Abstract
Purpose
The purpose of this study was to assess which factors were associated with the implementation of “Choosing Wisely” recommendations to refrain from routine MRI and arthroscopy use in degenerative knee disease.
Methods
Cross-sectional surveys were sent to 123 patients (response rate 95%) and 413 orthopaedic surgeons (response rate 62%) fulfilling the inclusion criteria. Univariate and multivariate logistic regression analyses were used to identify factors associated with implementation of “Choosing Wisely” recommendations.
Results
Factors reducing implementation of the MRI recommendation among patients included explanation of added value by an orthopaedic surgeon [OR 0.18 (95% CI 0.07–0.47)] and patient preference for MRI [OR 0.27 (95% CI 0.08–0.92)]. Factors reducing implementation among orthopaedic surgeons were higher valuation of own MRI experience than existing evidence [OR 0.41 (95% CI 0.19–0.88)] and higher estimated patients’ knowledge to participate in shared decision-making [OR 0.38 (95% CI 0.17–0.88)]. Factors reducing implementation of the arthroscopy recommendation among patients were orthopaedic surgeons’ preferences for an arthroscopy [OR 0.03 (95% CI 0.00–0.22)] and positive experiences with arthroscopy of friends/family [OR 0.03 (95% CI 0.00–0.39)]. Factors reducing implementation among orthopaedic surgeons were higher valuation of own arthroscopy experience than existing evidence [OR 0.17 (95% CI 0.07–0.46)] and belief in the added value [OR 0.28 (95% CI 0.10–0.81)].
Conclusions
Implementation of “Choosing Wisely” recommendations in degenerative knee disease can be improved by strategies to change clinician beliefs about the added value of MRIs and arthroscopies, and by patient-directed strategies addressing patient preferences and underlying beliefs for added value of MRI and arthroscopies resulting from experiences of people in their environment.
Level of evidence
IV.
Similar content being viewed by others
Introduction
Approximately, 25% of patients aged 50 years and over experience knee symptoms from degenerative knee disease [37, 41]. These patients suffer from pain during walking, climbing stairs and squatting, and have functional loss [15, 26]. In some cases, knee range of motion is limited due to a meniscal tear, also known as locking symptoms. These degenerative meniscal tears could be symptoms of early stage osteoarthritis [18, 19].
For diagnosing patients with degenerative knee disease, clinical practice guidelines [2, 4, 7, 8] and literature recommend weight-bearing radiographs (fixed flexion view—Rosenberg view) to determine the presence and severity of degenerative knee disease and to exclude other causes of knee pain, such as osteonecrosis of the femoral condyle or tibial plateau [18, 45]. Although MRI has high sensitivity and specificity in detecting meniscal tears in older patients [18, 39], routine use of MRI is not recommended for diagnosis because of the poor correlation with patient symptoms [14, 19, 20, 33]. Similarly, clinical practice guidelines do not recommend the use of arthroscopic surgery as there is no benefit shown of arthroscopic surgery over non-surgical treatments such as exercise therapy, analgesic medication and dietary advice [2, 17, 18, 27, 29,30,31, 37, 38, 43, 44]. If locking symptoms are present, or if pain is not reduced after non-surgical treatments, arthroscopy may be warranted. So, MRI and arthroscopic surgery without prior conservative management in degenerative knee disease can be considered as unnecessary or low value care as these provide no benefit for the patient, waste resources and may even cause harm to the patient [17, 35].
Although practice guidelines and the underlying evidence do not recommend routine use of MRI and arthroscopy, many patients aged 50 years and over with degenerative knee disease receive an MRI and/or a knee arthroscopy [9, 13, 16, 17, 24, 28, 32, 40]. Arthroscopic knee surgery is even the most common orthopaedic procedure in countries with available data and is, on a global scale, performed more than two million times each year [37].
