Abstract
Background
Prone position ventilation for acute hypoxemic respiratory failure (AHRF) improves oxygenation but not survival, except possibly when AHRF is severe.
Objective
To determine effects of prone versus supine ventilation in AHRF and severe hypoxemia [partial pressure of arterial oxygen (PaO2)/inspired fraction of oxygen (FiO2) <100 mmHg] compared with moderate hypoxemia (100 mmHg ≤ PaO2/FiO2 ≤ 300 mmHg).
Design
Systematic review and meta-analysis.
Data Sources
Electronic databases (to November 2009) and conference proceedings.
Methods
Two authors independently selected and extracted data from parallel-group randomized controlled trials comparing prone with supine ventilation in mechanically ventilated adults or children with AHRF. Trialists provided subgroup data. The primary outcome was hospital mortality in patients with AHRF and PaO2/FiO2 <100 mmHg. Meta-analyses used study-level random-effects models.
Results
Ten trials (N = 1,867 patients) met inclusion criteria; most patients had acute lung injury. Methodological quality was relatively high. Prone ventilation reduced mortality in patients with PaO2/FiO2 <100 mmHg [risk ratio (RR) 0.84, 95% confidence interval (CI) 0.74–0.96; p = 0.01; seven trials, N = 555] but not in patients with PaO2/FiO2 ≥100 mmHg (RR 1.07, 95% CI 0.93–1.22; p = 0.36; seven trials, N = 1,169). Risk ratios differed significantly between subgroups (interaction p = 0.012). Post hoc analysis demonstrated statistically significant improved mortality in the more hypoxemic subgroup and significant differences between subgroups using a range of PaO2/FiO2 thresholds up to approximately 140 mmHg. Prone ventilation improved oxygenation by 27–39% over the first 3 days of therapy but increased the risks of pressure ulcers (RR 1.29, 95% CI 1.16–1.44), endotracheal tube obstruction (RR 1.58, 95% CI 1.24–2.01), and chest tube dislodgement (RR 3.14, 95% CI 1.02–9.69). There was no statistical between-trial heterogeneity for most clinical outcomes.
Conclusions
Prone ventilation reduces mortality in patients with severe hypoxemia. Given associated risks, this approach should not be routine in all patients with AHRF, but may be considered for severely hypoxemic patients.
Similar content being viewed by others
Introduction
Acute lung injury (ALI) and the more hypoxemic subgroup of acute respiratory distress syndrome (ARDS) may occur after many primary or secondary pulmonary injuries, leading to a common syndrome characterized by hypoxemia, pulmonary congestion, and decreased pulmonary compliance. This syndrome is associated with substantial mortality [1, 2], morbidity [3, 4], and costs [5]. Mechanical ventilation usually corrects tissue hypoxemia [6] but also may be complicated by ventilator-induced lung injury. Although lower tidal volume [7] reduces ventilator-induced lung injury, mortality in patients with ARDS remains high [1, 2].
Mechanical ventilation of patients with ALI in the prone position, first suggested in 1974 [8], optimizes both lung recruitment and ventilation–perfusion matching [9]. Collapse due to gravity of ventral lung segments in the prone position is less than that of dorsal lung segments in the supine position [10, 11], while lung perfusion in the prone position is more evenly distributed [12]. Other potentially important improvements include enhanced postural drainage of secretions [13] and decreased alveolar overdistension [14], cyclic alveolar collapse, and ventilator-induced lung injury [15].
Multicenter randomized trials [16–18] and systematic reviews [19–23] have failed to demonstrate that prone ventilation improves overall mortality in patients with acute hypoxemic respiratory failure, despite the strong physiological rationale. Subgroup analyses have suggested a mortality benefit in patients with severe hypoxemia [16] or with higher severity of illness [16, 21, 22]. However, these analyses are limited by reporting bias due to lack of subgroup data from most trials [21, 22], limited numbers of patients and events [16, 21, 22], and omission of appropriate statistical tests to detect subgroup differences [24].
