Abstract
Background
Acute kidney injury (AKI) in the intensive care unit is associated with significant mortality and morbidity.
Objectives
To determine and update previous recommendations for the prevention of AKI, specifically the role of fluids, diuretics, inotropes, vasopressors/vasodilators, hormonal and nutritional interventions, sedatives, statins, remote ischaemic preconditioning and care bundles.
Method
A systematic search of the literature was performed for studies published between 1966 and March 2017 using these potential protective strategies in adult patients at risk of AKI. The following clinical conditions were considered: major surgery, critical illness, sepsis, shock, exposure to potentially nephrotoxic drugs and radiocontrast. Clinical endpoints included incidence or grade of AKI, the need for renal replacement therapy and mortality. Studies were graded according to the international GRADE system.
Results
We formulated 12 recommendations, 13 suggestions and seven best practice statements. The few strong recommendations with high-level evidence are mostly against the intervention in question (starches, low-dose dopamine, statins in cardiac surgery). Strong recommendations with lower-level evidence include controlled fluid resuscitation with crystalloids, avoiding fluid overload, titration of norepinephrine to a target MAP of 65–70 mmHg (unless chronic hypertension) and not using diuretics or levosimendan for kidney protection solely.
Conclusion
The results of recent randomised controlled trials have allowed the formulation of new recommendations and/or increase the strength of previous recommendations. On the other hand, in many domains the available evidence remains insufficient, resulting from the limited quality of the clinical trials and the poor reporting of kidney outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) affects up to 50% of critically ill patients and is independently associated with both short- and long-term morbidity and mortality [1,2,3,4,5]. The recent AKI-EPI study demonstrates that the most frequent causes of AKI in the critically ill are sepsis and hypovolaemia followed by nephrotoxic agents [6]. However, the cause of AKI is often multifactorial with pre-existing co-morbidities further increasing the risk [3, 7,8,9].
The aim of this systematic review on the prevention and avoidance of further progression of AKI, by core members of the AKI section of the ESICM, is to provide:
-
A critical evaluation of the existing evidence
-
Give recommendations for clinical practice
-
Update our previously published recommendations [10] and most recent guidelines [2, 11]
Our recommendations principally concern critically ill patients on the ICU but can also be applied to those planned to be admitted to the ICU such as high-risk surgical patients. By consensus, we primarily focussed on the role of volume expansion, diuretics, inotropes, vasopressors/vasodilators, hormones, nutrition, statins, sedatives and ischaemic preconditioning.
Methodology
A systematic search of the literature was performed using the following databases: MEDLINE (1966 through March 2017), EMBASE (1980 through March 2017), CINAHL (1982 through March 2017), Web of Science (1955 through March 2017) and PubMed/PubMed CENTRAL to identify key studies, preferably randomised (placebo) controlled trials (RCT) and meta-analyses, addressing strategies to prevent AKI in adult critically ill patients. The following clinical conditions were considered: major surgery, critical illness, sepsis, shock and exposure to potentially nephrotoxic drugs. Specifically, renal transplantation, primary intrinsic renal disease (e.g. vasculitis) and hepatorenal syndrome were not considered. Search strategy and endpoints are available as electronic supplementary material (ESM_1).
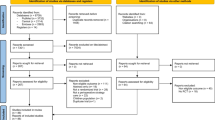
These recommendations are intended to provide clinical guidance and involved a modified Delphi process with a consensus meeting during the annual congresses of the European Society of Intensive Care Medicine in 2014, 2015 and 2016 followed by electronic-based/telephone discussions. The quality of the evidence was judged by using the most recent GRADE (Gradings of Recommendations, Assessment, Development and Evaluation) criteria (Fig. 1) [12, 13]. The strength of the recommendations was classified as either strong (Grade 1) or weak (Grade 2). The degree (i.e. quality) of evidence for the recommendations was classified from high (A) to very low (D) according to factors including study design consistency of the results and directness of the evidence (Fig. 1, ESM_1 Table S1). Evidence was downgraded where there was a risk of bias, inconsistency and imprecision. Evidence was upgraded for large effect size or significant dose–response gradient. If benefit or harm was unequivocal, but evidence was difficult to categorize by the GRADE methodology, we used best practice statements (BPSs), which represent ungraded strong recommendations [14] (Table 1).

(Modified from Guyatt et al. [12])
Grade system for grading recommendations
We acknowledge that there may be circumstances whereby a recommendation cannot or should not be followed for an individual patient. Furthermore, interventions are generally investigated in isolation and not in combination, and as such recommendations relate to the primary intervention. Local clinical guidelines will govern the use of either a single intervention or a combination thereof.
Volume expansion
Recommendations
-
1.
We recommend controlled fluid resuscitation in volume depletion, while, however, avoiding volume overload (Grade 1C).
-
2.
We recommend against the use of starches (Grade 1A) as harm has been shown and suggest not using gelatine or dextrans for fluid resuscitation (Grade 2C).
-
3.
We recommend correction of hypovolaemia/dehydration using isotonic crystalloids in patients receiving intravascular contrast media (Grade 1B).
-
4.
We recommend regular monitoring of chloride levels and acid–base status in situations where chloride-rich solutions are used (BPS).
-
5.
We suggest the use of balanced crystalloids for large volume resuscitation (Grade 2C).
-
6.
We suggest using human serum albumin if a colloid is deemed necessary for the treatment of patients with septic shock (Grade 2C).
-
7.
We suggest prophylactic volume expansion with crystalloids to prevent AKI by certain drugs (specified below) (BPS).
-
8.
We suggest not delaying urgent contrast-enhanced investigations or interventions for potential preventative measures (BPS).
Rationale
Relative and overt hypovolaemia are significant risk factors for development of AKI [15,16,17,18]. Timely fluid administration can restore circulating volume and renal perfusion, and may also reduce nephrotoxicity [19]. Volume replacement should be performed in a controlled, monitored fashion [20] as injudicious use of fluids carries its own inherent risks and may even contribute to AKI by increasing renal interstitial oedema and renal parenchymal pressure [21, 22]. Moreover, goal-directed therapy including the use of central venous pressure (CVP) as a resuscitation target has not been shown to prevent AKI in sepsis [23]. Volume replacement may be through crystalloids, colloids or their combination. Isotonic crystalloids represent the mainstay for correcting extracellular volume depletion with the caveat that hyperchloraemia is prevented to reduce potential renal vasoconstriction [24, 25]. Compared to crystalloids, colloids theoretically result in a greater plasma expansion. However, this effect depends on vascular barrier integrity which may be compromised in sepsis, particularly in the presence of vasoplegia [26, 27]. Consequently, the difference in required volumes for fluid resuscitation was minimal between crystalloids and colloids in large RCTs [28]. Moreover, large volume replacement with colloids alone risks hyperoncotic impairment of glomerular filtration [29, 30] and osmotic tubular damage [31, 32].
Available artificial colloids include gelatines, dextrans and until recently, starches. Gelatines have a moderate volume effect. Although risk of osmotic nephrosis with gelatines exists [33], the lack of clear clinical data on deleterious effects on renal function [34, 35] is offset by the possible prion transmission, histamine release and coagulopathy [36, 37]. Dextrans have reasonably high volume effects although anaphylaxis, coagulation disorders, osmotic nephrosis and AKI may occur with doses above 1.5 g/kg/day [38,39,40,41]. Human albumin (HA) is the only naturally occurring colloid and may appear attractive in hypooncotic hypovolaemia. It does increase the response to diuretics in patients with hypoalbuminaemia (e.g. nephrotic syndrome) [42, 43], has no negative effects on kidney function [44, 45], is safe [46] but can be costly.
Clinical studies
Unsurprisingly, no studies have specifically addressed the effects of volume expansion compared to no volume resuscitation in overt hypovolaemia given the intuitive benefits of volume replacement. In severe sepsis, the beneficial effects of timely volume replacement on organ failure and mortality are well known, although the first RCT proving benefit of early volume resuscitation did not report kidney function [47]. On the other hand, preoperative volume expansion failed to reduce the incidence of postoperative AKI ins 328 patients undergoing cardiac surgery [48], and a recent pilot RCT in sepsis could demonstrate that a volume-restrictive fluid protocol can reduced the incidence of AKI (RR 0.32; 95% CI 0.32–0.96) [49].
Crystalloids are considered the mainstay for volume expansion. Observational studies suggest an increased risk of AKI, renal replacement therapy (RRT) and mortality associated with the use of large volumes of normal saline (0.9% NaCl) as compared to so-called balanced solutions where chloride is partially replaced by another metabolizable anion [50–52]. An RCT comparing saline to a balanced solution (Plasmalyte®) in 2278 patients treated in four ICUs failed to show any superiority of balanced crystalloids regarding renal outcomes [53]. The study has been criticized for the limited fluid doses, inclusion of patients with low disease severity and the absence of data on chloride levels [54]. Similar results were observed in the pilot cluster-randomised, multiple-crossover SALT trial comparing saline to a balanced solution in 974 critically ill adults [55]. Again, only modest volumes were used, but increased rates of AKI were found in the normal saline group if larger volumes were administered (ESM_2 Table S2). Studies on the effectiveness of sodium bicarbonate in preventing AKI, predominantly in patients undergoing cardiac surgery, have produced conflicting results [56–59] as have consecutive meta-analyses [60–63].
The effect of colloids on renal function has undergone extensive scrutiny over the last decade. Large RCTs have substantiated the increased risk of AKI and RRT with use of starches [64] particularly in sepsis [65, 66], where they also lead to increased mortality [66] (ESM_2 Table S3). This is verified by several meta-analyses [67–70] which underpin the abandoning of starches in critically ill patients [20, 71, 72]. Clinical data on the effects of gelatine on renal function are scarce. A recent meta-analysis, including three trials in 212 patients comparing gelatins with crystalloids or albumin, indicated a 35% increased relative risk of developing AKI with gelatine [73].
In contrast to artificial colloids, the administration of albumin appears to be safe for the kidney. A large RCT comparing normal saline to 4% HA in various clinical settings failed to demonstrate any differences in renal function [46] (ESM_2 Table S3). In the ALBIOS trial the use of hyperoncotic (20%) albumin showed no effect on AKI or need for RRT in severe sepsis [74] but enabled a less positive fluid balance, confirming the results of another small trial [75]. A post hoc analysis of the ALBIOS trial showed survival benefit in septic shock [74] confirmed by meta-analyses [76, 77]. Hypoalbuminaemia in cardiac surgery might be another indication with improved fluid balance as well as a reduced rate of AKI being observed in a single-centre RCT of 220 patients [78].
Hypovolaemia may also contribute significantly towards drug-induced renal injury, although the available evidence supporting preventative hydration is only observational with no consensus related to timing, optimal volume and type of solution [19, 237, 79]. Prophylactic volume expansion has been shown to prevent harm from amphotericin B, antivirals including foscarnet, cidofovir and adefovir [81–83] as well as drugs causing crystal nephropathy such as indinavir, acyclovir, and sulfadiazine [84].
Prophylactic volume expansion is the mainstay of all recommendations to prevent contrast-associated AKI (CA-AKI) and is based on several randomised controlled studies performed in non-critically ill patients [85–90]. However, studies comparing hydration to no hydration are scarce [91]. Several pitfalls should be considered. First, CA-AKI is a diagnosis of exclusion and considerable variation exists with regard to the reported incidence rates, which are confounded by many factors such as transient fluctuations in measured serum creatinine in hospitalised patients and use of non-standardised diagnostic criteria [92]. Secondly, CA-AKI does not occur in patients without other risk factors for AKI, whereas most critically ill patients receiving intravascular contrast have other risk factors. Moreover, individuals with high risk for CA-AKI may not be given contrast. For these reasons the role of CA-AKI is uncertain, particularly in an era where the use of low- or iso-osmotic agents and lower contrast volume administration have become standard practice. As indicated by an analysis of the Nationwide Inpatient Sample dataset comprising 5, 931,523 hospitalisations the OR for CA-AKI adjusted for age, sex, mechanical ventilation and combined co-morbidity score was 0.93 (0.88–0.97) [93]. Whereas a retrospective single-centre cohort study in 747 critically ill patients showed a rate of CA-AKI of 16% [94], matched cohort studies could not demonstrate a relationship with IV contrast for computed tomography in the ICU [95–97] or emergency department [98]. These findings are supported by a systematic review and Bayesian meta-analysis [99]. In the most recent propensity-matched cohort study, IV contrast was not associated with an increased risk of AKI or dialysis, but a subgroup with pre-CT eGFR of at most 45 ml/min/1.73 m2 showed an increased risk of dialysis. The numbers in this subgroup were, however, small and subject to selection bias [97].
Although it seems prudent to correct hypovolaemia before contrast administration, prophylactic volume expansion in critically ll patients who are euvolaemic cannot be recommended on the basis of current data. No study demonstrates protection of pre-emptive volume expansion against CA-AKI in the critically ill. An RCT comparing hydration with isotonic bicarbonate versus normal saline failed to show superiority of either regimen but reported an excessively high rate of CA-AKI of 33% in both groups [100], which may be attributed to severity of illness in this critically ill cohort. Importantly, in patients with chronic kidney disease (CKD) undergoing percutaneous coronary intervention (PCI), hydration volumes above 11 ml/kg body weight (BW) were associated with continuously increased rates of AKI, requirement for RRT and mortality. The adjusted OR for developing AKI with hydration volumes greater than 25 ml/kg BW was 2.11 (CI 1.24–3.59) [101]. We recommend that the clinical decision to perform a contrast study in ICU patients must weigh the potential benefits with the low but probably not zero risk of CA-AKI.
Diuretics
Recommendations
-
1.
We recommend against loop diuretics given solely for the prevention of acute kidney injury (Grade 1B).
-
2.
We suggest using diuretics to control or avoid fluid overload in patients that are diuretic-responsive (Grade 2D).
Rationale
Oligoanuria is frequently the first indicator of acute renal dysfunction. Intensivists frequently use loop diuretics in a wide spectrum of AKI settings [102]. The rationale for using diuretics to ameliorate AKI includes prevention of tubular obstruction, reduction in medullary oxygen consumption and increase in renal blood flow as well as reducing fluid overload and venous congestion [103–105]. Although there is no single parameter for fluid overload, increased CVP [106], peripheral oedema [107] and/or increased intra-abdominal pressure [108, 109] may be used as surrogates. A recent study demonstrated than a urinary output of at least 100 ml/h following a test dose of 1.0–1.5 mg furosemide/kg BW predicted reduced progression to a higher stage of AKI in oliguric patients [110].
Clinical studies
Use of conservative fluid management including diuretics has been investigated in only one large RCT in patients with acute lung injury (FACTT trial) which showed a tendency to reduced requirement of RRT [111].
In cardiac surgery either no protection [112] or elevated postoperative serum creatinine levels were found in patients receiving furosemide [113]. These findings were supported by a recent meta-analysis [114]. In patients with acute heart failure, diuretic therapy with higher doses was more effective at reducing clinical symptoms, but at the cost of decreased renal function [115]. To date four RCTs have examined the role of diuretics in established renal failure in the intensive care setting. No demonstrable improvements in clinically relevant outcomes, such as recovery of renal function or mortality, were observed [31, 116–118]. Other studies compared diuretics with dopamine or placebo, again with no perceived benefit [119–121]. Three meta-analyses confirmed that the use of diuretics in established AKI did not alter outcome but carried a significant risk of side effects such as hearing loss [122–124] (ESM_2 Table S4).