In an effort to reduce the unnecessary use of MRIs and knee arthroscopies for patients with degenerative knee disease, medical societies in several countries have formulated “Choosing Wisely” recommendations regarding their use [1, 3, 6, 10]. A recent study of Rosenberg et al. [34] showed that developing such recommendations does not necessarily eradicate low value care. To stimulate the implementation of the CW recommendations, interventions should be adapted to the factors associated with implementation of specific CW recommendations—in this case ‘do not order an MRI for suspected degenerative meniscal tears’ and ‘do not perform knee arthroscopy for patients with degenerative meniscal tears of degenerative knee disease without mechanical symptoms’ [42]. Previous research has suggested that conducting knee arthroscopies is driven by clinician beliefs in the effectiveness [24, 28], the need to meet patient expectations [12], perverse financial incentives for clinicians/hospitals [24, 28], fragmented clinical decision pathways [24], and insurance coverage [32]. However, no study has systematically studied factors influencing the implementation of these CW recommendations on degenerative knee complaints in patients of 50 years and older.
Therefore, the aim of this study is to investigate which factors are associated with implementation of CW recommendations among patients and orthopaedic surgeons in the Netherlands which aim to reduce the number of unnecessary MRIs and arthroscopies in patients aged 50 years and over with degenerative knee disease. Based on the previous research above, it was hypothesized that orthopaedic surgeons’ beliefs in the effectiveness of MRI and knee arthroscopy, the need to meet patient expectations, perverse financial incentives and insurance coverage all hamper the implementation of CW recommendations.
Materials and methods
To investigate which factors are associated with implementation of CW recommendations, cross-sectional online surveys were performed among Dutch patients ≥ 50 years with degenerative knee disease and orthopaedic surgeons specialized in knee pathology (members of Dutch Knee Society) throughout the Netherlands. In the Netherlands, patients with (suspected) degenerative knee disease first visit a general practitioner before being referred to an orthopaedic surgeon.
A literature search and semi-structured interviews among Dutch patients with degenerative knee disease (N = 3) and orthopaedic surgeons (N = 3) were performed to identify potential factors influencing implementation of CW recommendations regarding MRIs and arthroscopies in patients ≥ 50 years with degenerative knee disease. For the interviews, purposive sampling was applied to obtain contrasting views, thereby identifying a broad spectrum of potential factors. Patients ≥ 50 years with degenerative knee problems who did and did not have an MRI and/or arthroscopy, and orthopaedic surgeons who either do or do not perform an MRI and/or arthroscopy in these patients were selected. The interview questions were based on the framework of Grol and Wensing [23]. This framework distinguishes factors influencing implementation at the following six levels: (a) innovation, (b) individual professional, (c) patient, (d) social context, (e) organisational context as well as the (f) economic and political context.
The semi-structured interviews were audio-taped, fully transcribed and analysed using open coding. The qualitative analysis was performed using the software program ATLAS.ti (version 7.5.16). A total of 55 factors were identified from the literature [21, 22, 25, 36, 46] for orthopaedic surgeons and patients. Besides, four factors were added based on the interviews among orthopaedic surgeons and patients. Overall, 59 factors were found, 26 for the patient and 33 for the orthopaedic surgeon.
Survey for patients
The survey included items about (1) background characteristics, (2) characteristics of the received care and (3) factors influencing implementation of the CW recommendations regarding MRI and arthroscopy. The items of these first two categories are given in “Appendix 1: Items survey patient”. The third part of the survey about factors influencing implementation of the CW recommendations consisted of 26 items identified in the interviews and literature. Answers could be given on a 4-point Likert scale, ranging from “totally agree” (coded 1) to “totally disagree” (coded 4) and some questions could be answered with yes/no. If the patient underwent an MRI or arthroscopy, additional questions followed, for example on waiting time.
