Abstract
Purpose
To assess the effect of systemic corticosteroids on the incidence of gastrointestinal bleeding in adult critically ill patients.
Methods
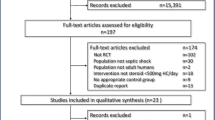
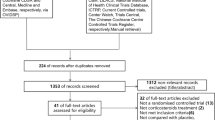
We systematically reviewed randomised clinical trials comparing systemic corticosteroids administered for more than 24 h with placebo/no treatment in adult critically ill patients. Trial selection, data abstraction and risk of bias assessments were performed in duplicate. We used trial sequential analysis (TSA) to assess the risk of random errors and the grading of recommendations, assessment, development, and evaluations (GRADE) approach to assess the quality of evidence. The primary outcome was the incidence of clinically important gastrointestinal bleeding within 90 days. The secondary outcome was the incidence of gastrointestinal bleeding of any severity within 90 days.
Results
Twenty-five trials (n = 14,615) reported data for the primary outcome and 55 trials (n = 21,792) for the secondary outcome. The pooled incidence of clinically important gastrointestinal bleeding was 2.3% in the corticosteroid group and 1.8% in the control group (RR, 1.26; 95% CI, 1.01–1.57; I2 = 0%, TSA-adjusted CI 0.51–3.14). We observed no difference in the risk of gastrointestinal bleeding of any severity (RR, 1.10; 95% CI, 0.92–1.32; I2 = 0%, TSA-adjusted CI 0.87–1.38). The GRADE quality of evidence was low (risk of bias and imprecision).
Conclusions
We observed an overall low incidence of clinically important gastrointestinal bleeding among adult critically ill patients. Corticosteroids may slightly increase the incidence of clinically important gastrointestinal bleeding, but not bleeding of any severity. Rarity of events, infrequent trial reporting and high risk of bias reduced the quality of evidence.


Similar content being viewed by others
Data availability
All data are freely available in the study and ESM.
References
Krag M, Perner A, Wetterslev J, Wise MP, Borthwick M, Bendel S, McArthur C, Cook D, Nielsen N, Pelosi P, Keus F, Guttormsen AB, Moller AD, Moller MH (2015) Prevalence and outcome of gastrointestinal bleeding and use of acid suppressants in acutely ill adult intensive care patients. Intensive Care Med 41:833–845
Cook DJ, Fuller HD, Guyatt GH, Marshall JC, Leasa D, Hall R, Winton TL, Rutledge F, Todd TJ, Roy P et al (1994) Risk factors for gastrointestinal bleeding in critically ill patients. N Engl J Med 330:377–381
MacLaren R, Reynolds PM, Allen RR (2014) Histamine-2 receptor antagonists vs proton pump inhibitors on gastrointestinal tract hemorrhage and infectious complications in the intensive care unit. JAMA Intern Med 174:564–574
Cook D, Heyland D, Griffith L, Cook R, Marshall J, Pagliarello J (1999) Risk factors for clinically important upper gastrointestinal bleeding in patients requiring mechanical ventilation. Crit Care Med 27:2812–2817
Cook DJ, Griffith LE, Walter SD, Guyatt GH, Meade MO, Heyland DK, Kirby A, Tryba M (2001) The attributable mortality and length of intensive care unit stay of clinically important gastrointestinal bleeding in critically ill patients. Crit Care 5:368–375
Pastores SM, Annane D, Rochwerg B (2018) Guidelines for the diagnosis and management of critical illness-related corticosteroid insufficiency (CIRCI) in critically ill patients (part II): Society of Critical Care Medicine (SCCM) and European Society of Intensive Care Medicine (ESICM) 2017. Intensive Care Med 44:474–477
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43:304–377