Vasopressors
Recommendations
-
1.
We recommend titrating vasopressors to a mean arterial pressure (MAP) of 65–70 mmHg (Grade 1B) rather than a higher MAP target (80–85 mmHg) in patients with septic shock. However, for patients with chronic hypertension we recommend aiming for a higher target (80–85 mmHg) for renal protection in septic shock (Grade 1C).
-
2.
We recommend lowering systolic pressure to 140–190 mmHg rather than to 110–139 mmHg in patients with acute cerebral haemorrhage with severe admission hypertension (Grade 1C).
-
3.
If vasopressors are needed for treatment of hypotension, we recommend norepinephrine (along with correction of hypovolaemia) as the first-choice vasopressor to protect kidney function (Grade 1B) and suggest vasopressin in patients with vasoplegic shock after cardiac surgery (Grade 2C).
-
4.
We suggest individualizing target pressure when premorbid blood pressure is available (BPS).
Rationale for MAP target
Preservation or improvement of renal perfusion can theoretically be achieved through increasing cardiac output by fluid resuscitation or inotropic drugs, through renal vasodilators or systemic vasopressors. Optimal target mean arterial pressure (MAP) was studied in a large open-label multicentre RCT randomising 777 patients with septic shock to resuscitation with a MAP target of either 80–85 mmHg or 65–70 mmHg [125]. In most of the patients the achieved MAP was above the set target. The study found no difference in mortality, incidence of AKI stage 2 (38.7% vs. 41.5%, p = 0.42) or need for RRT (33.5% vs. 35.8%, p = 0.5), but more atrial fibrillation in the high target group. However, in patients with known chronic hypertension a higher MAP resulted in a lower incidence of AKI stage 2 (38.9% vs. 52%, p = 0.02) and less RRT (31.7% vs 42.2%, p = 0.046); mortality was unchanged.
The safety of lowering systolic pressure was studied in a larger RCT in patients with acute cerebral haemorrhage with severe hypertension on admission [126]. Patients were randomised to a systolic blood pressure target of 110–139 or 140–179 mmHg. The primary endpoint (death or disability) was not different between groups. However, the rate of serious renal adverse events was higher in the lower target group (9% vs. 4%, p = 0.002) (ESM_2 Table S5).
Rationale for choice of vasopressor
Norepinephrine is the most commonly used vasopressor in patients with vasodilatory shock. A large RCT comparing dopamine to norepinephrine as initial vasopressor in patients with shock found no difference in mortality between randomised groups. However, norepinephrine was associated with less tachycardia in the first hours and was superior regarding survival in cardiogenic shock patients. In addition, there was a trend towards more RRT-free days through day 28 in the norepinephrine group [127].
Vasopressin or the analogue terlipressin may have a role in the treatment of norepinephrine-refractory shock [128]. Exogenous vasopressin has vasoconstrictive and antidiuretic properties and may increase glomerular filtration by preferential post-glomerular vasoconstriction [129]. In the largest RCT in septic shock (VASST trial), vasopressin reduced mortality in the subgroup with less severe shock, but not in the entire population. There were no differences in RRT-free days [130]. However, in a secondary analysis, a reduced progression to higher stages of AKI could be demonstrated in the subgroup of patients with AKI stage 1 at baseline [131]. In a subsequent 2 × 2 RCT in 409 patients with early septic shock (VANISH trial) [132], the use of vasopressin compared to norepinephrine did not affect the proportion of patients who never developed AKI stage 3 (57% vs. 59.2%), the number of AKI stage 3-free days [difference −4 (−11 to 5)] or the incidence of AKI stage 3 [difference −5.1% (−15.2 to 5.0)]. The use of vasopressin reduced the need for RRT (difference −9.9% (−19.3 to −0.6), but only in non-survivors. A recent single-centre RCT in 300 patients with vasoplegic shock after cardiac surgery compared noradrenalin to vasopressin as first-choice vasopressor. The use of vasopressin was associated with less acute renal failure (10.3% vs. 35.8%, p < 0.0001) and less RRT (2.7% vs. 13.9%, p = 0.0016) [133]. This trial, however, had some design issues (e.g. change in primary outcome during the study) and requires confirmation. The studies are summarized in ESM_2 Table S5.
Use of vasodilators
Recommendations
-
1.
We recommend against low-dose dopamine for protection against AKI (Grade 1A).
-
2.
We recommend not using levosimendan for renal protection in patients with sepsis (Grade 1B) and recommend against its use for renal protection in cardiac surgery patients with poor preoperative left ventricular function or needing postoperative haemodynamic support (Grade 1B).
-
3.
We suggest not using fenoldopam or natriuretic peptides for renal protection in critically ill or cardiovascular surgery patients at risk of AKI (Grade 2B).
Rationale
Early in the course of ischaemic AKI, renal blood flow (RBF) falls because of stimulation of the sympathetic nervous system and the release of vasoconstrictors such as endothelin, angiotensin II and vasoconstrictive prostaglandins [134, 135]. In contrast, during septic AKI global RBF seems to be well preserved [136, 137]. The main perfusion problem during sepsis seems to occur at the microvascular level and regionally in the outer medulla [138]. When using vasodilators for kidney protection, several issues should be considered. First, vasodilators may cause hypotension by counteracting compensatory vasoconstriction, thus unmasking occult hypovolaemia. Hypotension may further compromise renal perfusion and correction of hypovolaemia is therefore crucial. Second, as a result of endothelial damage, nitric oxide (NO)-dependent vasodilators seem to be ineffective [135]. Third, timing may be crucial, since delayed administration reduces effectiveness as a result of occlusion of the microcirculation [139].
Clinical studies
Low-dose or ‘renal’ dose dopamine has been advocated in the past to prevent selective renal vasoconstriction in a variety of conditions. This may not be the case in complex clinical conditions, where low-dose dopamine may even worsen renal perfusion [140]. Several meta-analyses have concluded that ‘renal-dose’ dopamine has no benefit in either preventing or ameliorating AKI in the critically ill [141–143], the latest [141] being presented in ESM_2 Table S6.
Fenoldopam is a pure dopamine-A1 receptor agonist providing systemic and renal vasodilation and natriuresis, and it has been studied in cardiovascular surgery and critically ill patients. Two older meta-analyses, one including 1290 critically ill and surgical patients (mainly cardiovascular) from 16 RCTs and the other including 1059 cardiac surgery patients from 13 (partially overlapping) RCTs and case-matched studies, reported that the use of fenoldopam reduced the incidence of AKI, need for RRT and hospital mortality [144]. Most studies were small with a moderate to high risk of bias and in the second meta-analysis 30% of the included studies were abstracts. The two most recent meta-analyses in cardiac surgery and major surgery used stricter inclusion criteria [145, 146] and only found a lower risk for AKI, but not for RRT or death. In addition, both showed an increased risk of hypotension and most included studies had a high risk of bias due to low sample size and fragility index, and use of different definitions for AKI. The most recent and largest RCT in post cardiac surgery patients with AKIN stage I [147] did not show any renal protection or clinical benefit from the use of fenoldopam, while fenoldopam conferred more hypotension. (Studies are summarized in ESM_2 Table S7).
Atrial natriuretic peptide (ANP) is produced by cardiac atria in response to an acute increase in stretch and/or pressure and induces afferent dilatation and efferent vasoconstriction, thereby increasing glomerular filtration and urinary sodium excretion with a dose-dependent hypotensive effect [148, 149]. B-type (brain) natriuretic peptide (BNP) is primarily produced in the cardiac ventricles and has similar effects [150, 151].
The two most recent meta-analyses including RCTs in the cardiac and cardiovascular surgery population found that the prophylactic infusion of low-dose ANP reduced postoperative peak creatinine [152] and the need for RRT [152–154]. However, the latter was based on only 24 cases of RRT in 563 patients. No effect was found in established AKI and high-dose ANP was associated with more frequent adverse effects (arrhythmias, hypotension) [154]. Two later RCTs on the use of ANP in aortic arch (n = 42) and high-risk cardiac surgery (n = 367) confirmed a reduction in postoperative AKI and need for RRT (0/183 vs. 7/184, p = 0.015) [155, 156] (ESM_2 Table S8).
A recent meta-analysis including 15 RCTs in 9623 patients with acute decompensated heart failure showed that the use of BNP (nesiritide) was associated with worsening renal function: RR 1.08 (1.01–1.15), especially in the subgroup receiving a high dose (>0.01 μg/kg/min) and in patients without CKD [157].
In general, most BNP trials were small, not powered for the endpoints RRT or mortality, of poor quality with low fragility index; inclusion criteria varied and results were heterogeneous. Furthermore, hypotension and arrhythmia were frequently reported. A small subgroup meta-analysis on BNP in cardiovascular surgery also showed no benefit [152] (ESM_2 Table S8).
The calcium sensitizer levosimendan has inodilator, cardioprotective and anti-inflammatory effects [158, 159]. In a recent meta-analysis of RCTs in the cardiac surgery population (13 trials, 1345 patients), the use of levosimendan decreased the risk of AKI [OR 0.51 (0.24–0.79)], the need for RRT [OR 0.43 (0.25–0.76)] and mortality [OR 0.41 (0.27–0.62)] [160]. The last meta-analysis of RCTs in the critically ill population with or at risk of AKI (33 RCTs, 3867 patients) found that, compared to placebo or another inotrope, levosimendan decreased the risk of AKI [RR 0.79 (0.63–0.99)] and the need for RRT [RR 0.52 (0.32–0.86)]. When limiting the analysis to high-quality studies, the difference in need for RRT between groups failed to reach significance [RR 0.41 (0.15–1.12)] [161]. Studies in both meta-analyses were small, there was some heterogeneity, AKI was not always a predefined endpoint, different definitions of AKI were used and there might have been some outcome reporting bias.
Three large placebo-controlled RCTs have recently been published. In patients with sepsis the use of levosimendan was not beneficial in terms of a reduction of renal SOFA, need for RRT [OR 0.99 (0.66–1.49)] or mortality [OR 1.19 (0.82–1.72)], while its use was associated with more adverse events [162]. In 882 patients with left ventricular dysfunction undergoing cardiac surgery, levosimendan had no effect on mortality or need for RRT [163]. No effect on AKI and RRT was seen when levosimendan was given for haemodynamic support after cardiac surgery in 506 patients [164] (ESM_2 Table S9).
Sedation
Recommendations
-
1.
On the basis of current data no recommendation can be given, although it appears that shorter sedation using propofol or dexmedetomidine may have several advantages, possibly reducing the rate of AKI (BPS).
Rationale
Sedation is necessary in many critically ill patients and this may affect cardiac function and/or vascular tone with renal consequences. In animal models propofol reduced markers of oxidative stress in the kidney [165, 166] and dexmedetomidine caused diuresis through reducing vasopressin secretion, enhancing renal blood flow and hence glomerular filtration [167] and showed renal protection [168–171].
Clinical studies
Propofol is commonly used as anaesthetic and for sedation in the intensive care unit [172]. The “propofol infusion syndrome” comprises myopathy, rhabdomyolysis, hyperkalaemia and AKI [173, 174]. On the basis of the data from case reports/series, it is recommended to administer propofol for a maximum of 48 h and a maximum dose of 4 mg/kg/h [175]. On the other hand, a recent propensity-matched cohort study in critically ill patients showed reduced risk of AKI and need for RRT in patients sedated with propofol as compared to midazolam [176]. Furthermore a small RCT including 112 patients undergoing valvular heart surgery showed less AKI and significantly lower cystatin C levels in the group treated with propofol as compared to sevoflurane [177]. However, the fact that remote ischaemic preconditioning showed less effect if patients were treated with propofol leaves uncertainty about the protective effect of propofol on the kidney [178].
α-2 Adrenergic agonists have multiple pharmacodynamic effects [179]. In a placebo-controlled double-blind RCT dexmedetomidine demonstrated significant diuretic effects, with an almost 75% increase in diuresis after cardiac surgery, but did not affect renal function per se [180]. Observational trials indicated protection of kidney function after cardiac surgery [181] but not when used for sedation during lung cancer resection [182]. A placebo-controlled study in 90 patients undergoing coronary artery bypass graft (CABG) showed a dose-dependent reduction of NGAL levels with dexmedetomidine used for postoperative sedation [183]. Another RCT in 200 patients showed that dexmedetomidine for 24 h at 0.4 μg/kg/h from start of anaesthesia resulted in reduced rate of AKI, morbidity and length of stay in the ICU [184] (ESM_2 Table S10).
Alltogether, the data for non-benzodiazepine sedatives, especially dexmedetomidine, are promising but currently not sufficiently convincing to give a clear recommendation.
Hormonal manipulation
Recommendations
-
1.
We suggest targeting a blood glucose level at least below 180 mg/dL (10 mmol/l) for the prevention of hyperglycaemic kidney damage in the general ICU population (Grade 2B).
-
2.
We suggest not using erythropoietin (Grade 2B) or steroids (Grade 2B) for prevention of acute kidney injury.
Rationale
In critical illness hyperglycaemia has been associated with adverse outcomes [185, 186] attributed to oxidative stress, endothelial dysfunction, alterations in haemostasis, immune dysregulation and mitochondrial dysfunction. The anti-inflammatory effect of steroids may attenuate the inflammatory component of AKI pathogenesis. Erythropoietin (EPO), besides being a haematopoietic growth factor, also has tissue-protective properties by decreasing apoptosis and inflammation and by promoting neovascularization and tissue regeneration.
Clinical studies
A large prospective RCT in 1548 surgical ICU patients compared tight glucose control (TGC) with insulin (target blood glucose 80–110 mg/dL) to standard care (insulin when blood glucose is greater than 200 mg/dL resulting in a mean blood glucose of 150–160 mg/dL) and showed not only an improved survival rate but also a 41% reduction in AKI requiring RRT [187]. Additionally, TGC also reduced the number of patients with peak plasma creatinine greater than 2.5 mg/dL by 27%. A subsequent study in the medical ICU of the same hospital, including many patients that already had AKI on admission, did not confirm the effect on survival or need for RRT, but showed a 34% reduction in AKI, defined as a doubling of serum creatinine compared with the admission level [188]. A combined analysis of both studies showed a more pronounced renal protection when normoglycaemia was achieved [189].
More recent RCTs in septic [65] and general [190–194] ICU patients (some of which had to be stopped early because of hypoglycaemia) including a large adequately powered multicentre trial in Australia and New Zealand (NICE-SUGAR) [191] did not confirm the renoprotective effect. The latter even found a higher mortality in patients treated with TGC compared to an intermediate level. Clinicians should, however, be aware of important differences between these landmark trials, such as the glycaemic target in the control group, the nutritional strategy and the methods used to measure blood glucose levels [195]. The most recent meta-analysis on this issue did not find a mortality benefit [RR 1.06 (0.99–1.13)] [196] of TGC nor a renoprotective effect (evaluated by the need for RRT only) [RR 0.96 (0.83–1.11)] [196] (ESM_2 Table 11).
A major obstacle to the broad implementation of TGC is the increased risk of hypoglycaemia. Patients with AKI are at particular risk [197]. On the other hand, a causal relationship between a short-lasting iatrogenic hypoglycaemia in the monitored setting of an ICU and outcome remains controversial [198–200]. If clinicians decide to adopt TGC strategies, fluctuations in glucose levels should be minimized and reliable tools should be employed to measure blood glucose [195]. Because of the risk of hypoglycemia, current guidelines suggest more moderate blood glucose targets (less than 180 mg/dL [20], less than 150 mg/dl [52], 140–180 mg/dL [201]) in critically ill patients, although these targets have not been formally compared with tolerating hyperglycaemia [202] (ESM_2 Table S11).