Population
Patients were recruited via advertisements in newspapers and on websites of patient organisations. Assuming a baseline implementation rate of 15% in those with a certain barrier for implementation, sample size calculations showed that at least 120 patients would be needed to be able to detect a twofold increase odds in those without the barrier with 80% power and 95% reliability. The developed survey was sent to a sample of patients with degenerative knee disease (N = 138). Inclusion criteria were: age ≥ 50 years; degenerative knee disease; consultation with an orthopaedic surgeon for their degenerative knee disease. Patients on a waiting list for a total knee arthroplasty (TKA) or who already received a TKA were excluded. Also, patients with an inability to understand written Dutch were excluded. If patients indicated that they preferred to fill in the survey on paper rather than online, they received a paper survey. Two reminders were sent in case of non-response, one after 6 and one 12 weeks after the initial invitation. Patients received a ten euro gift card as an incentive upon completion of the survey.
Survey for orthopaedic surgeons
The survey for orthopaedic surgeons included items regarding (1) background characteristics, (2) characteristics of care delivery and (3) factors influencing implementation of the CW recommendations. The items of these first two categories are given in “Appendix 2: Items survey orthopaedic surgeon”. The third part consisted of 33 items covering the factors influencing implementation of the CW recommendations for orthopaedic surgeons. Answers could be given on a 4-point Likert scale, ranging from “totally agree” (coded 1) to “totally disagree” (coded 4).
Population
All Dutch orthopaedic surgeons specialized in knee pathology listed with an email address in the registry of the Dutch Orthopaedic Association (NOV) were invited by email to participate in the current study (N = 422). Inclusion criterion was: treatment of patients ≥ 50 years with degenerative knee symptoms. This criterion was asked as the first question of the survey. Non-responders received two reminders, one after 2 weeks and another 4 weeks after the initial invitation.
The Medical Ethical Committee (CME P16.190/NV/nv) of the Leiden University Medical Center confirmed that ethical approval for this type of study was not required under Dutch law.
Statistical analysis
Data from all respondents who completed the survey and fulfilled the inclusion criteria were included in the analyses. Descriptive statistics were used to describe the background characteristics, the care received by the patients, and characteristics of the care delivery according to the orthopaedic surgeon. The factors influencing implementation were dichotomized into agree ‘1’ (totally agree and agree) and disagree ‘0’ (totally disagree and disagree), because of few observations in some categories of the original Likert scale. If patients had an MRI and/or an arthroscopy, implemented CW recommendation was coded as 0 (no) and as 1 (yes) otherwise.
For patients, univariate logistic regression analysis was first used to assess which background characteristics, received care and potential factor for implementation were associated with the implemented CW recommendation, with MRI and arthroscopy (‘1’ yes and ‘0’ no) as the dependent variable. A similar analysis was conducted for orthopaedic surgeons, with self-reported implementation of the MRI/arthroscopy recommendations (yes/no) as dependent variable and background characteristics, care delivery characteristics and the factors influencing implementation of the CW recommendations (agree/disagree) as independent variables.
In addition, for both patients and orthopaedic surgeons, a multivariate logistic regression analysis was performed including those background characteristics, characteristics of the received care/care delivery and the factors influencing the CW recommendations with a p value ≤ 0.10 in univariate analyses. All analyses were performed using the software package SPSS (IBM SPSS, version 23).
Results
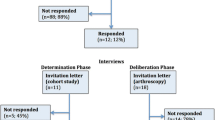
Of the 138 recruited patients, 131 completed the survey (response rate 95%). Fifteen were excluded because they did not fulfil the inclusion criteria (“Appendix 3: Flowcharts”). Of the 422 invited orthopaedic surgeons, 261 completed the survey (response rate 62%). Nine were excluded because they did not treat any patients ≥ 50 years with degenerative knee disease. Table 1 shows that the majority of the patients were female (61%) receiving higher education (47%), with average age 63.2 years. The majority of patients had additional coverage in their insurance (85%). In the Netherlands, patients are obliged to have a basic insurance with or without an additional coverage. The basic insurance has a mandatory excess of 385 euro. Patients who completed the survey represented the target group well, compared to the characteristics of Dutch orthopaedic patients [5]. Most of the orthopaedic surgeons who responded were male (90%), with an average age of 47.2 years and 12.0 years of working experience (Table 2). This was a realistic representation of the orthopaedic workforce in the Netherlands. The largest group worked in a general hospital (41%) in the middle region of the Netherlands (42%). Most of these orthopaedic surgeons saw more than 20 new patients per month (78%).