The objective of this systematic review, performed in collaboration with prone ventilation trialists, was to determine whether prone ventilation reduces mortality compared with supine ventilation in patients with acute hypoxemic respiratory failure and severe hypoxemia. We reasoned that patients with severe hypoxemia would be the most likely to benefit from prone ventilation because the main effect of prone ventilation is to improve oxygenation [19], and clinicians use this technique primarily for refractory hypoxemia [25]. Furthermore, the proposed protective effects of prone ventilation occur due to lung recruitment, and patients with more severe hypoxia have more recruitable lung [26]. A priori, we hypothesized that prone ventilation would reduce mortality in severely hypoxemic patients, defined by baseline ratio of partial pressure of arterial oxygen (PaO2) to inspired fraction of oxygen (FiO2) <100 mmHg, but not in patients with moderate hypoxemia (100 mmHg ≤ PaO2/FiO2 ≤ 300 mmHg). We chose a threshold PaO2/FiO2 of 100 mmHg to identify severe hypoxemia because this value was used to stratify patients in the most recent randomized controlled trial (RCT) of prone ventilation [27] and because bedside clinicians can readily determine whether a patient’s PaO2/FiO2 is above or below this threshold.
Methods
Study identification
We updated our previous search [19] using systematic methods (Appendix) to identify RCTs of mechanical ventilation in the prone compared with supine position in patients with ALI, ARDS, and acute hypoxemic respiratory failure [28]. We identified all relevant trials using the following techniques: electronic searches of MEDLINE, EMBASE, and CENTRAL (from inception to November 2009); manual searches of reference lists from included studies and review articles; manual and electronic searches of conference proceedings of the American Thoracic Society (1994–2009), Society of Critical Care Medicine (1994–2009), European Society of Intensive Care Medicine (1994–2009), American College of Chest Physicians (1994–2009), and the International Symposium on Intensive Care and Emergency Medicine (1997–2009); and contact with primary investigators. Finally, we searched for unpublished and ongoing trials in clinicaltrials.gov and controlled-trials.com [29]. No language restrictions were applied [30].
Study eligibility
Two investigators independently evaluated retrieved studies for possible inclusion and resolved differences by consensus [31]. We included studies if they (1) enrolled mechanically ventilated adults or postneonatal children with acute hypoxemic respiratory failure (defined by PaO2/FiO2 ≤300 mmHg); (2) randomly assigned patients to two or more groups, including a treatment group ventilated at least once in the prone position and a control group ventilated in the supine position, with an intervention period of at least 48 h in duration; and (3) reported any of our primary or secondary outcomes (see below).
Trials allocating patients in alternating fashion or by hospital registry number (quasirandomization) or trials with co-interventions (such as high-frequency oscillation or nitric oxide) specified as part of the intervention and applied equally to both groups were also eligible. We excluded randomized crossover trials in which patients received both treatment and control interventions in random order. We also excluded short-term trials in which the intervention was applied for ≤48 h, because we believed that outcomes would be minimally affected by applying the intervention for such a short duration.
We included trials in which prone positioning was used early (within 72 h after initiation of mechanical ventilation for acute hypoxemic respiratory failure) and as late or rescue therapy (72 h after initiation of mechanical ventilation), and trials in which prone ventilation was applied intermittently (for a predefined period of time each day) or continuously (without interruption for the duration of the study period).
Data extraction and study quality
Two reviewers independently abstracted data on study methods, details of prone ventilation (including duration of prone ventilation per day and total duration of the intervention period) and general mechanical ventilation, and study outcomes. Disagreements were resolved by consensus.
We abstracted data on: method of randomization and allocation concealment, number of postrandomization withdrawals and losses to follow-up, and crossovers between assigned groups [32]. Allocation concealment was assessed according to the criteria of the Cochrane Collaboration [33]. We also determined whether studies were stopped early for benefit [34] or for other reasons such as harm or futility. Since blinding of caregivers, patients, and family members is impossible in a trial evaluating prone ventilation, we determined whether outcome assessors were blinded to the diagnosis of ventilator-associated pneumonia (VAP) and whether important co-interventions such as weaning, sedation and paralysis, steroids, and use of rescue therapies for hypoxemia (inhaled nitric oxide, high-frequency oscillation, extracorporeal oxygenation) were standardized or equally applied in treatment and control groups.
The authors of included trials collaborated in this systematic review by reviewing original trial data, providing previously unpublished data for subgroups of patients, and clarifying data and methods.
Outcomes
The primary outcome was mortality in the subgroup of patients with severe acute hypoxemic respiratory failure, defined by baseline PaO2/FiO2 <100 mmHg, compared with mortality in patients with 100 mmHg ≤ PaO2/FiO2 ≤ 300 mmHg. For each study, mortality was determined at hospital discharge or, if not available, at the longest duration of follow-up. Secondary outcomes included mortality stratified according to the same threshold PaO2/FiO2 but limited to patients with ALI/ARDS; and in all patients, duration of mechanical ventilation, ventilator-free days to day 28, and adverse events (VAP, pressure ulcers, endotracheal tube obstruction, unplanned extubation, unplanned removal of central venous catheters or arterial lines, unplanned removal of chest tubes, pneumothoraces, and cardiac arrests). We also considered the effect on PaO2/FiO2 ratio on the first, second, and third calendar day after randomization in all patients. We measured the oxygenation effect of prone positioning by comparing the mean PaO2/FiO2 ratio measured in the prone group with the closest available recorded measurement in the supine group. Where more than one measurement was taken we chose the measurement closest to the end of the proning session on that day.