A recent large RCT (n = 4494) demonstrated no significant effect of the intraoperative administration of dexamethasone on a composite endpoint of major complications after cardiac surgery. The RR for RIFLE-Failure was 0.7 (0.44–1.14) [203]. A post hoc analysis of this trial showed a beneficial effect on the need for RRT (RR 0.44 (0.19–0.96)), an effect that was mainly seen in patients with eGFR less than 15 ml/min/1.73 m2 and remains to be confirmed [204]. Another placebo-controlled RCT in 7507 patients found no effect of methylprednisolone on the incidence of AKI stage 3 after cardiac surgery [205].
Prospective randomised placebo-controlled trials on the renoprotective effect of erythropoietin have mainly been performed in the setting of cardiac surgery [206–210]. A recent meta-analysis (5 studies, 423 patients) found no effect of erythropoietin on the incidence of AKI: RR 0.64 (0.35–1.16). Surprisingly, a preplanned subgroup analysis found a significant reduction of AKI in patients without high risk for AKI: RR 0.37 (0.24–0.61; p < 0.0001) [211]. Similar results were obtained in the most recent meta-analysis, which in addition showed more protection with pre-anaesthetic administration [212]. Another RCT in cardiac surgery including 75 patients with pre-existing renal impairment found no differences in postoperative levels of serum creatinine, cystatin C or NGAL [213]. A second meta-analysis (on a total of 2759 patients) that also included studies in ICU patients [214, 215] likewise did not establish a renoprotective effect of erythropoietin: incidence of AKI RR 0.72 (0.79–1.19); dialysis requirement RR 0.72 (0.31–1.70), mortality RR 0.96 (0.78–1.18), all without significant heterogeneity amongst studies [216]. It should, however, be emphasized that in the largest study in ICU patients [215] AKI was only reported as an adverse effect and not clearly defined. Two more recent RCTs in the setting of thoracic aortic surgery [217] and contrast administration in diabetics [218] confirmed the absence of beneficial effect of EPO on the incidence of AKI or need for RRT in critically ill patients (ESM_2 Table S12).
Metabolic interventions
Recommendations
-
1.
We recommend not using high-dose IV selenium for renal protection in critically ill patients (1B).
-
2.
We suggest not using N-acetylcysteine to prevent contrast-associated AKI in critically ill patients because of conflicting results and possible adverse effects (Grade 2B).
-
3.
We suggest that all patients with or at risk of acute kidney injury have adequate nutritional support preferably through the enteral route (BPS).
Rationale
Starvation accelerates protein breakdown and impairs protein synthesis in the kidney, whereas feeding might exert the opposite effects and promote renal regeneration. In animal experiments increased protein intake has been shown to reduce tubular injury [219, 220], and enteral versus parenteral nutrition improved the resolution of AKI [221]. On the other hand, amino acids infused before or during ischaemia may also enhance tubular damage and accelerate loss of renal function [222]. This may also extend to high-dose glutamine when given to patients during the injury phase of AKI [223]. Furthermore, brief periods of reduced food intake appear to increase resistance against ischaemia–reperfusion injury in rodents [224]. This “amino acid paradox” may be related to the increase in metabolic work for transport processes which may aggravate ischaemic injury. Enhanced autophagy, induced by nutrient deprivation and promoting the repair of cellular damage, may be an alternative explanation. In this context permissive underfeeding during the acute phase of critical illness may be protective against AKI.
One aspect of nutrition is the adequate supply of nutritional co-factors and antioxidants such as the glutathione precursor N-acetylcysteine (NAC), antioxidant vitamins (vitamin E (α-tocopherol) and vitamin C (ascorbic acid)) as well as selenium. However, these antioxidants have also been investigated in pharmacological doses with the intention to provide protection against damage by oxygen radicals.
Clinical studies
Protein(s) and amino acids augment renal perfusion and improve renal function, representing recruitment of “renal reserve capacity” [225]. An RCT investigating the effects of daily intravenous amino acid supplementation up to 100 g/day in 424 critically ill patients could not find a significant effect on the duration of AKI despite an increase in eGFR in the treatment group [226]. Furthermore, there was a trend towards increased need for RRT which corresponds to findings from the EPaNIC trial where early parenteral nutrition increased the duration of RRT probably driven by higher urea levels [227]. Correspondingly, lower caloric intake (defined as receiving less than 60% of requirements, also called permissive underfeeding) has been found to be associated with a lower risk for RRT (RR 0.711, 95% CI 0.545–0.928) [228].
A host of RCTs have been performed comparing NAC to placebo or other interventions with or without hydration in non-critically ill patients receiving radiocontrast media [229–80]. Results are controversial as alluded to earlier but the latest meta-analysis assessing the efficacy of intravenous NAC only showed no reduction of AKI or RRT [238]. The ACT trial, currently the largest RCT including 2308 patients undergoing coronary and peripheral vascular angiography, failed to demonstrate any beneficial effect of NAC [239]. RCTs in the critically ill population are not available.
RCTs examining the role of NAC in the prevention of renal dysfunction in high-risk contexts like cardiac surgery showed controversial results [240–246] (ESM_2 Table S13). In addition IV NAC may be harmful leading to allergic reactions [247] and decreased cardiac output or survival in patients with septic shock [248, 249].
A small RCT in 42 patients showed that selenium supplementation decreased the requirement for RRT from 43% to 14% in patients with SIRS [250]. These finding could, however, not be reproduced in consecutive trials [251] including two larger RCTs involving 249 and 1089 patients with sepsis [252, 253].
Statins
Recommendations
-
1.
We recommend against the perioperative use of high-dose statins to prevent postoperative AKI in cardiac surgery (Grade 1A).
-
2.
We suggest the short-term use of atorvastatin or rosuvastatin to prevent contrast-associated AKI in high-risk patients undergoing coronary contrast angiography (Grade 2B).
Rationale
The pleiotropic effect of statins, including antioxidant, anti-inflammatory and antithrombotic effects, may contribute to nephroprotection [254].
Clinical studies
Statins may have a beneficial role in high-risk patients exposed to contrast administration for angiography, as suggested by three recent RCTs [255–257]. In a multicentre trial in China, 2998 patients with type 2 diabetes or mild to moderate CKD undergoing coronary or peripheral arterial angiography were randomised to a 5-day course of rosuvastatin versus no statin [255]. The incidence of CA-AKI was significantly lower in those receiving rosuvastatin (2.3% vs. 3.9%, respectively, p = 0.01). In a single-centre study [256], 504 statin-naïve patients with acute coronary syndrome (ACS) scheduled to undergo an early invasive strategy were randomised to high-dose rosuvastatin at the time of admission versus treatment with atorvastatin commenced at hospital discharge; 6.7% of patients in the early high-dose statin group developed CA-AKI compared to 15.1% in the control group. The 30-day rate of adverse cardiovascular and renal events was also significantly reduced in the rosuvastatin group (3.6% vs. 7.9%, respectively, p = 0.036). An RCT in 410 CKD patients showed less CA-AKI in patients randomised to a single dose of atorvastatin within 24 h before contrast exposure compared to the control group (4.5% vs. 17.8%, p = 0.005) [257]. Two more recent RCTs found similar effects of statins in diabetics with CKD [258, 259]. These positive findings were confirmed by several meta-analyses combining studies in patients undergoing coronary angiography [260–263] (ESM_2 Table S14). One of these meta-analyses concluded that short-term, pre-procedural, intensive statin treatment only reduced CA-AKI in ACS patients and recommended further studies in non-ACS patients [264]. This meta-analysis, however, did not include the largest RCT [255]. Although, these results lend support to the short-term use of statins before procedures involving intra-arterial contrast exposure in patients with coronary artery disease with or without diabetes and/or CKD, it must be considered that most of the studies were performed outside the ICU, thereby warranting downgrading of the level of evidence.
In patients undergoing cardiac surgery, two large meta-analyses including data from observational studies found conflicting evidence regarding the role of preoperatve statin in preventing postoperative AKI [265, 266], and a Cochrane analysis of small RCTs found no effect [267]. Two recent placebo-controlled RCTs investigated the effects of perioperative high-dose atorvastatin (i.e. 80 mg, followed by 40 mg daily) in elective cardiac surgery [268] and valvular heart surgery [269] and showed no renal benefit. Furthermore, in the largest trial, statin-naïve patients with CKD had a higher incidence of AKI when treated with statin [268] (ESM_2 Table S15). Finally, an even larger placebo-controlled RCT in 1922 cardiac surgery patients that included AKI as a secondary outcome demonstrated renal harm in those receiving rosuvastatin 20 mg/day in the perioperative period [270].
Remote ischaemic preconditioning
Recommendations
-
1.
We suggest not using remote ischaemic preconditioning for prevention of AKI in critically ill patients (Grade 2A).
Rationale
Remote ischaemic preconditioning (RIPC) or several short cycles of limb ischaemia is achieved through inflation of a blood pressure cuff. The mechanism by which RIPC prevents AKI is incompletely understood.
Clinical studies
In cardiac surgery several single-centre RCTs demonstrated reduced incidence of AKI and need for RRT [271–273]. However, several others, including four larger and multicentric RCTs [274–277] did not confirm these beneficial effects, nor was a change in creatinine or mortality demonstrated. The conflicting results in cardiac surgery may be explained by inclusion of low-risk patients in trials that showed no benefit, and the use of propofol and opioids, treatments that may blunt the beneficial effects of RIPC.
In 13 recent meta-analyses the effect of RIPC was evaluated in different cohorts and definitions of AKI [178, 278–289]. Though several meta-analyses found a reduction of AKI [278, 279, 281–284, 286, 287, 289, 290] this was restricted to stage 1 AKI [289], or subgroups such as percutaneous coronary interventions [278, 279], or cardiac surgery with propofol-free anaesthesia [283]. The meta-analyses are limited by risk of bias, heterogeneity in definitions of AKI, low event rates and underestimation of influence of co-morbidities [283, 289]. Finally, a Cochrane review including studies on patients undergoing surgery could not show a benefit on renal outcomes [178] (ESM_2 Table S16).
In summary, the effects by which RIPC prevents AKI are incompletely understood. RIPC for prevention of AKI has mainly been evaluated in cardiovascular surgery and after contrast administration. Larger studies and meta-analyses are not consistent in demonstrating a preventive effect of RIPC for AKI.
AKI care bundles
Recommendations
-
1.
We suggest using the KDIGO recommendations to reduce the incidence of AKI after cardiac surgery (Grade 2C).
-
2.
The use of AKI care bundles outside the intensive care unit has some benefits, including the potential to improve the outcome of AKI (BPS).
Rationale
Care bundles have been proposed as tools to improve the quality of care and outcome of patients with AKI. Ideally, they should contain a small set of practices, processes or treatments that are evidence-based, endorsed and/or recommended by guidelines and broadly accepted as appropriate and/or standard care by local stakeholders. They are designed such that if one element is not implemented, the remaining elements are not impacted.
Clinical studies
Outside the critical care setting, different AKI care bundles have been implemented with variable improvement in clinical care, more efficient resource use and potentially improved outcomes, especially if combined with educational measures and electronic alerting [291–293]. To date, care bundles comprising the KDIGO recommendations have only been investigated in one study including 274 cardiac surgery patients at high risk for AKI as determined by AKI biomarkers. The study showed less postoperative AKI (although mainly by the urine output criteria) without, however, influencing any major patient-centred outcome like RRT or renal recovery at day 30 [294]. The treatment strategy included avoidance of nephrotoxins and hyperglycaemia as well as applying goal-directed haemodynamic optimisation. It is unclear which element was effective because goal-directed therapy (GDT) neither prevented AKI nor reduced the need for RRT in septic shock, as shown by a secondary analysis [23] and a meta-analysis of three recent large RCTs [295], but avoiding nephrotoxins, hyperglycaemia and hypovolaemia seems to be reasonable.
Conclusions and summary
Prompt resuscitation of the circulation with fluids, vasopressors and inotropes remains the cornerstone in the prevention of AKI. Volume expansion with isotonic crystalloids is only recommended in states of true and suspected hypovolaemia. Uncontrolled volume expansion and the use of starches and dextrans should be avoided. Following or together with fluid resuscitation hypotensive patients should be given a vasoconstrictor, preferably norepinephrine, and titrated individually with a target MAP of 65–70 mmHg being adequate in most individuals without pre-existing chronic hypertension. The potential role of vasopressin requires further investigation. Together with these measures a review of all medications with the cessation of those known to be nephrotoxic is mandatory. Diuretics should not be used for prevention of AKI alone but may benefit the kidney by relieving renal congestion. Frank hyperglycaemia should be avoided. The effect of statins appears to depend on the setting, with promising results in contrast administration but no effect or even harm in cardiac surgery. There is low-level evidence that the choice of the sedative may impact kidney function. The conflicting results on ischaemic preconditioning preclude a firm recommendation.
Heterogeneous definitions of AKI still hamper comparison of different studies, despite the commendable efforts by the ADQI, AKIN and KDIGO working groups [2, 296, 297]. In addition, AKI is frequently reported as a secondary outcome. Although several RCTs have fuelled the literature on prevention of AKI over the past 4–5 years, the available evidence remains insufficient. Many recommendations are therefore formulated as weak with low grade quality of evidence. More high-quality studies with consensus AKI definitions will be required to fill the knowledge gaps.