Factors influencing the use of MRI and arthroscopy among patients
Table 3 shows that most patients agreed with the statements “Good contact with physical therapist helped me to persevere the physical therapy treatments” (90%), “Good guidance of the physical therapist helped me to persevere all physical therapy treatments” (90%), “I have an additional coverage” (85%), and “Physical activity was difficult because of pain” (84%).
Table 4 shows that undergoing an MRI was associated with five barriers and two background characteristics among patients. Undergoing a knee arthroscopy was associated with five barriers, three facilitators and one background characteristic. From these, the orthopaedic surgeon’s explanation about the added value of an MRI [OR 0.18 (95% CI 0.07–0.47)] and the preference of the patient for an MRI [OR 0.27 (95% CI 0.08–0.92)] remained as independent factors associated with reduced implementation of the CW recommendation regarding MRI, whereas a higher age [OR 1.07 (95% CI 1.01–1.14)] was associated with higher implementation. For arthroscopy, the preference of the orthopaedic surgeon for arthroscopy [OR 0.03 (95% CI 0.00–0.22)] and positive experiences of people in the patient’s environment [OR 0.03 (95% CI 0.00–0.39)] remained as independent factors associated with reduced implementation of the CW recommendation regarding arthroscopy.
Factors influencing the use of MRI and arthroscopy among orthopaedic surgeons
Table 5 shows that most orthopaedic surgeons agreed with the statements “asking questions about the previous non-surgical treatments” (98%), the familiarity with the CW recommendation for MRI (99%) and arthroscopy (98%) as influential factors for implementation.
Table 6 shows that implementation of the CW recommendation regarding MRI was associated with four barriers and six facilitators among orthopaedic surgeons in univariate analysis. Implementation of the CW recommendation regarding arthroscopy was associated with two barriers, five facilitators and three background characteristics. From these, agreement with the CW recommendation regarding MRI [OR 12.10 (95% CI 3.51–41.64)] remained as an independent factor associated with higher implementation of the CW recommendation in multivariate analysis, whereas higher valuation of own experience than existing evidence [OR 0.41 (95% CI 0.19–0.88)] and higher estimated patients’ knowledge to participate in shared decision-making [OR 0.38 (95% CI 0.17–0.88)] were associated with reduced implementation. Knowledge of [OR 58.17 (95% CI 2.63–1287.24)] and agreement with the CW recommendations regarding arthroscopy [OR 37.45 (95% 5.39–260.24)] as well as actively searching for newest evidence and guidelines [OR 3.28 (95% CI 1.19–9.08)] were associated with higher implementation of the CW recommendation regarding arthroscopy, whereas higher valuation of own experience than existing evidence [OR 0.17 (95% CI 0.07–0.46)] and belief in the value of arthroscopy [OR 0.28 (95% CI 0.10–0.81)] were associated with reduced implementation.
Discussion
That the implementation of CW recommendations to reduce unnecessary MRIs and knee arthroscopies was hampered by patient preferences for MRI, positive experiences with arthroscopies in the patient’s environment, orthopaedic surgeons’ preferences for arthroscopy and their beliefs in the added value as well as valuing their own clinical experience to be more important than existing evidence were the most important findings of this study. On the other hand, orthopaedic surgeons’ knowledge of and agreement with the CW recommendations, as well as a proactive attitude towards searching for new evidence and guidelines facilitate implementation. Furthermore, older age of patients increased implementation of CW recommendations regarding MRI.