We analyzed patients according to assigned group for all outcomes.
Statistical analysis
We aggregated outcome data at the trial level and performed statistical calculations with Review Manager (RevMan) 5.0 (2009; The Cochrane Collaboration, Oxford, UK) and STATA 9.2 (2006; StataCorp, TX, USA) using random-effects models. Random-effects models incorporate both within-study and between-study variation and provide more conservative treatment estimates when heterogeneity is present. We reported continuous outcomes using mean differences (a measure of absolute change) and ratios of means (a measure of relative change [35]), and binary outcomes as risk ratios (RR). For the primary outcome, we performed a z test of interaction between the RR for mortality in the subgroup of patients with PaO2/FiO2 <100 mmHg and the RR in the subgroup of patients with PaO2/FiO2 ≥100 mmHg, which tests the null hypothesis that the treatment effect in each subgroup is the same. In a post hoc analysis, we conducted similar comparisons of the more versus less hypoxemic subgroups using PaO2/FiO2 thresholds ranging from 80 to 200 mmHg, in increments of 10 mmHg. All statistical tests were two sided. We considered p < 0.05 as statistically significant in all analyses and report individual trial and summary results with 95% confidence intervals (CIs).
We assessed between-study heterogeneity for each outcome using the I 2 measure [36, 37]. We considered statistical heterogeneity to be low for I 2 = 25–49%, moderate for I 2 = 50–74%, and high for I 2 ≥ 75% [37].
To assess publication bias we examined funnel plots of treatment effect versus study precision and assessed statistically using Begg’s rank correlation test [38] and modified Macaskill’s regression test [39]. Given the low power of these tests, we assumed a more liberal level of significance (p < 0.10) to indicate publication bias.
Results
Literature search
We identified 2,683 citations from searches of electronic bibliographic databases and 18 citations from other sources. We retrieved 52 records for detailed evaluation, of which 10 trials [16–18, 27, 40–45] met criteria for inclusion in our review (Fig. 1). One study [40] was verified to be randomized after contacting authors [46, 47]. We identified eight publications [46–53] whose authors provided duplicate or supplementary data. We excluded five trials [54–58] in which the intervention period was less than 48 h and identified one ongoing study that would meet inclusion criteria [59]. Reviewers had perfect agreement for study inclusion. The largest trial (n = 802) [17] enrolled patients with acute hypoxemic respiratory failure (PaO2/FiO2 ≤300 mmHg), including ALI/ARDS (n = 413). One other trial [45] enrolled patients requiring mechanical ventilation with Glasgow coma score ≤9, for which we included only patients with PaO2/FiO2 ≤300 mmHg at baseline. All other trials reporting mortality enrolled exclusively patients with ALI/ARDS.
Study characteristics and methodological quality
The ten included trials (Table 1) [16–18, 27, 40–45] enrolled 1,867 patients (median 77 per trial, range 16–802). One trial (n = 102) enrolled children [41]. Most trials enrolled patients within 72 h after the development of hypoxemic respiratory failure [18, 27, 40–43, 45], but two studies did not limit the duration of acute hypoxemic respiratory failure prior to enrolment [16, 17]. The median PaO2/FiO2 at baseline was 122 (range 100–243) mmHg. Patients in the included trials were ventilated in the prone position for a median of 14 h per day (range 4–24 h), and prone ventilation was continued either for a prespecified duration [40, 44] or until prespecified clinical improvements [16–18, 27, 41–43, 45] (median duration of proning 4.7 days, range 4–10 days).