References
Chertow GM, Burdick E, Honour M (2005) Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16:3365–3370
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Kane-Gill SL, Sileanu FE, Murugan R, Trietley GS, Handler SM, Kellum JA (2015) Risk factors for acute kidney injury in older adults with critical illness: a retrospective cohort study. Am J Kidney Dis 65:860–869
Kirwan CJ, Blunden MJ, Dobbie H, James A, Nedungadi A, Prowle JR (2015) Critically ill patients requiring acute renal replacement therapy are at an increased risk of long-term renal dysfunction, but rarely receive specialist nephrology follow-up. Nephron 129:164–170
Joannidis M, Metnitz B, Bauer P, Schusterschitz N, Moreno R, Druml W, Metnitz PG (2009) Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med 35:1692–1702
Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, Edipidis K, Forni LG, Gomersall CD, Govil D, Honore PM, Joannes-Boyau O, Joannidis M, Korhonen AM, Lavrentieva A, Mehta RL, Palevsky P, Roessler E, Ronco C, Uchino S, Vazquez JA, Vidal Andrade E, Webb S, Kellum JA (2015) Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med 41:1411–1423
Piccinni P, Cruz DN, Gramaticopolo S, Garzotto F, Dal Santo M, Aneloni G, Rocco M, Alessandri E, Giunta F, Michetti V, Iannuzzi M, Belluomo Anello C, Brienza N, Carlini M, Pelaia P, Gabbanelli V, Ronco C, Investigators N (2011) Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiol 77:1072–1083
Srisawat N, Sileanu FE, Murugan R, Bellomod R, Calzavacca P, Cartin-Ceba R, Cruz D, Finn J, Hoste EE, Kashani K, Ronco C, Webb S, Kellum JA, Acute Kidney Injury-6 Study Group (2015) Variation in risk and mortality of acute kidney injury in critically ill patients: a multicenter study. Am J Nephrol 41:81–88
Bell S, Dekker FW, Vadiveloo T, Marwick C, Deshmukh H, Donnan PT, Van Diepen M (2015) Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery–development and validation of a risk score and effect of acute kidney injury on survival: observational cohort study. BMJ 351:h5639
Joannidis M, Druml W, Forni LG, Groeneveld AB, Honore P, Oudemans-van Straaten HM, Ronco C, Schetz MR, Woittiez AJ, Critical Care Nephrology Working Group of the European Society of Intensive Care Medicine (2010) Prevention of acute kidney injury and protection of renal function in the intensive care unit. Expert opinion of the Working Group for Nephrology, ESICM. Intensive Care Med 36:392–411
Ichai C, Vinsonneau C, Souweine B, Armando F, Canet E, Clec’h C, Constantin JM, Darmon M, Duranteau J, Gaillot T, Garnier A, Jacob L, Joannes-Boyau O, Juillard L, Journois D, Lautrette A, Muller L, Legrand M, Lerolle N, Rimmele T, Rondeau E, Tamion F, Walrave Y, Velly L, Société française d’anesthésie et de réanimation (Sfar), Société de réanimation de langue française (SRLF), Groupe francophone de réanimation et urgences pédiatriques (GFRUP), Société française de néphrologie (SFN) (2016) Acute kidney injury in the perioperative period and in intensive care units (excluding renal replacement therapies). Ann Intensive Care 6:48
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926
Guyatt GH, Oxman AD, Kunz R, Atkins D, Brozek J, Vist G, Alderson P, Glasziou P, Falck-Ytter Y, Schunemann HJ (2011) GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol 64:395–400
Guyatt GH, Schunemann HJ, Djulbegovic B, Akl EA (2015) Guideline panels should not GRADE good practice statements. J Clin Epidemiol 68:597–600
de Mendonca A, Vincent JL, Suter PM, Moreno R, Dearden NM, Antonelli M, Takala J, Sprung C, Cantraine F (2000) Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med 26:915–921
Guerin C, Girard R, Selli JM, Perdrix JP, Ayzac L (2000) Initial versus delayed acute renal failure in the intensive care unit. A multicenter prospective epidemiological study. Rhone-Alpes Area Study Group on Acute Renal Failure. Am J Respir Crit Care Med 161:872–879
Schwilk B, Wiedeck H, Stein B, Reinelt H, Treiber H, Bothner U (1997) Epidemiology of acute renal failure and outcome of haemodiafiltration in intensive care. Intensive Care Med 23:1204–1211
Himmelfarb J, Joannidis M, Molitoris B, Schietz M, Okusa MD, Warnock D, Laghi F, Goldstein SL, Prielipp R, Parikh CR, Pannu N, Lobo SM, Shah S, D’Intini V, Kellum JA (2008) Evaluation and initial management of acute kidney injury. Clin J Am Soc Nephrol 3:962–967
Joannidis M (2004) Drug-induced renal failure in the ICU. Int J Artif Organs 27:1034–1042
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP (2017) Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43:304–377
Prowle JR, Kirwan CJ, Bellomo R (2014) Fluid management for the prevention and attenuation of acute kidney injury. Nat Rev Nephrol 10:37–47
Ostermann M, Straaten HM, Forni LG (2015) Fluid overload and acute kidney injury: cause or consequence? Crit Care 19:443
Kellum JA, Chawla LS, Keener C, Singbartl K, Palevsky PM, Pike FL, Yealy DM, Huang DT, Angus DC, ProCESS and ProGReSS-AKI Investigators (2016) The effects of alternative resuscitation strategies on acute kidney injury in patients with septic shock. Am J Respir Crit Care Med 193:281–287
Chowdhury AH, Cox EF, Francis ST, Lobo DN (2012) A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and Plasma-lyte® 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann Surg 256:18–24
Wilkes NJ, Woolf R, Mutch M, Mallett SV, Peachey T, Stephens R, Mythen MG (2001) The effects of balanced versus saline-based hetastarch and crystalloid solutions on acid-base and electrolyte status and gastric mucosal perfusion in elderly surgical patients. Anesth Analg 93:811–816
Alphonsus CS, Rodseth RN (2014) The endothelial glycocalyx: a review of the vascular barrier. Anaesthesia 69:777–784
Chappell D, Jacob M (2014) Role of the glycocalyx in fluid management: small things matter. Best Pract Res Clin Anaesthesiol 28:227–234
Perner A, Prowle JR, Joannidis M, Young P, Hjortrup PB, Pettilä V (2017) Fluid management in acute kidney injury. Intensive Care Med. doi:10.1007/s00134-017-4817-x
Horgan KJ, Ottaviano YL, Watson AJ (1989) Acute renal-failure due to mannitol intoxication. Am J Nephrol 9:106–109
Rozich JD, Paul RV (1989) Acute renal failure precipitated by elevated colloid osmotic pressure. Am J Med 87:359–360
Legendre C, Thervet E, Page B, Percheron A, Noel LH, Kreis H (1993) Hydroxyethylstarch and osmotic-nephrosis-like lesions in kidney transplantation. Lancet 342:248–249
Cittanova ML, Leblanc I, Legendre C, Mouquet C, Riou B, Coriat P (1996) Effect of hydroxyethylstarch in brain-dead kidney donors on renal function in kidney-transplant recipients. Lancet 348:1620–1622
Skinsnes OK (1947) Gelatin nephrosis; renal tissue changes in man resulting from the intravenous administration of gelatin. Surg Gynecol Obstetri 85:563–571
Beyer R, Harmening U, Rittmeyer O, Zielmann S, Mielck F, Kazmaier S, Kettler D (1997) Use of modified fluid gelatin and hydroxyethyl starch for colloidal volume replacement in major orthopaedic surgery. Brit J Anaesth 78:44–50
Schortgen F, Lacherade JC, Bruneel F, Cattaneo I, Hemery F, Lemaire F, Brochard L (2001) Effects of hydroxyethylstarch and gelatin on renal function in severe sepsis: a multicentre randomised study. Lancet 357:911–916
Mardel SN, Saunders FM, Allen H, Menezes G, Edwards CM, Ollerenshaw L, Baddeley D, Kennedy A, Ibbotson RM (1998) Reduced quality of clot formation with gelatin-based plasma substitutes. Br J Anaesth 80:204–207
Tabuchi N, deHaan J, Huet RCGG, Boonstra PW, vanOeveren W (1995) Gelatin use impairs platelet adhesion during cardiac surgery. Thromb Haemostasis 74:1447–1451
Kurnik BR, Singer F, Groh WC (1991) Case report: dextran-induced acute anuric renal failure. Am J Med Sci 302:28–30
Laxenaire MC, Charpentier C, Feldman L (1994) Anaphylactoid reactions to colloid plasma substitutes: incidence, risk factors, mechanisms. A French multicenter prospective study. Ann Fr Anesth Reanim 13:301–310
Mailloux L, Swartz CD, Capizzi R, Kim KE, Onesti G, Ramirez O, Brest AN (1967) Acute renal failure after administration of low-molecular weight dextran. N Engl J Med 277:1113–1118
Messmer KFW (1987) The use of plasma substitutes with special attention to their side-effects. World J Surg 11:69–74
Fliser D, Zurbruggen I, Mutschler E, Bischoff I, Nussberger J, Franek E, Ritz E (1999) Coadministration of albumin and furosemide in patients with the nephrotic syndrome. Kidney Int 55:629–634
Inoue M, Okajima K, Itoh K, Ando Y, Watanabe N, Yasaka T, Nagase S, Morino Y (1987) Mechanism of furosemide resistance in analbuminemic rats and hypoalbuminemic patients. Kidney Int 32 (2):198–203
Wiedermann CJ, Dunzendorfer S, Gaioni LU, Zaraca F, Joannidis M (2010) Hyperoncotic colloids and acute kidney injury: a meta-analysis of randomized trials. Crit Care 14:R191
Wiedermann CJ, Joannidis M (2015) Nephroprotective potential of human albumin infusion: a narrative review. Gastroenterol Res Pract 2015:912839
Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, SAFE Study Investigators (2004) A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 350:2247–2256
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Serrano AB, Candela-Toha AM, Zamora J, Vera J, Muriel A, Del Rey JM, Liano F (2016) Preoperative hydration with 0.9% normal saline to prevent acute kidney injury after major elective open abdominal surgery: a randomised controlled trial. Eur J Anaesthesiol 33:436–443
Hjortrup PB, Haase N, Bundgaard H, Thomsen SL, Winding R, Pettila V, Aaen A, Lodahl D, Berthelsen RE, Christensen H, Madsen MB, Winkel P, Wetterslev J, Perner A, CLASSIC Trial Group; Scandinavian Critical Care Trials Group (2016) Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomised, parallel-group, multicentre feasibility trial. Intensive Care Med 42:1695–1705
Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M (2012) Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA 308:1566–1572
Shaw AD, Raghunathan K, Peyerl FW, Munson SH, Paluszkiewicz SM, Schermer CR (2014) Association between intravenous chloride load during resuscitation and in-hospital mortality among patients with SIRS. Intensive Care Med 40:1897–1905
Kellum JA, Lameire N, KDIGO AKI Guideline Work Group (2013) Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care 17:204
Young P, Bailey M, Beasley R, Henderson S, Mackle D, McArthur C, McGuinness S, Mehrtens J, Myburgh J, Psirides A, Reddy S, Bellomo R (2015) Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: the SPLIT randomized clinical trial. JAMA 314:1701–1710
Joannidis M, Forni LG (2016) Acute kidney injury: buffered crystalloids or saline in the ICU—a SPLIT decision. Nat Rev Nephrol 12:6–8
Semler MW, Wanderer JP, Ehrenfeld JM, Stollings JL, Self WH, Siew ED, Wang L, Byrne DW, Shaw AD, Bernard GR, Rice TW, SALT Investigators and the Pragmatic Critical Care Research Group (2017) Balanced crystalloids versus saline in the intensive care unit: the SALT randomized trial. Am J Respir Crit Care Med. doi: 10.1164/rccm.201607-1345OC
Haase M, Haase-Fielitz A, Bellomo R, Devarajan P, Story D, Matalanis G, Reade MC, Bagshaw SM, Seevanayagam N, Seevanayagam S, Doolan L, Buxton B, Dragun D (2009) Sodium bicarbonate to prevent increases in serum creatinine after cardiac surgery: a pilot double-blind, randomized controlled trial. Crit Care Med 37:39–47
McGuinness SP, Parke RL, Bellomo R, Van Haren FM, Bailey M (2013) Sodium bicarbonate infusion to reduce cardiac surgery-associated acute kidney injury: a phase II multicenter double-blind randomized controlled trial. Crit Care Med 41:1599–1607
Kristeller JL, Zavorsky GS, Prior JE, Keating DA, Brady MA, Romaldini TA, Hickman TL, Stahl RF (2013) Lack of effectiveness of sodium bicarbonate in preventing kidney injury in patients undergoing cardiac surgery: a randomized controlled trial. Pharmacotherapy 33:710–717
Haase M, Haase-Fielitz A, Plass M, Kuppe H, Hetzer R, Hannon C, Murray PT, Bailey MJ, Bellomo R, Bagshaw SM (2013) Prophylactic perioperative sodium bicarbonate to prevent acute kidney injury following open heart surgery: a multicenter double-blinded randomized controlled trial. PLoS Med 10:e1001426
Tie HT, Luo MZ, Luo MJ, Zhang M, Wu QC, Wan JY (2014) Sodium bicarbonate in the prevention of cardiac surgery-associated acute kidney injury: a systematic review and meta-analysis. Crit Care 18:517
Tian ML, Hu Y, Yuan J, Zha Y (2015) Efficacy and safety of perioperative sodium bicarbonate therapy for cardiac surgery-associated acute kidney injury: a meta-analysis. J Cardiovasc Pharmacol 65:130–136
Kim JH, Kim HJ, Kim JY, Ahn H, Ahn IM, Choe WJ, Lim CH (2015) Meta-analysis of sodium bicarbonate therapy for prevention of cardiac surgery-associated acute kidney injury. J Cardiothorac Vasc Anesth 29:1248–1256
Bailey M, McGuinness S, Haase M, Haase-Fielitz A, Parke R, Hodgson CL, Forbes A, Bagshaw SM, Bellomo R (2015) Sodium bicarbonate and renal function after cardiac surgery: a prospectively planned individual patient meta-analysis. Anesthesiology 122:294–306
Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, Glass P, Lipman J, Liu B, McArthur C, McGuinness S, Rajbhandari D, Taylor CB, Webb SA, CHEST Investigators, Australian and New Zealand Intensive Care Society Clinical Trials Group (2012) Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med 367:1901–1911
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K, German Competence Network Sepsis (SepNet) (2008) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 358:125–139
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, Madsen KR, Moller MH, Elkjaer JM, Poulsen LM, Bendtsen A, Winding R, Steensen M, Berezowicz P, Soe-Jensen P, Bestle M, Strand K, Wiis J, White JO, Thornberg KJ, Quist L, Nielsen J, Andersen LH, Holst LB, Thormar K, Kjaeldgaard AL, Fabritius ML, Mondrup F, Pott FC, Moller TP, Winkel P, Wetterslev J, 6S Trial Group, Scandinavian Critical Care Trials Group (2012) Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 367:124–134
Gattas DJ, Dan A, Myburgh J, Billot L, Lo S, Finfer S, CHEST Management Committee (2013) Fluid resuscitation with 6% hydroxyethyl starch (130/0.4 and 130/0.42) in acutely ill patients: systematic review of effects on mortality and treatment with renal replacement therapy. Intensive Care Med 39:558–568
Zarychanski R, Abou-Setta AM, Turgeon AF, Houston BL, McIntyre L, Marshall JC, Fergusson DA (2013) Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation: a systematic review and meta-analysis. JAMA 309:678–688
Rochwerg B, Alhazzani W, Gibson A, Ribic CM, Sindi A, Heels-Ansdell D, Thabane L, Fox-Robichaud A, Mbuagbaw L, Szczeklik W, Alshamsi F, Altayyar S, Ip W, Li G, Wang M, Wludarczyk A, Zhou Q, Annane D, Cook DJ, Jaeschke R, Guyatt GH (2015) Fluid type and the use of renal replacement therapy in sepsis: a systematic review and network meta-analysis. Intensive Care Med 41:1561–1571
Haase N, Perner A, Hennings LI, Siegemund M, Lauridsen B, Wetterslev M, Wetterslev J (2013) Hydroxyethyl starch 130/0.38-0.45 versus crystalloid or albumin in patients with sepsis: systematic review with meta-analysis and trial sequential analysis. BMJ 346:f839
Mutter TC, Ruth CA, Dart AB (2013) Hydroxyethyl starch (HES) versus other fluid therapies: effects on kidney function. Cochrane Database Syst Rev 7:CD007594. doi:10.1002/14651858.CD007594.pub3.