Previous studies were limited in only presenting the clinician perspective and mentioned clinician beliefs in the effectiveness of arthroscopic surgery [24, 28], clinicians’ need to meet patient expectations [12], perverse financial incentives [24, 28], fragmented clinical decision pathways [24] and insurance coverage [32] as possible barriers for implementation of CW recommendations regarding MRI and arthroscopy in degenerative knee disease. Our study results confirm that clinician beliefs hamper implementation, but perverse financial incentives for clinicians/hospitals, fragmented clinical decision pathways, and insurance coverage were not identified as barriers. Possibly, this can be explained by a different health-care system in which the studies are performed. In this study only 7% of the orthopaedic surgeons felt pressure to perform MRIs and arthroscopies because of production agreements and 75% of the orthopaedic surgeons reported that they were able to make clear agreements with GPs, physical therapists and dieticians about care delivery (Table 5). Furthermore, in this study 85% of the patients have reported that they have additional coverage for physical therapy treatment (Table 1).
Previous studies also showed that clinicians felt CW recommendations were hard to accept for patients [46], were worried about malpractice claims and did not have enough time to discuss the risks and benefits of imaging with the patient [36]. Around 70% of the orthopaedic surgeons reported in this survey that they thought patients had difficulties in accepting the CW recommendations (Table 5), but these were not independently associated with implementation in multivariate regression analyses. In addition, fear of malpractice claims and lack of time to discuss risks and benefits of imaging with the patients were also not found to hamper implementation: less than 11% of the orthopaedic surgeons felt they needed to request an MRI or perform an arthroscopy for medicolegal substantiation (Table 5). Sixty-six percent of orthopaedic surgeons reported they had enough time to explain treatment options to patients (Table 5) and 69% of the patients felt that their orthopaedic surgeon spent sufficient time to explain treatment options including risks and benefits (Table 3). This underlines the importance of assessment of factors influencing the implementation of every CW recommendation for different countries and also to include both the clinician and the patient perspective.
That the implementation of CW recommendations can also be influenced by patients was shown by this study, in addition to other studies. While previous studies regarding the use of MRI and arthroscopies in degenerative knee disease mainly mentioned clinician-related barriers [24, 28], it was shown by this study that also patients’ preferences for MRIs and positive experiences of people in their environment with arthroscopies hampered implementation of the CW recommendations. This is an important finding for future initiatives to improve implementation of CW recommendations. These should include both patient- and orthopaedic surgeon-directed strategies.
Implications for clinical practice are that the use of unnecessary MRIs and knee arthroscopy for patients with degenerative knee disease can potentially be reduced by strategies tailored to the identified barriers for implementation of the CW recommendations [11]. This reduction is of great importance as MRIs and arthroscopies for patients with degenerative knees provide no benefit for the patient, waste resources and may even cause harm to the patient [17, 35].
Although this study identified important starting points for improving implementation of CW recommendations, there are also limitations. First, only three patients and three orthopaedic surgeons were interviewed for survey development. However, after the second interview with the orthopaedic surgeon, no new information was obtained so more interviews were not required. Besides, the interviews were only used to explore if other factors should be included in the survey than already found in the literature. The second limitation is the retrospective nature of this study and the use of self-reported questions. Both patients and orthopaedic surgeons were asked to report the characteristics of received care/care delivery and barriers/facilitators retrospectively, and the use of CW recommendation. Therefore, it is possible that some patients and orthopaedic surgeons were not able to fully recall their respective care trajectory and provided care. Third, patients were self-selected after seeing the advertisements in the newspapers or on the websites, which may have caused selection bias. However, it seems that the patients who completed the survey represented the target group well [5].