The included trials had relatively high methodological quality (Table 1). Eight trials concealed allocation [16–18, 27, 41–43, 45], one trial [40] did not conceal allocation [46, 47], and another enrolled alternating patients [44]. All trials analyzed outcomes for patients by assigned group. Seven studies were terminated prematurely after meeting prespecified criteria for futility [41] or because of slow recruitment [16, 18, 40, 42, 43, 45]. For the trials that reported mortality, vital status was known at the end of follow-up for all patients in three trials [40, 41, 43] and losses were less than 5% of those randomized in six trials (12/802 [17], 6/142 [18], 6/344 [27], 2/42 [42], 2/53 [45], 7/304 [16]). Seven trials reported crossovers between groups; these involved <6% of randomized patients for five trials (12/304 [16], 4/102 [41], 5/136 [18], 2/40 [42], 20/342 [27]), and 12% (6/51[45]) and 32% (251/791[17]) in two trials. Five trials mandated low-tidal-volume ventilation (6–8 ml/kg body weight) [27, 40–43], and five trials [18, 27, 40, 41, 43] used mechanical ventilation guidelines or protocols during the study period. Protocols for sedation [18, 41, 42, 44] and for weaning from mechanical ventilation [17, 18, 41, 42] were used in four trials each. Blinded assessment [45] or independent adjudication [17] for VAP was used in two of seven trials that reported this outcome [17, 18, 40, 42–45].
Quantitative data synthesis
Mortality
Seven [16–18, 27, 40–42] of ten trials provided mortality stratified by baseline PaO2/FiO2 and were included in the primary analysis. Two trials [43, 45] could not be included in the analysis because only one patient [43] or no patients [45] had PaO2/FiO2 <100 mmHg, and one trial did not report mortality [44]. The seven trials [16–18, 27, 40–42] in the primary analysis had the lowest baseline PaO2/FiO2 (median 113 mmHg, range 100–152 mmHg), and all but one trial [41] followed patients to hospital discharge [18, 40, 42, 43, 45] or at least 90 days [16, 17, 27]. Prone ventilation significantly reduced all-cause mortality (Fig. 2) in patients with baseline PaO2/FiO2 <100 mmHg (RR 0.84, 95% CI 0.74–0.96; p = 0.01; N = 555) but not in patients with baseline PaO2/FiO2 ≥100 mmHg (RR 1.07, 95% CI 0.93–1.22; p = 0.36; N = 1,169). The test for interaction between these subgroups was statistically significant (p = 0.012), indicating that treatment effects differed significantly in subgroups with severe and moderate baseline hypoxemia.Footnote 1 Considering all patients together, regardless of severity of hypoxemia, there was no effect on mortality (RR 0.97, 95% CI 0.88–1.07; p = 0.54; N = 1,786). In the severely hypoxemic subgroup, the number of patients needed to prone to prevent one death was 11 (95% CI 6–50, calculated from a random-effects risk difference model).
Effect of prone ventilation on mortality (at hospital discharge or longest duration of follow-up). The z test for subgroup interaction was statistically significant (p = 0.012). Trialists verified all overall and subgroup mortality data; overall mortality data differed from the original publication in one case [16]. Patients lost to follow-up were removed from the denominator. Results are unchanged if these patients are retained in the denominator and assumed to be alive at the end of the follow-up period, as done in two trials that followed up patients for 6 months [16, 27]. Baseline PaO2/FiO2 values were unavailable for one patient in the prone group in one trial [40] and one patient in the supine group in another trial [42]. Weight is the contribution of each study to the overall risk ratio. CI confidence interval, I 2 percentage of total variation across studies from between-study heterogeneity rather than chance, n/N = number of deaths/number of patients randomized
Since two trials [17, 45] included patients with acute hypoxemic respiratory failure but without ALI/ARDS, we also analyzed mortality limited to patients with ALI/ARDS. Results were similar, although the interaction p value (0.06) was not statistically significant: RR 0.85, 95% CI 0.74–0.98, p = 0.02 in patients with baseline PaO2/FiO2 <100 mmHg (N = 495), and RR 1.04, 95% CI 0.89–1.22, p = 0.60 in patients with baseline PaO2/FiO2 ≥100 mmHg (N = 852).
We found no evidence of statistical heterogeneity for all mortality analyses (I 2 = 0%). Neither Begg’s rank correlation test (p = 0.52) nor the modified Macaskill’s regression test (p = 0.37) suggested publication bias.
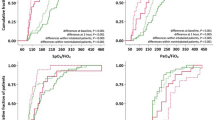
Post hoc analyses using varying PaO2/FiO2 thresholds (Fig. 3) suggested improved mortality in the more severely hypoxemic subgroup using PaO2/FiO2 thresholds up to approximately 140 mmHg to define this subgroup.