Reinhart K, Perner A, Sprung CL, Jaeschke R, Schortgen F, Johan Groeneveld AB, Beale R, Hartog CS, European Society of Intensive Care Medicine (2012) Consensus statement of the ESICM task force on colloid volume therapy in critically ill patients. Intensive Care Med 38:368–383
Moeller C, Fleischmann C, Thomas-Rueddel D, Vlasakov V, Rochwerg B, Theurer P, Gattinoni L, Reinhart K, Hartog CS (2016) How safe is gelatin? A systematic review and meta-analysis of gelatin-containing plasma expanders vs crystalloids and albumin. J Crit Care 35:75–83
Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, Fanizza C, Caspani L, Faenza S, Grasselli G, Iapichino G, Antonelli M, Parrini V, Fiore G, Latini R, Gattinoni L, ALBIOS Study Investigators (2014) Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 370:1412–1421
Dubois MJ, Orellana-Jimenez C, Melot C, De Backer D, Berre J, Leeman M, Brimioulle S, Appoloni O, Creteur J, Vincent JL (2006) Albumin administration improves organ function in critically ill hypoalbuminemic patients: a prospective, randomized, controlled, pilot study. Crit Care Med 34:2536–2540
Wiedermann CJ, Joannidis M (2014) Albumin replacement in severe sepsis or septic shock. N Engl J Med 371:83
Patel A, Laffan MA, Waheed U, Brett SJ (2014) Randomised trials of human albumin for adults with sepsis: systematic review and meta-analysis with trial sequential analysis of all-cause mortality. BMJ 349:g4561
Lee EH, Kim WJ, Kim JY, Chin JH, Choi DK, Sim JY, Choo SJ, Chung CH, Lee JW, Choi IC (2016) Effect of exogenous albumin on the incidence of postoperative acute kidney injury in patients undergoing off-pump coronary artery bypass surgery with a preoperative albumin level of less than 4.0 g/dl. Anesthesiology 124:1001–1011
Pannu N, Nadim MK (2008) An overview of drug-induced acute kidney injury. Crit Care Med 36:S216–223
Perazella MA, Luciano RL (2015) Review of select causes of drug-induced AKI. Expert Rev Clin Pharmacol 8(4):367–371
Branch RA (1988) Prevention of amphotericin-B induced renal impairment. A review on the use of sodium supplementation. Arch Intern Med 148:2389–2394
Cheung TW, Jayaweera DT, Pearce D, Benson P, Nahass R, Olson C, Wool GM (2000) Safety of oral versus intravenous hydration during induction therapy with intravenous foscarnet in AIDS patients with cytomegalovirus infections. Int J STD AIDS 11:640–647
Safrin S, Cherrington J, Jaffe HS (1999) Cidofovir. Review of current and potential clinical uses. Adv Exp Med Biol 458:111–120
Perazella MA (1999) Crystal-induced acute renal failure. Am J Med 106:459–465
Solomon R, Werner C, Mann D, D’Elia J, Silva P (1994) Effects of saline, mannitol, and furosemide on acute decreases in renal function induced by radiocontrast agents. N Engl J Med 331:1416–1420
Mueller C, Buerkle G, Buettner HJ, Petersen J, Perruchoud AP, Eriksson U, Marsch S, Roskamm H (2002) Prevention of contrast media-associated nephropathy: randomized comparison of 2 hydration regimens in 1620 patients undergoing coronary angioplasty. Arch Intern Med 162:329–336
Merten GJ, Burgess WP, Gray LV, Holleman JH, Roush TS, Kowalchuk GJ, Bersin RM, Van Moore A, Simonton CA 3rd, Rittase RA, Norton HJ, Kennedy TP (2004) Prevention of contrast-induced nephropathy with sodium bicarbonate: a randomized controlled trial. JAMA 291:2328–2334
Ozcan EE, Guneri S, Akdeniz B, Akyildiz IZ, Senaslan O, Baris N, Aslan O, Badak O (2007) Sodium bicarbonate, N-acetylcysteine, and saline for prevention of radiocontrast-induced nephropathy. A comparison of 3 regimens for protecting contrast-induced nephropathy in patients undergoing coronary procedures. A single-center prospective controlled trial. Am Heart J 154:539–544
Masuda M, Yamada T, Mine T, Morita T, Tamaki S, Tsukamoto Y, Okuda K, Iwasaki Y, Hori M, Fukunami M (2007) Comparison of usefulness of sodium bicarbonate versus sodium chloride to prevent contrast-induced nephropathy in patients undergoing an emergent coronary procedure. Am J Cardiol 100:781–786
Briguori C, Airoldi F, D’Andrea D, Bonizzoni E, Morici N, Focaccio A, Michev I, Montorfano M, Carlino M, Cosgrave J, Ricciardelli B, Colombo A (2007) Renal Insufficiency Following Contrast Media Administration Trial (REMEDIAL): a randomized comparison of 3 preventive strategies. Circulation 115:1211–1217
Nijssen EC, Rennenberg RJ, Nelemans PJ, Essers BA, Janssen MM, Vermeeren MA, Ommen VV, Wildberger JE (2017) Prophylactic hydration to protect renal function from intravascular iodinated contrast material in patients at high risk of contrast-induced nephropathy (AMACING): a prospective, randomised, phase 3, controlled, open-label, non-inferiority trial. Lancet 389:1312–1322
Newhouse JH, Kho D, Rao QA, Starren J (2008) Frequency of serum creatinine changes in the absence of iodinated contrast material: implications for studies of contrast nephrotoxicity. AJR Am J Roentgenol 191:376–382
Wilhelm-Leen E, Montez-Rath ME, Chertow G (2017) Estimating the risk of radiocontrast-associated nephropathy. J Am Soc Nephrol 28:653–659
Hoste EA, Doom S, De Waele J, Delrue LJ, Defreyne L, Benoit DD, Decruyenaere J (2011) Epidemiology of contrast-associated acute kidney injury in ICU patients: a retrospective cohort analysis. Intensive Care Med 37:1921–1931
Cely CM, Schein RM, Quartin AA (2012) Risk of contrast induced nephropathy in the critically ill: a prospective, case matched study. Crit Care 16:R67
Ehrmann S, Badin J, Savath L, Pajot O, Garot D, Pham T, Capdevila X, Perrotin D, Lakhal K (2013) Acute kidney injury in the critically ill: is iodinated contrast medium really harmful? Crit Care Med 41:1017–1026
McDonald JS, McDonald RJ, Williamson EE, Kallmes DF, Kashani K (2017) Post-contrast acute kidney injury in intensive care unit patients: a propensity score-adjusted study. Intensive Care Med. doi:10.1007/s00134-017-4699-y
Hinson JS, Ehmann MR, Fine DM, Fishman EK, Toerper MF, Rothman RE, Klein EY (2017) Risk of acute kidney injury after intravenous contrast media administration. Ann Emerg Med 69:577–586.e4
Ehrmann S, Quartin A, Hobbs BP, Robert-Edan V, Cely C, Bell C, Lyons G, Pham T, Schein R, Geng Y, Lakhal K, Ng CS (2017) Contrast-associated acute kidney injury in the critically ill: systematic review and Bayesian meta-analysis. Intensive Care Med. doi:10.1007/s00134-017-4700-9
Valette X, Desmeulles I, Savary B, Masson R, Seguin A, Sauneuf B, Brunet J, Verrier P, Pottier V, Orabona M, Samba D, Viquesnel G, Lermuzeaux M, Hazera P, Dutheil JJ, Hanouz JL, Parienti JJ, du Cheyron D (2017) Sodium bicarbonate versus sodium chloride for preventing contrast-associated acute kidney injury in critically ill patients: a randomized controlled trial. Crit Care Med 45:637–644
Liu Y, Li H, Chen S, Chen J, Tan N, Zhou Y, Liu Y, Ye P, Ran P, Duan C, Chen P (2016) Excessively high hydration volume may not be associated with decreased risk of contrast-induced acute kidney injury after percutaneous coronary intervention in patients with renal insufficiency. J Am Heart Assoc. doi:10.1161/JAHA.115.003171
Bagshaw SM, Delaney A, Jones D, Ronco C, Bellomo R (2007) Diuretics in the management of acute kidney injury: a multinational survey. Contrib Nephrol 156:236–249
Bayati A, Nygren K, Kallskog O, Wolgast M (1990) The effect of loop diuretics on the long-term outcome of post-ischaemic acute renal failure in the rat. Acta Physiol Scand 139:271–279
Heyman SN, Rosen S, Epstein FH, Spokes K, Brezis ML (1994) Loop diuretics reduce hypoxic damage to proximal tubules of the isolated perfused rat kidney. Kidney Int 45:981–985
Kramer HJ, Schuurmann J, Wassermann C, Dusing R (1980) Prostaglandin-independent protection by furosemide from oliguric ischemic renal failure in conscious rats. Kidney Int 17:455–464
Legrand M, Dupuis C, Simon C, Gayat E, Mateo J, Lukaszewicz AC, Payen D (2013) Association between systemic hemodynamics and septic acute kidney injury in critically ill patients: a retrospective observational study. Crit Care 17:R278
Chen KP, Cavender S, Lee J, Feng M, Mark RG, Celi LA, Mukamal KJ, Danziger J (2016) Peripheral edema, central venous pressure, and risk of AKI in critical illness. Clinic J Am Soc Nephrol 11:602–608
Wu YF, Zheng YP, Zhang N, Liu H, Zheng QX, Yang FT, Wu YF (2015) Study on the correlation between the changes in intra-abdominal pressure and renal functional in the patients with abdominal compartment syndrome. Eur Rev Med Pharmacol Sci 19:3682–3687
Cordemans C, De Laet I, Van Regenmortel N, Schoonheydt K, Dits H, Huber W, Malbrain ML (2012) Fluid management in critically ill patients: the role of extravascular lung water, abdominal hypertension, capillary leak, and fluid balance. Ann Intensive Care 2:S1
Chawla LS, Davison DL, Brasha-Mitchell E, Koyner JL, Arthur JM, Shaw AD, Tumlin JA, Trevino SA, Kimmel PL, Seneff MG (2013) Development and standardization of a furosemide stress test to predict the severity of acute kidney injury. Crit Care 17:R207
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Lassnigg A, Donner E, Grubhofer G, Presterl E, Druml W, Hiesmayr M (2000) Lack of renoprotective effects of dopamine and furosemide during cardiac surgery. J Am Soc Nephrol 11:97–104
Brown CB, Ogg CS, Cameron JS (1981) High dose frusemide in acute renal failure: a controlled trial. Clin Nephrol 15:90–96
Ho KM, Power BM (2010) Benefits and risks of furosemide in acute kidney injury. Anaesthesia 65:283–293
Felker GM, Lee KL, Bull DA, Redfield MM, Stevenson LW, Goldsmith SR, LeWinter MM, Deswal A, Rouleau JL, Ofili EO, Anstrom KJ, Hernandez AF, McNulty SE, Velazquez EJ, Kfoury AG, Chen HH, Givertz MM, Semigran MJ, Bart BA, Mascette AM, Braunwald E, O’Connor CM, NHLBI Heart Failure Clinical Research Network (2011) Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med 364:797–805
Cotter G, Weissgarten J, Metzkor E, Moshkovitz Y, Litinski I, Tavori U, Perry C, Zaidenstein R, Golik A (1997) Increased toxicity of high-dose furosemide versus low-dose dopamine in the treatment of refractory congestive heart failure. Clin Pharmacol Ther 62:187–193
Hager B, Betschart M, Krapf R (1996) Effect of postoperative intravenous loop diuretic on renal function after major surgery. Schweiz Med Wochenschr 126:666–673
van der Voort PHJ, Boerma EC, Koopmans M, Zandberg M, de Ruiter J, Gerritsen RT, Egbers PH, Kingma WP, Kuiper MA (2009) Furosemide does not improve renal recovery after hemofiltration for acute renal failure in critically ill patients: a double blind randomized controlled trial. Crit Care Med 37:533–538
Ahsan N, Palmer BF, Wheeler D, Greenlee RG Jr, Toto RD (1994) Intravenous immunoglobulin-induced osmotic nephrosis. Arch Intern Med 154:1985–1987
Shilliday IR, Quinn KJ, Allison ME (1997) Loop diuretics in the management of acute renal failure: a prospective, double-blind, placebo-controlled, randomized study. Nephrol Dial Transplant 12:2592–2596
Sirivella S, Gielchinsky I, Parsonnet V (2000) Mannitol, furosemide, and dopamine infusion in postoperative renal failure complicating cardiac surgery. Ann Thorac Surg 69:501–506
Ho KM, Sheridan DJ (2006) Meta-analysis of frusemide to prevent or treat acute renal failure. BMJ 333:420
Bagshaw SM, Delaney A, Haase M, Ghali WA, Bellomo R (2007) Loop diuretics in the management of acute renal failure: a systematic review and meta-analysis. Crit Care Resusc 9:60–68
Sampath S, Moran JL, Graham PL, Rockliff S, Bersten AD, Abrams KR (2007) The efficacy of loop diuretics in acute renal failure: assessment using Bayesian evidence synthesis techniques. Crit Care Med 35:2516–2524
Asfar P, Meziani F, Hamel JF, Grelon F, Megarbane B, Anguel N, Mira JP, Dequin PF, Gergaud S, Weiss N, Legay F, Le Tulzo Y, Conrad M, Robert R, Gonzalez F, Guitton C, Tamion F, Tonnelier JM, Guezennec P, Van Der Linden T, Vieillard-Baron A, Mariotte E, Pradel G, Lesieur O, Ricard JD, Herve F, du Cheyron D, Guerin C, Mercat A, Teboul JL, Radermacher P, Investigators S (2014) High versus low blood-pressure target in patients with septic shock. N Engl J Med 370:1583–1593
Qureshi AI, Palesch YY, Suarez JI (2016) Intensive blood-pressure lowering in cerebral hemorrhage. N Eng J Med 375:e48
De Backer D, Biston P, Devriendt J, Madl C, Chochrad D, Aldecoa C, Brasseur A, Defrance P, Gottignies P, Vincent JL, SOAP II Investigators (2010) Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med 362:779–789
Serpa Neto A, Nassar AP, Cardoso SO, Manetta JA, Pereira VG, Esposito DC, Damasceno MC, Russell JA (2012) Vasopressin and terlipressin in adult vasodilatory shock: a systematic review and meta-analysis of nine randomized controlled trials. Crit Care 16:R154
Bragadottir G, Redfors B, Nygren A, Sellgren J, Ricksten SE (2009) Low-dose vasopressin increases glomerular filtration rate, but impairs renal oxygenation in post-cardiac surgery patients. Acta Anaesthesiol Scand 53:1052–1059
Russell JA, Walley KR, Singer J, Gordon AC, Hebert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D, VASST Investigators (2008) Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med 358:877–887
Gordon AC, Russell JA, Walley KR, Singer J, Ayers D, Storms MM, Holmes CL, Hebert PC, Cooper DJ, Mehta S, Granton JT, Cook DJ, Presneill JJ (2010) The effects of vasopressin on acute kidney injury in septic shock. Intensive Care Med 36:83–91
Gordon AC, Mason AJ, Thirunavukkarasu N, Perkins GD, Cecconi M, Cepkova M, Pogson DG, Aya HD, Anjum A, Frazier GJ, Santhakumaran S, Ashby D, Brett SJ, VANISH Investigators (2016) Effect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: the VANISH randomized clinical trial. JAMA 316:509–518