Conclusions
The identified factors give important starting points for improving implementation of the CW recommendations regarding MRIs and arthroscopies in degenerative knee disease. It seems important to search for strategies to change clinician beliefs on the added value of arthroscopies and MRIs. Moreover, these strategies should focus on the importance of clinical experiences based on evidence. Furthermore, patient-directed strategies are needed to address patient ‘subjective’ preferences based on social feedback from environment and social media. These may add to underlying misbeliefs on the value of MRI and arthroscopies in degenerative knee disease.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- CW:
-
Choosing Wisely
References
American Medical Society for Sports Medicine (2014) Five things physicians and patients should question. http://www.choosingwisely.org/societies/american-medical-society-for-sports-medicine/. Accessed 13 Feb 2019
Arthroscopy of the knee (in Dutch) (2019) https://richtlijnendatabase.nl/richtlijn/artroscopie_van_de_knie/startpagina_-_artroscopie_van_de_knie.html. Accessed 13 Feb 2019
Australian Rheumatology Association (2018) tests, treatments and procedures clinicians and consumers should question. http://www.choosingwisely.org.au/recommendations/ara. Accessed 13 Feb 2019
ESSKA Meniscus Consensus Project (2016) Degenerative meniscus lesions. https://cdn.ymaws.com/www.esska.org/resource/resmgr/Docs/2016-meniscus-consensus-proj.pdf. Accessed 13 Feb 2019
Medical specialist care (2018) Diagnosis treatment combination (DTC) to diagnosis (in Dutch). https://opendata.cbs.nl/statline/#/CBS/nl/dataset/82470NED/table?ts=1540560239360. Accessed 13 Feb 2019
Orthopaedics (2018) Ten things physicians and patients should question. https://choosingwiselycanada.org/orthopaedics/. Accessed 13 Feb 2019
Osteoarthritis: care and management 2014 https://www.nice.org.uk/guidance/cg177. Accessed 13 Feb 2019
VA/DoD Clinical Practice Guideline For The Non-Surgical Management of Hip and Knee Osteoarthritis (2014) https://www.healthquality.va.gov/guidelines/CD/OA/VADoDOACPGFINAL090214.pdf. Accessed 13 Feb 2019
Adelani MA, Harris AH, Bowe TR, Giori NJ (2016) Arthroscopy for knee osteoarthritis has not decreased after a clinical trial. Clin Orthop Relat Res 474:489–494
Al Sayah F, Williams B, Pederson JL, Majumdar SR, Johnson JA (2014) Health literacy and nurses’ communication with type 2 diabetes patients in primary care settings. Nurs Res 63:408–417
Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S et al (2015) Tailored interventions to address determinants of practice. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd005470.pub3
Barlow T, Plant CE (2015) Why we still perform arthroscopy in knee osteoarthritis: a multi-methods study. BMC Musculoskelet Disord 16:85
Bergkvist D, Dahlberg LE, Neuman P, Englund M (2016) Knee arthroscopies: who gets them, what does the radiologist report, and what does the surgeon find? An evaluation from southern Sweden. Acta Orthop 87:12–16
Bhattacharyya TMD, Gale DMD, Dewire PMD, Totterman SMD, Gale MEMD, McLaughlin SMPH et al (2003) The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Jt Surg Am 85:4–9
Bijlsma JW, Berenbaum F, Lafeber FP (2011) Osteoarthritis: an update with relevance for clinical practice. Lancet 377:2115–2126
Bohensky MA, Sundararajan V, Andrianopoulos N, de Steiger RN, Bucknill A, Kondogiannis CM et al (2012) Trends in elective knee arthroscopies in a population-based cohort, 2000–2009. Med J Aust 197:399–403
Brignardello-Petersen R, Guyatt G, Buchbinder R, Poolman R, Schandelmaier S, Chang Y et al (2017) Knee arthroscopy versus conservative management in patients with degenerative knee disease: a systematic review. BMJ Open 7:e016114
Buchbinder R, Harris IA, Sprowson A (2015) Management of degenerative meniscal tears and the role of surgery. BMJ 350:h2212
Englund M (2008) The role of the meniscus in osteoarthritis genesis. Rheum Dis Clin N Am 34:573–579
Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M et al (2008) Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med 359:1108–1115
Fleuren P, van Dommelen P, van Buren SV (2012) Measuring instrument for determinants of innovations (MIDI) (in dutch). Int J Qual Health Care 26:501–510
Flottorp SA, Oxman AD, Krause J, Musila NR, Wensing M, Godycki-Cwirko M et al (2013) A checklist for identifying determinants of practice: a systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement Sci 8:35