Effect of prone ventilation on mortality in severe and moderate baseline hypoxemic subgroups for a range of PaO2/FiO2 threshold values. Error bars indicate width of 95% confidence interval of relative risk in the severe (black squares) and moderate (white squares) baseline hypoxemic subgroups. * Interaction p value <0.05, indicating that treatment effects differed significantly in subgroups with severe and moderate baseline hypoxemia at the PaO2/FiO2 threshold. + Treatment effect p value <0.05, indicating that prone ventilation significantly decreased mortality in the subgroup with severe baseline hypoxemia defined using the PaO2/FiO2 threshold. p-Values were not corrected for multiple comparisons. Trials with no or all patients with events (i.e., risk ratio not calculable) in either the severe or moderate baseline hypoxemia subgroup were excluded from both subgroups at each PaO2/FiO2 threshold. If the data from these trials are included in the subgroup in which the trial has some patients with events, there are no significant changes to the results. CI confidence interval, N number of randomized patients included for each subgroup at the PaO2/FiO2 threshold
Oxygenation and nonmortality clinical endpoints
On days 1–3 after randomization, prone ventilation increased PaO2/FiO2 ratio in seven trials [16, 18, 27, 40–42, 44], by 27–39% (Fig. 4). Prone ventilation also reduced VAP (RR 0.81, 95% CI 0.67–1.00, p = 0.05; eight trials [17, 18, 40, 42–45], N = 1,066). Despite these improvements, there was no effect on duration of mechanical ventilation (mean difference −0.70 days, 95% CI −2.01 to +0.62 days, p = 0.30; eight trials [16, 17, 27, 41–45], N = 1,588) or ventilator-free days to day 28 (mean difference −0.88 days, 95% CI −2.14 to +0.37 days, p = 0.17; five trials [16, 27, 41, 42, 45], N = 771). Statistical heterogeneity was low to moderate for physiologic and clinical endpoints (I 2 = 0–35%).
Effect of prone ventilation on PaO2 (partial pressure of arterial oxygen)/FiO2 (inspired fraction of oxygen) on postrandomization calendar days 1–3. Ratio of means = mean PaO2/FiO2 in the prone group (in the prone position)/mean PaO2/FiO2 in the supine group (at the closest available time). Weight is the contribution of each study to the overall ratio of means. CI confidence interval, I 2 percentage of total variation across studies due to between-study heterogeneity rather than chance
Adverse events (Table 2)
Prone positioning increased the risk of pressure ulcers (RR 1.29, 95% CI 1.16–1.44, p < 0.00001; seven trials [16, 18, 40, 41, 43, 45], N = 1,279), endotracheal tube obstruction (RR 1.58, 95% CI 1.24–2.01, p = 0.0002; seven trials [17, 27, 41–45], N = 1,351), and inadvertent chest tube removal (RR 3.14, 95% CI 1.02–9.69, p = 0.05; eight trials [16, 27, 40–45], N = 886, of which only two trials [16, 27] reported any events). We found no significant differences in the risk of unplanned extubation, unplanned removal of central venous or arterial lines, pneumothoraces, and cardiac arrests. There was no statistical heterogeneity for adverse event analyses (I 2 = 0%), except for the outcomes of unplanned extubations or endotracheal tube dislodgements (I 2 = 25%) and unplanned removal of central venous or arterial lines (I 2 = 67%). For both of these latter two adverse events, the most recent trial [27] found statistically significantly increased risks.
Post hoc mortality analysis comparing short versus long duration of prone ventilation
In another post hoc analysis, we compared mortality in trials with a mean duration of prone ventilation above the median of 14 h per day (RR 0.86, 95% CI 0.73–1.01; p = 0.07; five trials [18, 27, 40–42], published in 2005 or later, N = 638) with trials with duration of prone ventilation below the median (RR 1.04, 95% CI 0.92–1.17; p = 0.57; four trials [16, 17, 43, 45], published in 2005 or earlier, N = 529). There was a trend to different treatment effects between these longer- versus shorter-duration trials, but the interaction p value was not statistically significant (0.06).
Discussion
The main finding of our systematic review is that mechanical ventilation in the prone position has a different impact on mortality in patients with acute hypoxemic respiratory failure depending on the extent of hypoxemia: it reduces mortality in those with severe hypoxemia, defined by baseline PaO2/FiO2 <100 mmHg, but not in those with less severe hypoxemia. Post hoc analysis demonstrated that the statistically significant difference between the relative risk of death in the more severely hypoxemic subgroup compared with the less severely hypoxemic subgroup was robust across several PaO2/FiO2 thresholds up to approximately 140 mmHg. Other benefits of prone ventilation included significant improvements in oxygenation on days 1–3 and reduced VAP, although there was no decrease in duration of ventilation. The risks of pressure ulcers, endotracheal tube obstruction, and possibly line and tube dislodgement were increased. Results were consistent among trials for mortality and most other clinical outcomes, with low to moderate between-trial differences for oxygenation outcomes, strengthening our findings.