Annane D, Pastores SM, Rochwerg B, Arlt W, Balk RA, Beishuizen A, Briegel J, Carcillo J, Christ-Crain M, Cooper MS, Marik PE, Umberto Meduri G, Olsen KM, Rodgers SC, Russell JA, Van den Berghe G (2017) Guidelines for the diagnosis and management of critical illness-related corticosteroid insufficiency (CIRCI) in critically ill patients (part I): Society of Critical Care Medicine (SCCM) and European Society of Intensive Care Medicine (ESICM) 2017. Crit Care Med 45:2078–2088
Kiser TH, Allen RR, Valuck RJ, Moss M, Vandivier RW (2014) Outcomes associated with corticosteroid dosage in critically ill patients with acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 189:1052–1064
Butler E, Moller MH, Cook O, Granholm A, Penketh J, Rygard SL, Aneman A, Perner A (2018) Corticosteroids and risk of gastrointestinal bleeding in critically ill adults: protocol for a systematic review. Acta Anaesthesiol Scand 62:1321–1326
Wetterslev J, Jakobsen JC, Gluud C (2017) Trial sequential analysis in systematic reviews with meta-analysis. BMC Med Res Methodol 17:39
Higgins J, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration. Available from http://handbook.cochrane.org
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clin Res Ed) 339:b2700
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 349:g7647
Jakobsen JC, Wetterslev J, Winkel P, Lange T, Gluud C (2014) Thresholds for statistical and clinical significance in systematic reviews with meta-analytic methods. BMC Med Res Methodol 14:120
Friedrich JO, Adhikari NK, Beyene J (2007) Inclusion of zero total event trials in meta-analyses maintains analytic consistency and incorporates all available data. BMC Med Res Methodol 7:5
Møller CH, Penninga L, Wetterslev J, Steinbrüchel DA, Gluud C (2008) Clinical outcomes in randomized trials of off- vs. on-pump coronary artery bypass surgery: systematic review with meta-analyses and trial sequential analyses. Eur Heart J 29:2601–2616
Sweeting MJ, Sutton AJ, Lambert PC (2004) What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med 23:1351–1375
Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, Guyatt GH, Harbour RT, Haugh MC, Henry D, Hill S, Jaeschke R, Leng G, Liberati A, Magrini N, Mason J, Middleton P, Mrukowicz J, O’Connell D, Oxman AD, Phillips B, Schunemann HJ, Edejer T, Varonen H, Vist GE, Williams JW Jr, Zaza S, Group GW (2004) Grading quality of evidence and strength of recommendations. BMJ 328:1490
El-Ghamrawy AH, Shokier MH, AA E (2006) Effects of low-dose hydrocortisone in ICU patients with severe community-acquired pneumonia. Egypt J Chest Dis Tuberc 55:91–99
Gaab MR, Trost HA, Alcantara A, Karimi-Nejad A, Moskopp D, Schultheiss R, Bock WJ, Piek J, Klinge H, Scheil F et al (1994) “Ultrahigh” dexamethasone in acute brain injury. Results from a prospective randomized double-blind multicenter trial (GUDHIS). German Ultrahigh Dexamethasone Head Injury Study Group. Zentralbl Neurochir 55:135–143
Annane D, Renault A, Brun-Buisson C, Megarbane B, Quenot JP, Siami S, Cariou A, Forceville X, Schwebel C, Martin C, Timsit JF, Misset B, Ali Benali M, Colin G, Souweine B, Asehnoune K, Mercier E, Chimot L, Charpentier C, Francois B, Boulain T, Petitpas F, Constantin JM, Dhonneur G, Baudin F, Combes A, Bohe J, Loriferne JF, Amathieu R, Cook F, Slama M, Leroy O, Capellier G, Dargent A, Hissem T, Maxime V, Bellissant E (2018) Hydrocortisone plus fludrocortisone for adults with septic shock. N Engl J Med 378:809–818
Venkatesh B, Finfer S, Cohen J, Rajbhandari D, Arabi Y, Bellomo R, Billot L, Correa M, Glass P, Harward M, Joyce C, Li Q, McArthur C, Perner A, Rhodes A, Thompson K, Webb S, Myburgh J (2018) Adjunctive glucocorticoid therapy in patients with septic shock. N Engl J Med 378:797–808