Grol R, Wensing M (2004) What drives change? Barriers to and incentives for achieving evidence-based practice. Med J Aust 180:S57–S60
Hamilton DF, Howie CR (2015) Knee arthroscopy: influence of systems for delivering healthcare on procedure rates. BMJ 351:h4720
Hofstede SN, Marang-van de Mheen PJ, Vliet Vlieland TP, van den Ende CH, Nelissen RG, van Bodegom-Vos L (2016) Barriers and facilitators associated with non-surgical treatment use for osteoarthritis patients in orthopaedic practice. PLoS One 11:e0147406
Hunter DJ, Bierma-Zeinstra S (2019) Osteoarthritis. Lancet 393:1745–1759
Ikuta F, Takahashi K, Hashimoto S, Mochizuki Y, Yuzawa Y, Inanami H et al (2019) Effect of physical therapy on early knee osteoarthritis with medial meniscal posterior tear assessed by MRI T2 mapping and 3D-to-2D registration technique: a prospective intervention study. Mod Rheumatol. https://doi.org/10.1080/14397595.2019.16461931-10
Jarvinen TL, Guyatt GH (2016) Arthroscopic surgery for knee pain. BMJ 354:i3934
Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL et al (2013) Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med 368:1675–1684
Khan M, Evaniew N, Bedi A, Ayeni OR, Bhandari M (2014) Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ 186:1057–1064
Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM (2016) Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with 2 year follow-up. BMJ 354:i3740
Muheim LLS, Senn O, Fruh M, Reich O, Rosemann T, Neuner-Jehle SM (2017) Inappropriate use of arthroscopic meniscal surgery in degenerative knee disease. Acta Orthop 88:550–555
Parent ME, Vezina F, Carrier N, Masetto A (2018) Indications for and clinical procedures resulting from magnetic resonance imaging of the knee in older patients: are we choosing wisely? Can Fam Physician 64:e126–e132
Rosenberg A, Agiro A, Gottlieb M, Barron J, Brady P, Liu Y et al (2015) Early trends among seven recommendations from the Choosing Wisely campaign. JAMA Intern Med 175:1913–1920
Scott IA, Duckett SJ (2015) In search of professional consensus in defining and reducing low-value care. Med J Aust 203:179–181
Sears ED, Caverly TJ, Kullgren JT et al (2016) Clinicians’ perceptions of barriers to avoiding inappropriate imaging for low back pain—knowing is not enough. JAMA Intern Med 176:1866–1868
Siemieniuk RAC, Harris IA, Agoritsas T, Poolman RW, Brignardello-Petersen R, Van de Velde S et al (2017) Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ 357:j1982
Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H et al (2013) Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 369:2515–2524
Subhas N, Sakamoto FA, Mariscalco MW, Polster JM, Obuchowski NA, Jones MH (2012) Accuracy of MRI in the diagnosis of meniscal tears in older patients. AJR Am J Roentgenol 198:W575–W580
Thorlund JB, Hare KB, Lohmander LS (2014) Large increase in arthroscopic meniscus surgery in the middle-aged and older population in Denmark from 2000 to 2011. Acta Orthop 85:287–292
Turkiewicz A, Gerhardsson de Verdier M, Engstrom G, Nilsson PM, Mellstrom C, Lohmander LS et al (2015) Prevalence of knee pain and knee OA in southern Sweden and the proportion that seeks medical care. Rheumatology (Oxford) 54:827–835
van Bodegom-Vos L, Davidoff F, Marang-van de Mheen PJ (2017) Implementation and de-implementation: two sides of the same coin? BMJ Qual Saf 26:495–501
van de Graaf VA, Noorduyn JCA, Willigenburg NW, Butter IK, de Gast A, Mol BW et al (2018) Effect of early surgery vs physical therapy on knee function among patients with nonobstructive meniscal tears: the escape randomized clinical trial. JAMA 320:1328–1337
Yim J-H, Seon J-K, Song E-K, Choi J-I, Kim M-C, Lee K-B et al (2013) A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med 41:1565–1570
Zhang W, Doherty M, Peat G, Bierma-Zeinstra MA, Arden NK, Bresnihan B et al (2010) EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 69:483–489
Zikmund-Fisher BJ, Kullgren JT, Fagerlin A, Klamerus ML, Bernstein SJ, Kerr EA (2017) Perceived barriers to implementing individual Choosing Wisely((R)) recommendations in two national surveys of primary care providers. J Gen Intern Med 32:210–217
Funding
This study was funded by the Netherlands Organization for Health Research and Development (ZonMw) Grant 8392010022. They have no role in the study design or analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This study was approved by the Medical Ethical Committee (CME P16.190/NV/nv) of the Leiden University Medical Center.