The 16% reduction in the relative risk of death among patients with PaO2/FiO2 <100 mmHg was consistent with our a priori hypothesis that improved oxygenation during prone ventilation would be clinically important in patients at high risk of death from profound hypoxemia. In a post hoc analysis, the first multicenter RCT of prone ventilation [16] showed improved mortality in the quartile of patients with the most severe hypoxemia. The treatment effect, however, did not significantly differ from that in less hypoxemic patients, possibly due to inadequate statistical power. In our meta-analysis, we analyzed mortality stratified by severity of hypoxemia for all trials of prone ventilation which measured this outcome, thereby providing a more robust and powerful analysis.
A physiologic explanation for our finding is that ventilation in the prone position recruits collapsed regions [10, 11] of the lung without increasing airway pressure [16, 18, 41, 42] or hyperinflation [14]. Thus, the delivered tidal volume and peak pressure are dispersed to more alveoli, decreasing the risk of alveolar injury from stretch and strain forces [15]. This lung-protective effect of prone ventilation may be less important in patients with less severe hypoxemic respiratory failure, but appears to be highly relevant for patients with severe hypoxemia (mostly due to ARDS) who are most at risk for alveolar injury from shear and strain forces due to the low ratio of normal to collapsed lung [60]. In severely hypoxemic patients, prone ventilation may provide additive benefit to the lung-protective strategy of lowering delivered tidal volumes [7].
A practical question facing clinicians using this intervention is the optimal duration of prone positioning. This issue is difficult to address with the available data. Our post hoc analysis did not show a significant difference in effect on mortality between trials implementing longer versus shorter daily duration of prone ventilation. Furthermore, the analysis was based on subgroups of trials rather than subgroups of patients within trials, and these subgroups differed in several other important ways. Trials using shorter-duration prone ventilation were published earlier (up to 2005), whereas trials using longer-duration prone ventilation were published since 2005. Consequently, the longer-duration trials were more likely to implement treatments such as low-tidal-volume mechanical ventilation [7] that may have contributed to a reduction in mortality. In addition, the more recently completed trials attempted to enrol patients with more severe hypoxemia and earlier in the course of ARDS [18, 27, 40–42]. Finally, performing trial-level subgroup analysis using the mean overall duration of daily prone ventilation in each trial may lead to ecological bias [61], since it cannot be ascertained whether individuals within each trial who received longer durations of prone ventilation actually benefited more than individuals with shorter durations. In contrast, in the primary subgroup comparison of hypoxemia severity, groups of patients with severe and moderate hypoxemia within each trial were analyzed, limiting the potential for ecological bias.
Prone ventilation tended to reduce VAP, possibly through improved drainage of secretions [13]. Nonetheless, the observed reduction in VAP did not hasten weaning from mechanical ventilation. Moreover, as discussed previously [19], most trials did not blind outcome assessors or mandate duplicate independent VAP adjudication [18, 40, 42–44], and did not use protocols for sedation [16, 17, 27, 40, 43, 45] or ventilator weaning [16, 27, 40, 43–45]. Thus, the finding of reduced VAP must be interpreted cautiously.
Unlike other interventions for ARDS, such as high-frequency oscillation [62] and inhaled nitric oxide [63], prone ventilation is readily implemented in any intensive care unit. However, we found that prone ventilation was not without harm, significantly increasing the risks of pressure ulcers, endotracheal tube obstruction, and chest tube dislodgement. Although we did not find differences in pooled outcomes of other adverse events, one multicenter trial [27] found significantly increased rates of endotracheal tube and intravenous line dislodgements. Such events can have catastrophic effects in such critically ill patients. For example, in another trial [18] cardiac arrest resulted from dislodgement of a pulmonary artery catheter, which was directly attributed to a prone manoeuvre, highlighting that great care and experienced personnel are required when performing this intervention. Indeed, some ICU personnel remain reluctant to use this technique given its risks and perceived effects on other care practices, such as increased sedation needs and reduced enteral feeding [25, 64]. Our finding that prone ventilation benefits primarily the most severely hypoxemic patients, who are uncommonly cared for in many ICUs, challenges caregivers to implement this infrequently performed technique safely [64]. Such patients might be optimally served in higher-volume centres with more experience [65].
