discharge.
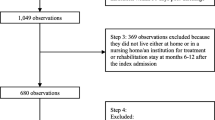
Methods
A prospective study of 278 consecutive patients aged 75 or older with hip fracture admitted, as an emergency, to the Orthopaedics Department of Hospital Universitário de Santa Maria, Portugal, was conducted. A logistic regression model was used to examine the impact of relevant covariates on delayed discharges, and a negative binomial regression model was used to examine the main drivers of days of delayed discharges. Costs of delayed discharges were estimated using unit costs from national databases.
Results
Mean age at admission was 85.5 years and mean length of stay was 13.1 days per patient. Sixty-two (22.3 %) patients had delayed discharges, resulting in 419 bed days lost (11.5 % of the total length of stay). Being isolated or at a high risk of social isolation, measured with the Lubben social network scale, was significantly associated with delayed discharges (odds ratio (OR) 3.5) as was being referred to a public-funded rehabilitation unit (OR 7.6). These two variables also increased the number of days of delayed discharges (2.6 and 4.9 extra days, respectively, holding all else constant). Patients who were admitted from an institution were less likely to have delayed discharges (OR 0.2) with 5.5 fewer days of delay. Total costs of delayed discharges were between 11.2 and 30.7 % of total costs (€2352 and €9317 per patient with delayed discharge) conditional on whether waiting costs for placement in public-funded rehabilitation unit were included.
Conclusion
High risk of social isolation, social isolation and referral to public-funded rehabilitation units increase delays in patients’ discharges from acute care hospitals.
Similar content being viewed by others
References
United Nations Department of Economic and Social Affairs. (2013) World population prospects: the 2012 revision, volume I: comprehensive tables. New York
Casey B, Oxley H, Whitehouse E et al (2003) Policies for an ageing society: recent measures and areas for future reform. OECD, Paris
Spillman BC, Lubitz J (2000) The effect of longevity on spending for acute and long-term care. N Engl J Med 342(19):1409–1415. doi:10.1056/NEJM200005113421906
Suarez Garcia F (2001) Oterino de la Fuente D, Peiro S, et al. Factors associated with hospitalization use and appropriateness for patients over 64 years of age. [Spanish]. Rev Esp Salud Publica 75(3):237–248
Department of Health. (2001) National service framework for older people. London
Gray LC, Yeo MA, Duckett SJ (2004) Trends in the use of hospital beds by older people in Australia: 1993-2002. Med J Aust 181(9):478–481
Irish Medical Organisation. (2005) IMO position paper on Acute Hospital Bed Capacity: Irish Medical Organisation
Becchi MA, Pescetelli M, Caiti O et al (2010) Characteristics of patients in a ward of Academic Internal Medicine: implications for medical care, training programmes and research. Intern Emerg Med 5(3):205–213. doi:10.1007/s11739-009-0325-5
Edirimanne S, Roake JA, Lewis DR (2010) Delays in discharge of vascular surgical patients: a prospective audit. ANZ J Surg 80:443–446. doi:10.1111/j.1445-2197.2009.05130.x
Foer D, Ornstein K, Soriano TA et al (2012) Nonmedical factors associated with prolonged hospital length of stay in an urban homebound population. J Hosp Med 7(2):73–78
Mohammed A (2001) Audit of orthopaedic bed utilisation. Health Bull 59(6):353–355
Lefevre F, Feinglass J, Potts S et al (1992) Iatrogenic complications in high-risk, elderly patients. Arch Intern Med 152(10):2074–2080
Giraud T, Dhainaut JF, Vaxelaire JF et al (1993) Iatrogenic complications in adult intensive care units: a prospective two-center study. Crit Care Med 21(1):40–51
Kohli HS, Bhaskaran MC, Muthukumar T et al (2000) Treatment-related acute renal failure in the elderly: a hospital-based prospective study. Nephrol Dial Transplant 15(2):212–217
McFarland LV (1995) Epidemiology of infectious and iatrogenic nosocomial diarrhea in a cohort of general medicine patients. Am J Infect Control 23(5):295–305
Tepp J, Voitk A (1999) Hip fracture as a complication of hospitalization. Int J Health Care Qual Assur Inc Leadersh Health Serv 12(6-7):10–13
Creditor MC (1993) Hazards of Hospitalization of the Elderly. Ann Intern Med 118(3):219–223
Hirsch CH, Sommers L, Olsen A et al (1990) The natural history of functional morbidity in hospitalized older patients. J Am Geriatr Soc 38(12):1296–1303
Sager MA, Franke T, Inouye SK et al (1996) Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 156(6):645–652
Sager MA, Rudberg MA, Jalaluddin M et al (1996) Hospital admission risk profile (HARP): identifying older patients at risk for functional decline following acute medical illness and hospitalization. J Am Geriatr Soc 44(3):251–257
Kozyrskyj AL, Black C, Chateau D et al (2005) Discharge outcomes in seniors hospitalized for more than 30 days. Can J Aging-Revue Canadienne Du Vieillissement 24:107–119. doi:10.1353/cja.2005.0048
Mayo NE, Wood-Dauphinee S, Gayton D et al (1997) Nonmedical bed-days for stroke patients admitted to acute-care hospitals in Montreal, Canada. Stroke 28(3):543–549