Hajjar LA, Vincent JL, Barbosa Gomes Galas FR, Rhodes A, Landoni G, Osawa EA, Melo RR, Sundin MR, Grande SM, Gaiotto FA, Pomerantzeff PM, Dallan LO, Franco RA, Nakamura RE, Lisboa LA, de Almeida JP, Gerent AM, Souza DH, Gaiane MA, Fukushima JT, Park CL, Zambolim C, Rocha Ferreira GS, Strabelli TM, Fernandes FL, Camara L, Zeferino S, Santos VG, Piccioni MA, Jatene FB, Costa Auler JO Jr, Filho RK (2017) Vasopressin versus norepinephrine in patients with vasoplegic shock after cardiac surgery: the VANCS randomized controlled trial. Anesthesiology 126:85–93
Ramaswamy D, Corrigan G, Polhemus C, Boothroyd D, Scandling J, Sommer FG, Alfrey E, Higgins J, Deen WM, Olshen R, Myers BD (2002) Maintenance and recovery stages of postischemic acute renal failure in humans. Am J Physiol Renal Physiol 282:F271–F280
Conger J, Robinette J, Villar A, Raij L, Shultz P (1995) Increased nitric oxide synthase activity despite lack of response to endothelium-dependent vasodilators in postischemic acute renal failure in rats. J Clin Invest 96:631–638
Wan L, Bagshaw SM, Langenberg C, Saotome T, May C, Bellomo R (2008) Pathophysiology of septic acute kidney injury: what do we really know? Crit Care Med 36:S198–S203
Ishikawa K, May CN, Gobe G, Langenberg C, Bellomo R (2010) Pathophysiology of septic acute kidney injury: a different view of tubular injury. Contrib Nephrol 165:18–27
Legrand M, Bezemer R, Kandil A, Demirci C, Payen D, Ince C (2011) The role of renal hypoperfusion in development of renal microcirculatory dysfunction in endotoxemic rats. Intensive Care Med 37:1534–1542
Molitoris BA, Sutton TA (2004) Endothelial injury and dysfunction: role in the extension phase of acute renal failure. Kidney Int 66:496–499
Lauschke A, Teichgraber UKM, Frei U, Eckardt KU (2006) ‘Low-dose’ dopamine worsens renal perfusion in patients with acute renal failure. Kidney Int 69:1669–1674
Friedrich JO, Adhikari N, Herridge MS, Beyene J (2005) Meta-analysis: low-dose dopamine increases urine output but does not prevent renal dysfunction or death. Ann Intern Med 142:510–524
Karthik S, Lisbon A (2006) Low-dose dopamine in the intensive care unit. Semin Dial 19:465–471
Holmes CL, Walley KR (2003) Bad medicine: low-dose dopamine in the ICU. Chest 123:1266–1275
Landoni G, Biondi-Zoccai GG, Tumlin JA, Bove T, De Luca M, Calabro MG, Ranucci M, Zangrillo A (2007) Beneficial impact of fenoldopam in critically ill patients with or at risk for acute renal failure: a meta-analysis of randomized clinical trials. Am J Kidney Dis 49:56–68
Zangrillo A, Biondi-Zoccai GG, Frati E, Covello RD, Cabrini L, Guarracino F, Ruggeri L, Bove T, Bignami E, Landoni G (2012) Fenoldopam and acute renal failure in cardiac surgery: a meta-analysis of randomized placebo-controlled trials. J Cardiothorac Vasc Anesth 26:407–413
Gillies MA, Kakar V, Parker RJ, Honore PM, Ostermann M (2015) Fenoldopam to prevent acute kidney injury after major surgery-a systematic review and meta-analysis. Crit Care 19:449
Bove T, Zangrillo A, Guarracino F, Alvaro G, Persi B, Maglioni E, Galdieri N, Comis M, Caramelli F, Pasero DC, Pala G, Renzini M, Conte M, Paternoster G, Martinez B, Pinelli F, Frontini M, Zucchetti MC, Pappalardo F, Amantea B, Camata A, Pisano A, Verdecchia C, Dal CE, Cariello C, Faita L, Baldassarri R, Scandroglio AM, Saleh O, Lembo R, Calabro MG, Bellomo R, Landoni G (2014) Effect of fenoldopam on use of renal replacement therapy among patients with acute kidney injury after cardiac surgery: a randomized clinical trial. JAMA 312:2244–2253
Sward K, Valson F, Ricksten SE (2001) Long-term infusion of atrial natriuretic peptide (ANP) improves renal blood flow and glomerular filtration rate in clinical acute renal failure. Acta Anaesthesiol Scand 45:536–542
Sward K, Valsson F, Sellgren J, Ricksten SE (2005) Differential effects of human atrial natriuretic peptide and furosemide on glomerular filtration rate and renal oxygen consumption in humans. Intensive Care Med 31:79–85
Houben AJ, van der Zander K, de Leeuw PW (2005) Vascular and renal actions of brain natriuretic peptide in man: physiology and pharmacology. Fundam Clin Pharmacol 19:411–419
Kuhn M (2012) Endothelial actions of atrial and B-type natriuretic peptides. Br J Pharmacol 166:522–531
Mitaka C, Kudo T, Haraguchi G, Tomita M (2011) Cardiovascular and renal effects of carperitide and nesiritide in cardiovascular surgery patients: a systematic review and meta-analysis. Crit Care 15:R258
Patel NN, Rogers CA, Angelini GD, Murphy GJ (2011) Pharmacological therapies for the prevention of acute kidney injury following cardiac surgery: a systematic review. Heart Fail Rev 16:553–567
Nigwekar SU, Navaneethan SD, Parikh CR, Hix JK (2009) Atrial natriuretic peptide for preventing and treating acute kidney injury. Cochrane Database Syst Rev CD006028. doi:10.1002/14651858.CD006028.pub2
Sezai A, Nakata K, Iida M, Yoshitake I, Wakui S, Hata H, Shiono M (2013) Results of low-dose carperitide infusion in high-risk patients undergoing coronary artery bypass grafting. Ann Thorac Surg 96:119–126
Mori Y, Kamada T, Ochiai R (2014) Reduction in the incidence of acute kidney injury after aortic arch surgery with low-dose atrial natriuretic peptide: a randomised controlled trial. Eur J Anaesthesiol 31:381–387
Xiong B, Wang C, Yao Y, Huang Y, Tan J, Cao Y, Zou Y, Huang J (2015) The dose-dependent effect of nesiritide on renal function in patients with acute decompensated heart failure: a systematic review and meta-analysis of randomized controlled trials. PLoS One 10:e0131326
Papp Z, Edes I, Fruhwald S, De Hert SG, Salmenpera M, Leppikangas H, Mebazaa A, Landoni G, Grossini E, Caimmi P, Morelli A, Guarracino F, Schwinger RH, Meyer S, Algotsson L, Wikstrom BG, Jorgensen K, Filippatos G, Parissis JT, Gonzalez MJ, Parkhomenko A, Yilmaz MB, Kivikko M, Pollesello P, Follath F (2012) Levosimendan: molecular mechanisms and clinical implications: consensus of experts on the mechanisms of action of levosimendan. Int J Cardiol 159:82–87
Hasslacher J, Bijuklic K, Bertocchi C, Kountchev J, Bellmann R, Dunzendorfer S, Joannidis M (2011) Levosimendan inhibits release of reactive oxygen species in polymorphonuclear leukocytes in vitro and in patients with acute heart failure and septic shock: a prospective observational study. Crit Care 15:R166
Bove T, Matteazzi A, Belletti A, Paternoster G, Saleh O, Taddeo D, Dossi R, Greco T, Bradic N, Husedzinovic I, Nigro Neto C, Lomivorotov VV, Calabro MG (2015) Beneficial impact of levosimendan in critically ill patients with or at risk for acute renal failure: a meta-analysis of randomized clinical trials. Heart Lung Vessel 7:35–46
Zhou C, Gong J, Chen D, Wang W, Liu M, Liu B (2016) Levosimendan for prevention of acute kidney injury after cardiac surgery: a meta-analysis of randomized controlled trials. Am J Kidney Dis 67:408–416
Gordon AC, Perkins GD, Singer M, McAuley DF, Orme RM, Santhakumaran S, Mason AJ, Cross M, Al-Beidh F, Best-Lane J, Brealey D, Nutt CL, McNamee JJ, Reschreiter H, Breen A, Liu KD, Ashby D (2016) Levosimendan for the prevention of acute organ dysfunction in sepsis. N Engl J Med 375:1638–1648
Mehta RH, Leimberger JD, van Diepen S, Meza J, Wang A, Jankowich R, Harrison RW, Hay D, Fremes S, Duncan A, Soltesz EG, Luber J, Park S, Argenziano M, Murphy E, Marcel R, Kalavrouziotis D, Nagpal D, Bozinovski J, Toller W, Heringlake M, Goodman SG, Levy JH, Harrington RA, Anstrom KJ, Alexander JH, LEVO-CTS Investigators (2017) Levosimendan in patients with left ventricular dysfunction undergoing cardiac surgery. N Engl J Med. doi:10.1056/NEJMoa1616218
Landoni G, Lomivorotov VV, Alvaro G, Lobreglio R, Pisano A, Guarracino F, Calabro MG, Grigoryev EV, Likhvantsev VV, Salgado-Filho MF, Bianchi A, Pasyuga VV, Baiocchi M, Pappalardo F, Monaco F, Boboshko VA, Abubakirov MN, Amantea B, Lembo R, Brazzi L, Verniero L, Bertini P, Scandroglio AM, Bove T, Belletti A, Michienzi MG, Shukevich DL, Zabelina TS, Bellomo R, Zangrillo A, CHEETAH Study Group (2017) Levosimendan for hemodynamic support after cardiac surgery. N Engl J Med. doi:10.1056/NEJMoa1616325
Luo C, Yuan D, Li X, Yao W, Luo G, Chi X, Li H, Irwin MG, Xia Z, Hei Z (2015) Propofol attenuated acute kidney injury after orthotopic liver transplantation via inhibiting gap junction composed of connexin 32. Anesthesiology 122:72–86
Hsing CH, Chou W, Wang JJ, Chen HW, Yeh CH (2011) Propofol increases bone morphogenetic protein-7 and decreases oxidative stress in sepsis-induced acute kidney injury. Nephrol Dial Transplant 26:1162–1172
Villela NR, Nascimento Junior P, Carvalho LR, Teixeira A (2005) Effects of dexmedetomidine on renal system and on vasopressin plasma levels. Experimental study in dogs. Rev Bras Anestesiol 55:429–440
Billings FT, Chen SW, Kim M, Park SW, Song JH, Wang S, Herman J, D’Agati V, Lee HT (2008) alpha2-Adrenergic agonists protect against radiocontrast-induced nephropathy in mice. Am J Physiol Renal Physiol 295:F741–748
Hsing CH, Lin CF, So E, Sun DP, Chen TC, Li CF, Yeh CH (2012) alpha2-Adrenoceptor agonist dexmedetomidine protects septic acute kidney injury through increasing BMP-7 and inhibiting HDAC2 and HDAC5. Am J Physiol Renal Physiol 303:F1443–F1453
Tan F, Chen Y, Yuan D, Gong C, Li X, Zhou S (2015) Dexmedetomidine protects against acute kidney injury through downregulating inflammatory reactions in endotoxemia rats. Biomed Rep 3:365–370
Yao H, Chi X, Jin Y, Wang Y, Huang P, Wu S, Xia Z, Cai J (2015) Dexmedetomidine inhibits TLR4/NF-kappaB activation and reduces acute kidney injury after orthotopic autologous liver transplantation in rats. Sci Rep 5:16849
Reade MC, Finfer S (2014) Sedation and delirium in the intensive care unit. N Engl J Med 370:444–454
Mirrakhimov AE, Voore P, Halytskyy O, Khan M, Ali AM (2015) Propofol infusion syndrome in adults: a clinical update. Crit Care Res Pract 2015:260385
Krajcova A, Waldauf P, Andel M, Duska F (2015) Propofol infusion syndrome: a structured review of experimental studies and 153 published case reports. Crit Care 19:398
Cremer OL, Moons KG, Bouman EA, Kruijswijk JE, de Smet AM, Kalkman CJ (2001) Long-term propofol infusion and cardiac failure in adult head-injured patients. Lancet 357:117–118
Leite TT, Macedo E, Martins Ida S, Neves FM, Liborio AB (2015) Renal outcomes in critically ill patients receiving propofol or midazolam. Clin J Am Soc Nephrol 10:1937–1945
Yoo YC, Shim JK, Song Y, Yang SY, Kwak YL (2014) Anesthetics influence the incidence of acute kidney injury following valvular heart surgery. Kidney Int 86:414–422
Menting TP, Wever KE, Ozdemir-van Brunschot DM, Van der Vliet DJ, Rovers MM, Warle MC (2017) Ischaemic preconditioning for the reduction of renal ischaemia reperfusion injury. Cochrane Database Syst Rev 3:Cd010777
Pichot C, Longrois D, Ghignone M, Quintin L (2012) Dexmedetomidine and clonidine: a review of their pharmacodynamy to define their role for sedation in intensive care patients. Ann Fr Anesth Reanim 31:876–896
Leino K, Hynynen M, Jalonen J, Salmenpera M, Scheinin H, Aantaa R, Dexmedetomidine in Cardiac Surgery Study Group (2011) Renal effects of dexmedetomidine during coronary artery bypass surgery: a randomized placebo-controlled study. BMC Anesthesiol 11:9
Ji F, Li Z, Young JN, Yeranossian A, Liu H (2013) Post-bypass dexmedetomidine use and postoperative acute kidney injury in patients undergoing cardiac surgery with cardiopulmonary bypass. PLoS One 8:e77446
Moon T, Tsai JY, Vachhani S, Peng SP, Feng L, Vaporciyan AA, Cata JP (2016) The use of intraoperative dexmedetomidine is not associated with a reduction in acute kidney injury after lung cancer surgery. J Cardiothorac Vasc Anesth 30:51–55
Balkanay OO, Goksedef D, Omeroglu SN, Ipek G (2015) The dose-related effects of dexmedetomidine on renal functions and serum neutrophil gelatinase-associated lipocalin values after coronary artery bypass grafting: a randomized, triple-blind, placebo-controlled study. Interact Cardiovasc Thorac Surg 20:209–214
Cho JS, Shim JK, Soh S, Kim MK, Kwak YL (2016) Perioperative dexmedetomidine reduces the incidence and severity of acute kidney injury following valvular heart surgery. Kidney Int 89:693–700
Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE (2002) Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 87:978–982
Krinsley JS (2003) Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc 78:1471–1478
van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R (2001) Intensive insulin therapy in critically ill patients. N Engl J Med 345:1359–1367
Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, Van Wijngaerden E, Bobbaers H, Bouillon R (2006) Intensive insulin therapy in the medical ICU. N Engl J Med 354:449–461
Schetz M, Vanhorebeek I, Wouters PJ, Wilmer A, van den Berghe G (2008) Tight blood glucose control is renoprotective in critically ill patients. J Am Soc Nephrol 19: 571–578
Arabi YM, Dabbagh OC, Tamim HM, Al-Shimemeri AA, Memish ZA, Haddad SH, Syed SJ, Giridhar HR, Rishu AH, Al-Daker MO, Kahoul SH, Britts RJ, Sakkijha MH (2008) Intensive versus conventional insulin therapy: a randomized controlled trial in medical and surgical critically ill patients. Crit Care Med 36:3190–3197
Investigators N-SS, Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hebert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ (2009) Intensive versus conventional glucose control in critically ill patients. N Engl J Med 360:1283–1297
Preiser JC, Devos P, Ruiz-Santana S, Melot C, Annane D, Groeneveld J, Iapichino G, Leverve X, Nitenberg G, Singer P, Wernerman J, Joannidis M, Stecher A, Chiolero R (2009) A prospective randomised multi-centre controlled trial on tight glucose control by intensive insulin therapy in adult intensive care units: the Glucontrol study. Intensive Care Med 35:1738–1748