Our review has several strengths, including methods to reduce bias and a comprehensive set of relevant clinical and physiological outcomes. Trialists confirmed the primary data, which were analyzed using a predefined statistical plan. The primary hypothesis, that prone ventilation would be of benefit to patients with more severe hypoxemia, was prespecified, biologically plausible, and analyzed using appropriate tests for subgroup effects [66, 67]. However, subgroup analysis should, in general, be hypothesis-generating and confirmed in adequately powered randomized trials, and an ongoing trial targeting the enrolment of 500 patients with PaO2/FiO2 <150 mmHg [59] may provide more definitive data. Unfortunately, over half of the included trials to date were terminated due to slow enrolment. The trials included in this meta-analysis exhibited some methodological diversity (different inclusion criteria, different intervention intensity, etc.); however, for our primary comparison we used patient-level subgroup data, which helps balance out this diversity by producing similar distributions of these trial-specific characteristics in the severe and moderate hypoxemic subgroups. In some trials, some of the patients crossed over from the supine to the prone ventilation group or from the prone to the supine group (either missing one or more prone ventilation sessions or discontinuing prone ventilation prior to meeting prone weaning criteria). For example, in the largest trial [17] many patients randomized to the supine ventilation group whose PaO2/FiO2 decreased to <100 mmHg were treated with prone position ventilation. With our intention-to-treat analysis (i.e., analyzing patients by the group to which they were randomized), such crossovers would tend to reduce measured treatment effects, particularly in the severely hypoxic subgroup. Despite this type of analysis, we still found a significant treatment effect in this subgroup, which strengthens the findings.
Our review has other limitations. First, most trials reported PaO2/FiO2 ratio, which is influenced by ventilator settings and many other factors that are difficult to standardize. An alternative measure, oxygenation index, which incorporates mean airway pressure as a marker of the intensity of mechanical ventilation, was not measured in most trials. However, the finding that a PaO2/FiO2 threshold identifies patients whose survival improves with prone ventilation provides predictive validity to this measure and at a minimum demonstrates that prone ventilation may have different effects on patients with more severe hypoxemia compared with less severe hypoxemia. Our post hoc analysis suggested a PaO2/FiO2 threshold at which prone ventilation begins to be beneficial of approximately 140 mmHg. However, individual patient data meta-analysis [68] would be a more robust method for identifying such a threshold, since it can adjust for patient-level confounders. Individual patient data meta-analytic techniques would also permit the conduct of time-to-event analyses and exploratory analyses of the optimal intervention duration for prone ventilation. Finally, the small number of available trials, many of which accrued fewer than 30 events, reduced the precision of our pooled effect estimates and may have underestimated heterogeneity.
In summary, our systematic review and meta-analysis found that prone ventilation significantly reduced mortality in patients with severe acute hypoxemic respiratory failure but not in patients with less severe hypoxemia. Prone ventilation improved oxygenation but also increased the risk of adverse events. Although the finding of improved mortality in severely hypoxemic patients is based on a subgroup analysis, clinicians may justifiably consider prone ventilation in these patients.
Notes
Two trials were excluded from this subgroup analysis because only one patient [43] or no patients [45] had PaO2/FiO2 <100 mmHg. Adding data from these two trials to the PaO2/FiO2 ≥100 mmHg subgroup caused small changes to the pooled effect estimate for this subgroup (RR 1.05, 95% CI 0.92–1.20, p = 0.44; N = 1,230) and test for subgroup interaction (p = 0.019).