Hinchliffe D (2002) Delayed discharges
Hawkley LC, Cacioppo JT (2010) Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med 40:218–227
Kharicha K, Iliffe S, Harari D et al (2007) Health risk appraisal in older people 1: are older people living alone an “at-risk” group? Br J Gen Pract 57:271–276
Tivis RS, Laitala V, Routasalo PE et al (2011) Suffering from loneliness indicates significant mortality risk of older people. J Aging Res
Geller J, Janson P, McGovern E et al (1999) Loneliness as a predictor of hospital emergency department use. J Fam Pract 48(12):801–804
Iliffe S, Kharicha K, Harari D et al (2001) Health risk appraisal in older people 2: the implications for clinicians and commissioners of social isolation risk in older people. Br J Gen Pract 57:277–282
The Scottish Government (2004) Research review on tackling delayed discharge
Lim SC, Doshi V, Castasus B et al (2006) Factors causing delay in discharge of elderly patients in an acute care hospital. Ann Acad Med Singap 35:27–32
Lubben N (1988) Assessing social network among elderly population. Fam Community Health 11:42–52
Administração central de sistemas de saúde. Base de dados de elementos analíticos
Instituto da Segurança Social IP, Departamento de Planeamento e Sistemas de Informação. (2006) Custos reais das respostas sociais desenvolvidas pelo sector solidário:155
European Commission - Eurostat: annual gross average earnings. (2008-2011) Secondary. http://epp.eurostat.ec.europa.eu/statistics_explained/index.php?title=File:Table1_Average_Gross_annual_Earnings_in_the_business_economy_(full-time_employees),_2008-2011.png&filetimestamp=20130619135352
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Bianco A, Pileggi C, Rizza P et al (2006) An assessment of inappropriate hospital bed utilization by elderly patients in southern Italy. Aging Clin Exp Res 18(3):249–256
Chin JJ, Sahadevan S, Tan CY et al (2001) Critical role of functional decline in delayed discharge from an acute geriatric unit. Ann Acad Med Singap 30(6):593–599
Ingold BB, Yersin B, Wietlisbach V et al (2000) Characteristics associated with inappropriate hospital use in elderly patients admitted to a general internal medicine service. Aging Clin Exp Res 12(6):430–438
Victor C, Healy J, Thomas A et al (2000) Older patients and delayed discharges. Health Soc Care Community 8(6):443–452
Melo M, Ferreira P, Melo P, et al. Disparidades de género no mercado de trabalho português. Secondary Disparidades de género no mercado de trabalho português. http://pascal.iseg.utl.pt/~mclopes/ERHSITE.pdf
Martins PS, Novo AA, Portugal P. Increasing the Legal Retirement Age: The Impact on Wages, Worker Flows and Firm Performance Discussion Paper No 4187 2009;IZA
Carneiro R, Chau F, Soares C et al O Envelhecimento da População: Dependência, Ativação e Qualidade Centro de estudos dos povos e culturas de expressão portuguesa, Faculdade de Ciências Humanas da Universidade Católica Portuguesa
Cooper B, Mahnkopf B (1984) H B. Psychiatric disease and social isolation in elderly nursing home residents: a comparative study. Z Gerontol 17(3):117–125
Royal College of Physicians (2014) Falls and fragility fracture audit programme: national hip fracture database extended report
Ministério das Finanças da Saúde e da Solidariedade Emprego e Segurança Social. Portaria n.° 360/2013 de 16 de dezembro
Gertman PM, Restuccia JD (1981) The appropriateness evaluation protocol: a technique for assessing unnecessary days of hospital care. Med Care 19(8):855–871
Acknowledgments
The authors would like to thank Professor Jacinto Monteiro for allowing the study to be conducted in the Orthopedics Service of Hospital de Santa Maria and for his help and constructive comments. We also wish to thank Dr. Joaquim Soares do Brito, for his helpful collaboration as a participating investigator during the data collection process, and for providing useful comments. We would also like to gratefully acknowledge the help of Ana Maximiano, Renata Gomes, José Miranda and Tânia Fernandes in the gathering of social care data, and Clara Alves and Anabela Matos in identifying patients to take part in the study. Finally, we would like to thank Seamus Kent for discussing this paper at the 2014 joint congress of the International Health Economics Association and European Conference on Health Economics, and to both Seamus Kent and Dr. Wei Han for providing valuable feedback. Filipa Landeiro is sponsored by Fundação para a Ciência e Tecnologia, I.P. (SFRH / BD / 90910 / 2012, financed by POPH-QREN) and Instituto do Envelhecimento – Universidade de Lisboa.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments on comparable ethical standards.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 29.9 KB)
Rights and permissions
About this article
Cite this article
Landeiro, F., Leal, J. & Gray, A.M. The impact of social isolation on delayed hospital discharges of older hip fracture patients and associated costs. Osteoporos Int 27, 737–745 (2016). https://doi.org/10.1007/s00198-015-3293-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3293-9