Arabi YM, Tamim HM, Dhar GS, Al-Dawood A, Al-Sultan M, Sakkijha MH, Kahoul SH, Brits R (2011) Permissive underfeeding and intensive insulin therapy in critically ill patients: a randomized controlled trial. Am J Clin Nutr 93:569–577
De La Rosa GC, Donado JH, Restrepo AH, Quintero AM, Gonzalez LG, Saldarriaga NE, Bedoya M, Toro JM, Velasquez JB, Valencia JC, Arango CM, Aleman PH, Vasquez EM, Chavarriaga JC, Yepes A, Pulido W, Cadavid CA (2008) Strict glycaemic control in patients hospitalised in a mixed medical and surgical intensive care unit: a randomised clinical trial. Crit Care 12:R120
Van den Berghe G, Schetz M, Vlasselaers D, Hermans G, Wilmer A, Bouillon R, Mesotten D (2009) Clinical review: intensive insulin therapy in critically ill patients: NICE-SUGAR or Leuven blood glucose target? J Clin Endocrinol Metab 94:3163–3170
Ling Y, Li X, Gao X (2012) Intensive versus conventional glucose control in critically ill patients: a meta-analysis of randomized controlled trials. Eur J Intern Med 23:564–574
Dickerson RN, Hamilton LA, Connor KA, Maish GO 3rd, Croce MA, Minard G, Brown RO (2011) Increased hypoglycemia associated with renal failure during continuous intravenous insulin infusion and specialized nutritional support. Nutrition 27:766–772
Kosiborod M, Inzucchi SE, Goyal A, Krumholz HM, Masoudi FA, Xiao L, Spertus JA (2009) Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA 301:1556–1564
Mowery NT, Guillamondegui OD, Gunter OL, Diaz JJ Jr, Collier BR, Dossett LA, Dortch MJ, May AK (2010) Severe hypoglycemia while on intensive insulin therapy is not an independent predictor of death after trauma. J Trauma 68:342–347
NICE-SUGAR Study Investigators, Finfer S, Liu B, Chittock DR, Norton R, Myburgh JA, McArthur C, Mitchell I, Foster D, Dhingra V, Henderson WR, Ronco JJ, Bellomo R, Cook D, McDonald E, Dodek P, Hebert PC, Heyland DK, Robinson BG (2012) Hypoglycemia and risk of death in critically ill patients. N Engl J Med 367:1108–1118
Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, Inzucchi SE, Ismail-Beigi F, Kirkman MS, Umpierrez GE (2009) American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. EndocrPract 15:353–369
van den Berghe G (2013) What’s new in glucose control in the ICU? Intensive Care Med 39:823–825
Dieleman JM, Nierich AP, Rosseel PM, van der Maaten JM, Hofland J, Diephuis JC, Schepp RM, Boer C, Moons KG, van Herwerden LA, Tijssen JG, Numan SC, Kalkman CJ, van Dijk D, Dexamethasone for Cardiac Surgery Study Group (2012) Intraoperative high-dose dexamethasone for cardiac surgery: a randomized controlled trial. JAMA 308:1761–1767
Jacob KA, Leaf DE, Dieleman JM, van Dijk D, Nierich AP, Rosseel PM, van der Maaten JM, Hofland J, Diephuis JC, de Lange F, Boer C, Kluin J, Waikar SS, Dexamethasone for Cardiac Surgery Study Group (2015) Intraoperative high-dose dexamethasone and severe AKI after cardiac surgery. J Am Soc Nephrol 26:2947–2951
Whitlock RP, Devereaux PJ, Teoh KH, Lamy A, Vincent J, Pogue J, Paparella D, Sessler DI, Karthikeyan G, Villar JC, Zuo Y, Avezum A, Quantz M, Tagarakis GI, Shah PJ, Abbasi SH, Zheng H, Pettit S, Chrolavicius S, Yusuf S (2015) Methylprednisolone in patients undergoing cardiopulmonary bypass (SIRS): a randomised, double-blind, placebo-controlled trial. Lancet 386:1243–1253
Song YR, Lee T, You SJ, Chin HJ, Chae DW, Lim C, Park KH, Han S, Kim JH, Na KY (2009) Prevention of acute kidney injury by erythropoietin in patients undergoing coronary artery bypass grafting: a pilot study. Am J Nephrol 30:253–260
de Seigneux S, Ponte B, Weiss L, Pugin J, Romand JA, Martin PY, Saudan P (2012) Epoetin administrated after cardiac surgery: effects on renal function and inflammation in a randomized controlled study. BMC Nephrol 13:132
Yoo YC, Shim JK, Kim JC, Jo YY, Lee JH, Kwak YL (2011) Effect of single recombinant human erythropoietin injection on transfusion requirements in preoperatively anemic patients undergoing valvular heart surgery. Anesthesiology 115:929–937
Kim JH, Shim JK, Song JW, Song Y, Kim HB, Kwak YL (2013) Effect of erythropoietin on the incidence of acute kidney injury following complex valvular heart surgery: a double blind, randomized clinical trial of efficacy and safety. Crit Care 17:R254
Tasanarong A, Duangchana S, Sumransurp S, Homvises B, Satdhabudha O (2013) Prophylaxis with erythropoietin versus placebo reduces acute kidney injury and neutrophil gelatinase-associated lipocalin in patients undergoing cardiac surgery: a randomized, double-blind controlled trial. BMC Nephrol 14:136
Tie HT, Luo MZ, Lin D, Zhang M, Wan JY, Wu QC (2015) Erythropoietin administration for prevention of cardiac surgery-associated acute kidney injury: a meta-analysis of randomized controlled trials. Eur J Cardiothorac Surg 48:32–39
Penny-Dimri JC, Cochrane AD, Perry LA, Smith JA (2016) Characterising the role of perioperative erythropoietin for preventing acute kidney injury after cardiac surgery: systematic review and meta-analysis. Heart Lung Circ 25:1067–1076
Dardashti A, Ederoth P, Algotsson L, Bronden B, Grins E, Larsson M, Nozohoor S, Zinko G, Bjursten H (2014) Erythropoietin and protection of renal function in cardiac surgery (the EPRICS Trial). Anesthesiology 121:582–590
Endre ZH, Walker RJ, Pickering JW, Shaw GM, Frampton CM, Henderson SJ, Hutchison R, Mehrtens JE, Robinson JM, Schollum JB, Westhuyzen J, Celi LA, McGinley RJ, Campbell IJ, George PM (2010) Early intervention with erythropoietin does not affect the outcome of acute kidney injury (the EARLYARF trial). Kidney Int 77:1020–1030
Corwin HL, Gettinger A, Pearl RG, Fink MP, Levy MM, Shapiro MJ, Corwin MJ, Colton T, EPO Critical Care Trials Group (2002) Efficacy of recombinant human erythropoietin in critically ill patients: a randomized controlled trial. JAMA 288:2827–2835
Zhao C, Lin Z, Luo Q, Xia X, Yu X, Huang F (2015) Efficacy and safety of erythropoietin to prevent acute kidney injury in patients with critical illness or perioperative care: a systematic review and meta-analysis of randomized controlled trials. J Cardiovasc Pharmacol 65:593–600
Kim JE, Song SW, Kim JY, Lee HJ, Chung KH, Shim YH (2016) Effect of a single bolus of erythropoietin on renoprotection in patients undergoing thoracic aortic surgery with moderate hypothermic circulatory arrest. Ann Thorac Surg 101:690–696
Shema-Didi L, Kristal B, Eizenberg S, Marzuq N, Sussan M, Feldman-Idov Y, Ofir P, Atar S (2016) Prevention of contrast-induced nephropathy with single bolus erythropoietin in patients with diabetic kidney disease: a randomized controlled trial. Nephrology (Carlton) 21:295–300
Pons M, Plante I, LeBrun M, Gourde P, Simard M, Grenier L, Thibault L, Labrecque G, Beauchamp D (2003) Protein-rich diet attenuates cyclosporin a-induced renal tubular damage in rats. J Ren Nutr 13:84–92
Roberts PR, Black KW, Zaloga GP (1997) Enteral feeding improves outcome and protects against glycerol-induced acute renal failure in the rat. Am J Respir Crit Care Med 156:1265–1269
Mouser JF, Hak EB, Kuhl DA, Dickerson RN, Gaber LW, Hak LJ (1997) Recovery from ischemic acute renal failure is improved with enteral compared with parenteral nutrition. Crit Care Med 25:1748–1754
Zager RA (1987) Amino acid hyperalimentation in acute renal failure: a potential therapeutic paradox. Kidney Int Suppl 22:S72–S75
Heyland DK, Elke G, Cook D, Berger MM, Wischmeyer PE, Albert M, Muscedere J, Jones G, Day AG (2015) Glutamine and antioxidants in the critically ill patient: a post hoc analysis of a large-scale randomized trial. JPEN J Parenter Enteral Nutr 39:401–409
Mitchell JR, Verweij M, Brand K, van de Ven M, Goemaere N, van den Engel S, Chu T, Forrer F, Muller C, de Jong M, van IJcken W, IJzermans JN, Hoeijmakers JH, de Bruin RW (2010) Short-term dietary restriction and fasting precondition against ischemia reperfusion injury in mice. Aging Cell 9:40–53
Abel RM, Beck CH Jr, Abbott WM, Ryan JA Jr, Barnett GO, Fischer JE (1973) Improved survival from acute renal failure after treatment with intravenous essential l-amino acids and glucose. Results of a prospective, double-blind study. N Engl J Med 288:695–699
Doig GS, Simpson F, Bellomo R, Heighes PT, Sweetman EA, Chesher D, Pollock C, Davies A, Botha J, Harrigan P, Reade MC (2015) Intravenous amino acid therapy for kidney function in critically ill patients: a randomized controlled trial. Intensive Care Med 41:1197–1208
Gunst J, Vanhorebeek I, Casaer MP, Hermans G, Wouters PJ, Dubois J, Claes K, Schetz M, Van den Berghe G (2013) Impact of early parenteral nutrition on metabolism and kidney injury. J Am Soc Nephrol 24:995–1005
Al-Dorzi HM, Albarrak A, Ferwana M, Murad MH, Arabi YM (2016) Lower versus higher dose of enteral caloric intake in adult critically ill patients: a systematic review and meta-analysis. Crit Care 20:358
Gonzales DA, Norsworthy KJ, Kern SJ, Banks S, Sieving PC, Star RA, Natanson C, Danner RL (2007) A meta-analysis of N-acetylcysteine in contrast-induced nephrotoxicity: unsupervised clustering to resolve heterogeneity. BMC Med 5:32
Zagler A, Azadpour M, Mercado C, Hennekens CH (2006) N-acetylcysteine and contrast-induced nephropathy: a meta-analysis of 13 randomized trials. Am Heart J 151:140–145
Duong MH, MacKenzie TA, Malenka DJ (2005) N-acetylcysteine prophylaxis significantly reduces the risk of radiocontrast-induced nephropathy: comprehensive meta-analysis. Catheter Cardiovasc Interv 64:471–479
Pannu N, Manns B, Lee H, Tonelli M (2004) Systematic review of the impact of N-acetylcysteine on contrast nephropathy. Kidney Int 65:1366–1374
Alonso A, Lau J, Jaber BL, Weintraub A, Sarnak MJ (2004) Prevention of radiocontrast nephropathy with N-acetylcysteine in patients with chronic kidney disease: a meta-analysis of randomized, controlled trials. Am J Kidney Dis 43:1–9
Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC (2008) Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med 148:284–294
Zhao SJ, Zhong ZS, Qi GX, Tian W (2016) The efficacy of N-acetylcysteine plus sodium bicarbonate in the prevention of contrast-induced nephropathy after cardiac catheterization and percutaneous coronary intervention: a meta-analysis of randomized controlled trials. Int J Cardiol 221:251–259
Wang N, Qian P, Kumar S, Yan TD, Phan K (2016) The effect of N-acetylcysteine on the incidence of contrast-induced kidney injury: a systematic review and trial sequential analysis. Int J Cardiol 209:319–327
Kang X, Hu DY, Li CB, Ai ZS, Peng A (2015) N-acetylcysteine for the prevention of contrast-induced nephropathy in patients with pre-existing renal insufficiency or diabetes: a systematic review and meta-analysis. Ren Fail 37(10):297–303
Sun Z, Fu Q, Cao L, Jin W, Cheng L, Li Z (2013) Intravenous N-acetylcysteine for prevention of contrast-induced nephropathy: a meta-analysis of randomized, controlled trials. PLoS One 8:e55124
ACT Investigators (2011) Acetylcysteine for prevention of renal outcomes in patients undergoing coronary and peripheral vascular angiography: main results from the randomized Acetylcysteine for Contrast-induced nephropathy Trial (ACT). Circulation 124:1250–1259
Burns KE, Chu MW, Novick RJ, Fox SA, Gallo K, Martin CM, Stitt LW, Heidenheim AP, Myers ML, Moist L (2005) Perioperative N-acetylcysteine to prevent renal dysfunction in high-risk patients undergoing CABG surgery: a randomized controlled trial. JAMA 294:342–350
Macedo E, Abdulkader R, Castro I, Sobrinho AC, Yu L, Vieira JM Jr (2006) Lack of protection of N-acetylcysteine (NAC) in acute renal failure related to elective aortic aneurysm repair-a randomized controlled trial. Nephrol Dial Transplant 21:1863–1869
Komisarof JA, Gilkey GM, Peters DM, Koudelka CW, Meyer MM, Smith SM (2007) N-acetylcysteine for patients with prolonged hypotension as prophylaxis for acute renal failure (NEPHRON). Crit Care Med 35:435–441
Sisillo E, Ceriani R, Bortone F, Juliano G, Salvi L, Veglia F, Fiorentini C, Marenzi G (2008) N-acetylcysteine for prevention of acute renal failure in patients with chronic renal insufficiency undergoing cardiac surgery: a prospective, randomized, clinical trial. Crit Care Med 36:81–86
Adabag AS, Ishani A, Koneswaran S, Johnson DJ, Kelly RF, Ward HB, McFalls EO, Bloomfield HE, Chandrashekhar Y (2008) Utility of N-acetylcysteine to prevent acute kidney injury after cardiac surgery: a randomized controlled trial. Am Heart J 155:1143–1149
Song JW, Shim JK, Soh S, Jang J, Kwak YL (2015) Double-blinded, randomized controlled trial of N-acetylcysteine for prevention of acute kidney injury in high risk patients undergoing off-pump coronary artery bypass. Nephrology (Carlton) 20:96–102
Wijeysundera DN, Beattie WS, Rao V, Granton JT, Chan CT (2007) N-acetylcysteine for preventing acute kidney injury in cardiac surgery patients with pre-existing moderate renal insufficiency. Can J Anaesth 54:872–881
Sandilands EA, Bateman DN (2009) Adverse reactions associated with acetylcysteine. Clin Toxicol (Phila) 47:81–88
Molnar Z, Shearer E, Lowe D (1999) N-Acetylcysteine treatment to prevent the progression of multisystem organ failure: a prospective, randomized, placebo-controlled study. Crit Care Med 27:1100–1104
Peake SL, Moran JL, Leppard PI (1996) N-acetyl-l-cysteine depresses cardiac performance in patients with septic shock. Crit Care Med 24:1302–1310
Angstwurm MW, Schottdorf J, Schopohl J, Gaertner R (1999) Selenium replacement in patients with severe systemic inflammatory response syndrome improves clinical outcome. Crit Care Med 27:1807–1813