Gordon AC, Mason AJ, Thirunavukkarasu N, Perkins GD, Cecconi M, Cepkova M, Pogson DG, Aya HD, Anjum A, Frazier GJ, Santhakumaran S, Ashby D, Brett SJ (2016) Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: the VANISH randomized clinical trialearly vasopressin vs norepinephrine on kidney failure in septic shock patientsearly vasopressin vs norepinephrine on kidney failure in septic shock patients. JAMA 316:509–518
Roquilly A, Mahe PJ, Seguin P, Guitton C, Floch H, Tellier AC, Merson L, Renard B, Malledant Y, Flet L, Sebille V, Volteau C, Masson D, Nguyen JM, Lejus C, Asehnoune K (2011) Hydrocortisone therapy for patients with multiple trauma: the randomized controlled HYPOLYTE study. JAMA 305:1201–1209
Tongyoo S, Permpikul C, Mongkolpun W, Vattanavanit V, Udompanturak S, Kocak M, Meduri GU (2016) Hydrocortisone treatment in early sepsis-associated acute respiratory distress syndrome: results of a randomized controlled trial. Crit Care 20:329
Plummer MP, Blaser AR, Deane AM (2014) Stress ulceration: prevalence, pathology and association with adverse outcomes. Crit Care 18:213
Narum S, Westergren T, Klemp M (2014) Corticosteroids and risk of gastrointestinal bleeding: a systematic review and meta-analysis. BMJ Open 4:e004587
Beardsley J, Wolbers M, Kibengo FM, Ggayi A-BM, Kamali A, Cuc NTK, Binh TQ, Chau NVV, Farrar J, Merson L, Phuong L, Thwaites G, Van Kinh N, Thuy PT, Chierakul W, Siriboon S, Thiansukhon E, Onsanit S, Supphamongkholchaikul W, Chan AK, Heyderman R, Mwinjiwa E, van Oosterhout JJ, Imran D, Basri H, Mayxay M, Dance D, Phimmasone P, Rattanavong S, Lalloo DG, Day JN, CryptoDex I (2016) Adjunctive dexamethasone in HIV-associated cryptococcal meningitis. N Engl J Med 374:542–554
Tongyoo S, Permpikul C, Mongkolpun W, Vattanavanit V, Udompanturak S, Kocak M, Meduri GU (2016) Hydrocortisone treatment in early sepsis-associated acute respiratory distress syndrome: results of a randomized controlled trial. Crit Care 20:329
Keh D, Trips E, Marx G, Wirtz SP, Abduljawwad E, Bercker S, Bogatsch H, Briegel J, Engel C, Gerlach H, Goldmann A, Kuhn SO, Huter L, Meier-Hellmann A, Nierhaus A, Kluge S, Lehmke J, Loeffler M, Oppert M, Resener K, Schadler D, Schuerholz T, Simon P, Weiler N, Weyland A, Reinhart K, Brunkhorst FM (2016) Effect of hydrocortisone on development of shock among patients with severe sepsis: the HYPRESS randomized clinical trial. JAMA 316:1775–1785
Acknowledgements
We are indebted to the numerous authors who have provided additional information and clarifications regarding their studies including Professors Ananne, Arabi, Ashenoune, Briegel, Christ-Crain, Chotmongkol, Cicarelli, Day, Edwards, Gordon, Hoffman, Keh, Kerr, Martin Jr, Meduri, Mirea, Paydas, Payen, Sawanyawisuth, Scarborough, Sorensen, Sprung, Thwaites, Venkatesh and Weigelt and Dr’s Alía, Blum, Fernandez-Serrano and Plassais. We are also grateful for the assistance with translations of non-English studies from Mr Chris Chui, Dr Peter Biesenbach and Dr Fernando Zampieri. We apologise if in the process of transcribing we have accidently left out authors who have aided this study and we offer our utmost gratitude. .
Funding
No funding was received for any aspect of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
EB, MHM, OC, AG, JP, SLR, AA: none to declare. AP: the ICU at Rigshospitalet, where AP chairs the Research Unit, receives funds for research from Ferring Pharmaceuticals and the Novo Nordisk Foundation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Butler, E., Møller, M.H., Cook, O. et al. The effect of systemic corticosteroids on the incidence of gastrointestinal bleeding in critically ill adults: a systematic review with meta-analysis. Intensive Care Med 45, 1540–1549 (2019). https://doi.org/10.1007/s00134-019-05754-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-019-05754-3