Informed consent
For this type of article, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1: Items survey patient
Background characteristics | |
|---|---|
Age | In years |
Gender | Male, female |
Region of residence | North (Friesland, Groningen, Flevoland, Noord-Holland, Drenthe, and Overijssel), middle (Zuid-Holland, Utrecht, and Gelderland) and south (Noord-Brabant, Zeeland, and Limburg) |
Education level | Basic education (no or only primary education), intermediate education (prevocational secondary education, senior secondary vocational training, senior secondary general education, pre-university education) or higher education (higher professional education or university (bachelor’s, master’s or PhD degree) |
Start of disease symptoms | 0–3 months, 3–6 months, 6–12 months, and > 1 year |
Diagnosis of locking symptoms by orthopaedic surgeon if patient received arthroscopy | Yes, no |
Pain before visiting an orthopaedic surgeon | Visual analogue scale (VAS) |
Pain at the moment of the survey | Visual analogue scale (VAS) |
Health insurance | Basic insurance or additional coveragea |
Characteristics of the received care | |
History of caregivers | General practitioner (GP), physical therapist, orthopaedic surgeon, dietitian, and/or other |
Received care modalities | MRI, arthroscopy and/or physical therapy (yes/no) |
Time between start of knee complaints and visiting the GP | < 1 week, 1–6 weeks, > 6 weeks, or no idea |
Waiting time between GP and orthopaedic surgeon | 1–2 weeks, 3–4 weeks, 5–6 weeks, more than 6 weeks, or no idea |
Waiting time MRI | 1–2 weeks, 3–4 weeks, 5–6 weeks, more than 6 weeks, or no idea, not applicable (NA) |
Waiting time arthroscopy | Waiting time arthroscopy (1–2 weeks, 3–4 weeks, 5–6 weeks, more than 6 weeks, or no idea, NA) |
Preferred and actual role of the patient in treatment decision-making process | Control Preference Scale (CPS) [17] |
Appendix 2: Items survey orthopaedic surgeon
Background characteristics | |
|---|---|
Age | |
Gender | Male, female |
Years of working experience | |
Work setting | University medical centre, teaching hospital, general hospital, independent treatment centre |
Work region | North (Friesland, Groningen, Flevoland, Noord-Holland, Drenthe, and Overijssel), middle (Zuid-Holland, Utrecht, and Gelderland), and south (Noord-Brabant, Zeeland, and Limburg) |
Number of new patients per month | |
Number of MRIs and arthroscopies per month | |
Percentage of patients undergoing an arthroscopy with locking symptoms | |
Characteristics of care delivery | |
Availability of MRI scan in hospital | Yes, no |
Waiting time MRI | 0–1 week, 1–2 weeks, 3–4 weeks, 4–5 weeks, or more than 5 weeks |
Waiting time arthroscopy | 0–1 week, 1–2 weeks, 3–4 weeks, 4–5 weeks, or more than 5 weeks |
Implementation of CW recommendation | 4-point Likert scale, ranging from “totally agree” (coded 1) till “totally disagree” (coded 4) |
Appendix 3: Flowcharts

Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rietbergen, T., Diercks, R.L., Anker-van der Wel, I. et al. Preferences and beliefs of Dutch orthopaedic surgeons and patients reduce the implementation of “Choosing Wisely” recommendations in degenerative knee disease. Knee Surg Sports Traumatol Arthrosc 28, 3101–3117 (2020). https://doi.org/10.1007/s00167-019-05708-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05708-8