Mishra V, Baines M, Perry SE, McLaughlin PJ, Carson J, Wenstone R, Shenkin A (2007) Effect of selenium supplementation on biochemical markers and outcome in critically ill patients. Clin Nutr 26:41–50
Angstwurm MW, Engelmann L, Zimmermann T, Lehmann C, Spes CH, Abel P, Strauss R, Meier-Hellmann A, Insel R, Radke J, Schuttler J, Gartner R (2007) Selenium in Intensive Care (SIC): results of a prospective randomized, placebo-controlled, multiple-center study in patients with severe systemic inflammatory response syndrome, sepsis, and septic shock. Crit Care Med 35:118–126
Bloos F, Trips E, Nierhaus A, Briegel J, Heyland DK, Jaschinski U, Moerer O, Weyland A, Marx G, Grundling M, Kluge S, Kaufmann I, Ott K, Quintel M, Jelschen F, Meybohm P, Rademacher S, Meier-Hellmann A, Utzolino S, Kaisers UX, Putensen C, Elke G, Ragaller M, Gerlach H, Ludewig K, Kiehntopf M, Bogatsch H, Engel C, Brunkhorst FM, Loeffler M, Reinhart K, for SepNet Critical Care Trials G (2016) Effect of sodium selenite administration and procalcitonin-guided therapy on mortality in patients with severe sepsis or septic shock: a randomized clinical trial. JAMA intern med 176: 1266-1276
Kavalipati N, Shah J, Ramakrishan A, Vasnawala H (2015) Pleiotropic effects of statins. Indian J Endocrinol Metab 19:554–562
Han Y, Zhu G, Han L, Hou F, Huang W, Liu H, Gan J, Jiang T, Li X, Wang W, Ding S, Jia S, Shen W, Wang D, Sun L, Qiu J, Wang X, Li Y, Deng J, Li J, Xu K, Xu B, Mehran R, Huo Y (2014) Short-term rosuvastatin therapy for prevention of contrast-induced acute kidney injury in patients with diabetes and chronic kidney disease. J Am Coll Cardiol 63:62–70
Leoncini M, Toso A, Maioli M, Tropeano F, Villani S, Bellandi F (2014) Early high-dose rosuvastatin for contrast-induced nephropathy prevention in acute coronary syndrome: results from the PRATO-ACS Study (Protective EFFECT of Rosuvastatin and Antiplatelet Therapy On contrast-induced acute kidney injury and myocardial damage in patients with Acute Coronary Syndrome). J Am Coll Cardiol 63:71–79
Quintavalle C, Fiore D, De Micco F, Visconti G, Focaccio A, Golia B, Ricciardelli B, Donnarumma E, Bianco A, Zabatta MA, Troncone G, Colombo A, Briguori C, Condorelli G (2012) Impact of a high loading dose of atorvastatin on contrast-induced acute kidney injury. Circulation 126:3008–3016
Shehata M, Hamza M (2015) Impact of high loading dose of atorvastatin in diabetic patients with renal dysfunction undergoing elective percutaneous coronary intervention: a randomized controlled trial. Cardiovasc Ther 33:35–41
Li J, Li Y, Xu B, Jia G, Guo T, Wang D, Xu K, Deng J, Han Y (2016) Short-term rosuvastatin therapy prevents contrast-induced acute kidney injury in female patients with diabetes and chronic kidney disease: a subgroup analysis of the TRACK-D study. J Thorac Dis 8:1000–1006
Barbieri L, Verdoia M, Schaffer A, Nardin M, Marino P, De Luca G (2014) The role of statins in the prevention of contrast induced nephropathy: a meta-analysis of 8 randomized trials. J Thromb Thrombolysis 38:493–502
Lee JM, Park J, Jeon KH, Jung JH, Lee SE, Han JK, Kim HL, Yang HM, Park KW, Kang HJ, Koo BK, Jo SH, Kim HS (2014) Efficacy of short-term high-dose statin pretreatment in prevention of contrast-induced acute kidney injury: updated study-level meta-analysis of 13 randomized controlled trials. PLoS One 9:e111397
Ukaigwe A, Karmacharya P, Mahmood M, Pathak R, Aryal MR, Jalota L, Donato AA (2014) Meta-analysis on efficacy of statins for prevention of contrast-induced acute kidney injury in patients undergoing coronary angiography. Am J Cardiol 114:1295–1302
Singh N, Lee JZ, Huang JJ, Low SW, Howe C, Pandit A, Suryanarayana P, Lee KS (2014) Benefit of statin pretreatment in prevention of contrast-induced nephropathy in different adult patient population: systematic review and meta-analysis. Open Heart 1:e000127
Marenzi G, Cosentino N, Werba JP, Tedesco CC, Veglia F, Bartorelli AL (2015) A meta-analysis of randomized controlled trials on statins for the prevention of contrast-induced acute kidney injury in patients with and without acute coronary syndromes. Int J Cardiol 183:47–53
Liakopoulos OJ, Choi YH, Haldenwang PL, Strauch J, Wittwer T, Dorge H, Stamm C, Wassmer G, Wahlers T (2008) Impact of preoperative statin therapy on adverse postoperative outcomes in patients undergoing cardiac surgery: a meta-analysis of over 30,000 patients. Eur Heart J 29:1548–1559
Wang J, Gu C, Gao M, Yu W, Yu Y (2015) Preoperative statin therapy and renal outcomes after cardiac surgery: a meta-analysis and meta-regression of 59,771 patients. Can J Cardiol 31:1051–1060
Lewicki M, Ng I, Schneider AG (2015) HMG CoA reductase inhibitors (statins) for preventing acute kidney injury after surgical procedures requiring cardiac bypass. Cochrane Database Syst Rev 3:CD010480
Billings FT, Hendricks PA, Schildcrout JS, Shi Y, Petracek MR, Byrne JG, Brown NJ (2016) High-dose perioperative atorvastatin and acute kidney injury following cardiac surgery: a randomized clinical trial. JAMA 315:877–888
Park JH, Shim JK, Song JW, Soh S, Kwak YL (2016) Effect of atorvastatin on the incidence of acute kidney injury following valvular heart surgery: a randomized, placebo-controlled trial. Intensive Care Med 42:1398–1407
Zheng Z, Jayaram R, Jiang L, Emberson J, Zhao Y, Li Q, Du J, Guarguagli S, Hill M, Chen Z, Collins R, Casadei B (2016) Perioperative rosuvastatin in cardiac surgery. N Engl J Med 374:1744–1753
Zarbock A, Schmidt C, Van Aken H, Wempe C, Martens S, Zahn PK, Wolf B, Goebel U, Schwer CI, Rosenberger P, Haeberle H, Gorlich D, Kellum JA, Meersch M, Renal RI (2015) Effect of remote ischemic preconditioning on kidney injury among high-risk patients undergoing cardiac surgery: a randomized clinical trial. JAMA 313:2133–2141
Zimmerman RF, Ezeanuna PU, Kane JC, Cleland CD, Kempananjappa TJ, Lucas FL, Kramer RS (2011) Ischemic preconditioning at a remote site prevents acute kidney injury in patients following cardiac surgery. Kidney Int 80:861–867
Kim TK, Min JJ, Cho YJ, Hausenloy DJ, Ahn H, Kim KH, Hwang HY, Hong DM, Jeon Y (2017) Effects of delayed remote ischemic preconditioning on peri-operative myocardial injury in patients undergoing cardiac surgery—a randomized controlled trial. Int J Cardiol 227:511–515
Meybohm P, Bein B, Brosteanu O, Cremer J, Gruenewald M, Stoppe C, Coburn M, Schaelte G, Boning A, Niemann B, Roesner J, Kletzin F, Strouhal U, Reyher C, Laufenberg-Feldmann R, Ferner M, Brandes IF, Bauer M, Stehr SN, Kortgen A, Wittmann M, Baumgarten G, Meyer-Treschan T, Kienbaum P, Heringlake M, Schon J, Sander M, Treskatsch S, Smul T, Wolwender E, Schilling T, Fuernau G, Hasenclever D, Zacharowski K (2015) A multicenter trial of remote ischemic preconditioning for heart surgery. N Engl J Med 373:1397–1407
Hong DM, Lee EH, Kim HJ, Min JJ, Chin JH, Choi DK, Bahk JH, Sim JY, Choi IC, Jeon Y (2014) Does remote ischaemic preconditioning with postconditioning improve clinical outcomes of patients undergoing cardiac surgery? Remote Ischaemic Preconditioning with Postconditioning Outcome Trial. Eur Heart J 35:176–183
Hausenloy DJ, Candilio L, Evans R, Ariti C, Jenkins DP, Kolvekar S, Knight R, Kunst G, Laing C, Nicholas J, Pepper J, Robertson S, Xenou M, Clayton T, Yellon DM, ERICCA Trial Investigators (2015) Remote ischemic preconditioning and outcomes of cardiac surgery. N Engl J Med 373:1408–1417
Walsh M, Whitlock R, Garg AX, Legare JF, Duncan AE, Zimmerman R, Miller S, Fremes S, Kieser T, Karthikeyan G, Chan M, Ho A, Nasr V, Vincent J, Ali I, Lavi R, Sessler DI, Kramer R, Gardner J, Syed S, VanHelder T, Guyatt G, Rao-Melacini P, Thabane L, Devereaux PJ, Remote IMPACT Investigators (2016) Effects of remote ischemic preconditioning in high-risk patients undergoing cardiac surgery (Remote IMPACT): a randomized controlled trial. CMAJ 188:329–336
Zhang L, Diao Y, Chen G, Tanaka A, Eastwood GM, Bellomo R (2016) Remote ischemic conditioning for kidney protection: a meta-analysis. J Crit Care 33:224–232
Zhou C, Jeon Y, Meybohm P, Zarbock A, Young PJ, Li L, Hausenloy DJ (2016) Renoprotection by remote ischemic conditioning during elective coronary revascularization: a systematic review and meta-analysis of randomized controlled trials. Int J Cardiol 222:295–302
Yang Y, Lang XB, Zhang P, Lv R, Wang YF, Chen JH (2014) Remote ischemic preconditioning for prevention of acute kidney injury: a meta-analysis of randomized controlled trials. Am J Kidney Dis 64:574–583
Li B, Lang X, Cao L, Wang Y, Lu Y, Feng S, Yang Y, Chen J, Jiang H (2017) Effect of remote ischemic preconditioning on postoperative acute kidney injury among patients undergoing cardiac and vascular interventions: a meta-analysis. J Nephrol 30:19–33
Hu J, Liu S, Jia P, Xu X, Song N, Zhang T, Chen R, Ding X (2016) Protection of remote ischemic preconditioning against acute kidney injury: a systematic review and meta-analysis. Crit Care 20:111
Pierce B, Bole I, Patel V, Brown DL (2017) Clinical outcomes of remote ischemic preconditioning prior to cardiac surgery: a meta-analysis of randomized controlled trials. J Am Heart Assoc. doi:10.1161/JAHA.116.004666
Yi B, Chen X, Shi H, Lin T, Lin H, Xu Y, Rong J (2017) Remote ischaemic preconditioning reduces acute kidney injury in adult patients undergoing cardiac surgery with cardiopulmonary bypass: a meta-analysis. Eur J Cardiothorac Surg 51:616–623
Zhou C, Bulluck H, Fang N, Li L, Hausenloy DJ (2017) Age and surgical complexity impact on renoprotection by remote ischemic preconditioning during adult cardiac surgery: a meta analysis. Scientific reports 7:215
Zhang Y, Zhang X, Chi D, Wang S, Wei H, Yu H, Li Q, Liu B (2016) Remote ischemic preconditioning for prevention of acute kidney injury in patients undergoing on-pump cardiac surgery: a systematic review and meta-analysis. Medicine 95:e3465
Pei H, Wu Y, Wei Y, Yang Y, Teng S, Zhang H (2014) Remote ischemic preconditioning reduces perioperative cardiac and renal events in patients undergoing elective coronary intervention: a meta-analysis of 11 randomized trials. PLoS One 9:e115500
Li L, Li G, Yu C, Li Y (2013) The role of remote ischemic preconditioning on postoperative kidney injury in patients undergoing cardiac and vascular interventions: a meta-analysis. J Cardiothorac Surg 8:43
Sukkar L, Hong D, Wong MG, Badve SV, Rogers K, Perkovic V, Walsh M, Yu X, Hillis GS, Gallagher M, Jardine M (2016) Effects of ischaemic conditioning on major clinical outcomes in people undergoing invasive procedures: systematic review and meta-analysis. BMJ 355:i5599
Zhou CC, Ge YZ, Yao WT, Wu R, Xin H, Lu TZ, Li MH, Song KW, Wang M, Zhu YP, Zhu M, Geng LG, Gao XF, Zhou LH, Zhang SL, Zhu JG, Jia RP (2017) Limited clinical utility of remote ischemic conditioning in renal transplantation: a meta-analysis of randomized controlled trials. PLoS One 12:e0170729
Kolhe NV, Reilly T, Leung J, Fluck RJ, Swinscoe KE, Selby NM, Taal MW (2016) A simple care bundle for use in acute kidney injury: a propensity score-matched cohort study. Nephrol Dial Transplant 31:1846–1854
Joslin J, Wilson H, Zubli D, Gauge N, Kinirons M, Hopper A, Pile T, Ostermann M (2015) Recognition and management of acute kidney injury in hospitalised patients can be partially improved with the use of a care bundle. Clinic Med (Lond) 15:431–436
Bhagwanani A, Carpenter R, Yusuf A (2014) Improving the management of acute kidney injury in a district general hospital: introduction of the DONUT bundle. BMJ Qual Improv Rep. doi:10.1136/bmjquality.u202650.w1235
Meersch M, Schmidt C, Hoffmeier A, Van Aken H, Wempe C, Gerss J, Zarbock A (2017) Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med. doi:10.1007/s00134-016-4670-3
Angus DC, Barnato AE, Bell D, Bellomo R, Chong CR, Coats TJ, Davies A, Delaney A, Harrison DA, Holdgate A, Howe B, Huang DT, Iwashyna T, Kellum JA, Peake SL, Pike F, Reade MC, Rowan KM, Singer M, Webb SA, Weissfeld LA, Yealy DM, Young JD (2015) A systematic review and meta-analysis of early goal-directed therapy for septic shock: the ARISE, ProCESS and ProMISe investigators. Intensive Care Med 41:1549–1560
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8:R204–R212
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A (2007) Acute Kidney Injury Network (AKIN): report of an initiative to improve outcomes in acute kidney injury. Crit Care 11:R31
Acknowlegements
Open access funding provided by University of Innsbruck and Medical University of Innsbruck.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
MJ has received honoraria or research support from Baxter Healthcare Corp, AM-Pharma, CLS Behring, Fresenius and Astute Medical. WD declares no conflicts of interest. LF has received honoraria and research support from Astute Medical, Fresenius, Baxter Gambro Renal and Orthoclinical Diagnostics. PH had received research grants from Baxter, AM Pharma, Bellco, and Pfizer EH received speaker’s fees from Alexion and Astute Medical, and a research grant from Bellco. MO has received honoraria and research funding from Fresenius Medical Care and Baxter Gambro. HO has financial congress support from Dirinco (Netherlands) and speaker’s honoraria from Fresenius and Gambro/Baxter. MS declares no conflicts of interest.
Additional information
Professor Groeneveld succumbed to a long illness which he fought with typical determination during the updating of this paper. He is sadly missed by us all.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Joannidis, M., Druml, W., Forni, L.G. et al. Prevention of acute kidney injury and protection of renal function in the intensive care unit: update 2017. Intensive Care Med 43, 730–749 (2017). https://doi.org/10.1007/s00134-017-4832-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-017-4832-y