References
Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD (2005) Incidence and outcomes of acute lung injury. N Engl J Med 353:1685–1693
Phua J, Badia JR, Adhikari NK, Friedrich JO, Fowler RA, Singh JM, Scales DC, Stather DR, Li A, Jones A, Gattas DJ, Hallett D, Tomlinson G, Stewart TE, Ferguson ND (2009) Has mortality from acute respiratory distress syndrome decreased over time? A systematic review. Am J Respir Crit Care Med 179:220–227
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 348:683–693
Angus DC, Musthafa AA, Clermont G, Griffin MF, Linde-Zwirble WT, Dremsizov TT, Pinsky MR (2001) Quality-adjusted survival in the first year after the acute respiratory distress syndrome. Am J Respir Crit Care Med 163:1389–1394
Cheung AM, Tansey CM, Tomlinson G, Diaz-Granados N, Matte A, Barr A, Mehta S, Mazer CD, Guest CB, Stewart TE, Al-Saidi F, Cooper AB, Cook D, Slutsky AS, Herridge MS (2006) Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med 174:538–544
Artigas A, Bernard GR, Carlet J, Dreyfuss D, Gattinoni L, Hudson L, Lamy M, Marini JJ, Matthay MA, Pinsky MR, Spragg R, Suter PM (1998) The American–European Consensus Conference on ARDS, part 2. Ventilatory, pharmacologic, supportive therapy, study design strategies, and issues related to recovery and remodeling. Acute respiratory distress syndrome. Am J Respir Crit Care Med 157:1332–1347
(2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 342:1301–1308
Bryan AC (1974) Conference on the scientific basis of respiratory therapy. Pulmonary physiotherapy in the pediatric age group. Comments of a devil’s advocate. Am Rev Respir Dis 110:143–144
Pelosi P, Brazzi L, Gattinoni L (2002) Prone position in acute respiratory distress syndrome. Eur Respir J 20:1017–1028
Gattinoni L, Pesenti A, Baglioni S, Vitale G, Rivolta M, Pelosi P (1988) Inflammatory pulmonary edema and positive end-expiratory pressure: correlations between imaging and physiologic studies. J Thorac Imaging 3:59–64
Gattinoni L, Pelosi P, Vitale G, Pesenti A, D’Andrea L, Mascheroni D (1991) Body position changes redistribute lung computed-tomographic density in patients with acute respiratory failure. Anesthesiology 74:15–23
Pappert D, Rossaint R, Slama K, Gruning T, Falke KJ (1994) Influence of positioning on ventilation–perfusion relationships in severe adult respiratory distress syndrome. Chest 106:1511–1516
Gillart T, Bazin JE, Guelon D, Constantin JM, Mansoor O, Conio N, Schoeffler P (2000) Effect of bronchial drainage on the improvement in gas exchange observed in ventral decubitus in ARDS (French). Ann Fr Anesth Reanim 19:156–163
Galiatsou E, Kostanti E, Svarna E, Kitsakos A, Koulouras V, Efremidis SC, Nakos G (2006) Prone position augments recruitment and prevents alveolar overinflation in acute lung injury. Am J Respir Crit Care Med 174:187–197
Gattinoni L, Protti A (2008) Ventilation in the prone position: for some but not for all? CMAJ 178:1174–1176
Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Labarta V, Malacrida R, Di Giulio P, Fumagalli R, Pelosi P, Brazzi L, Latini R (2001) Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med 345:568–573
Guerin C, Gaillard S, Lemasson S, Ayzac L, Girard R, Beuret P, Palmier B, Le QV, Sirodot M, Rosselli S, Cadiergue V, Sainty JM, Barbe P, Combourieu E, Debatty D, Rouffineau J, Ezingeard E, Millet O, Guelon D, Rodriguez L, Martin O, Renault A, Sibille JP, Kaidomar M (2004) Effects of systematic prone positioning in hypoxemic acute respiratory failure: a randomized controlled trial. JAMA 292:2379–2387
Mancebo J, Fernandez R, Blanch L, Rialp G, Gordo F, Ferrer M, Rodriguez F, Garro P, Ricart P, Vallverdu I, Gich I, Castano J, Saura P, Dominguez G, Bonet A, Albert RK (2006) A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med 173:1233–1239
Sud S, Sud M, Friedrich JO, Adhikari NK (2008) Effect of mechanical ventilation in the prone position on clinical outcomes in patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis. CMAJ 178:1153–1161
Tiruvoipati R, Bangash M, Manktelow B, Peek GJ (2008) Efficacy of prone ventilation in adult patients with acute respiratory failure: a meta-analysis. J Crit Care 23:101–110
Alsaghir AH, Martin CM (2008) Effect of prone positioning in patients with acute respiratory distress syndrome: a meta-analysis. Crit Care Med 36:603–609
Kopterides P, Siempos II, Armaganidis A (2009) Prone positioning in hypoxemic respiratory failure: meta-analysis of randomized controlled trials. J Crit Care 24:89–100
Abroug F, Ouanes-Besbes L, Elatrous S, Brochard L (2008) The effect of prone positioning in acute respiratory distress syndrome or acute lung injury: a meta-analysis. Areas of uncertainty and recommendations for research. Intensive Care Med 34:1002–1011
Sud S, Sud M, Friedrich JO, Adhikari NK (2008) Effect of prone positioning in patients with acute respiratory distress syndrome and high Simplified Acute Physiology Score II. Crit Care Med 36:2711–2712 author reply 2712–2713
Leonet S, Fontaine C, Moraine JJ, Vincent JL (2002) Prone positioning in acute respiratory failure: survey of Belgian ICU nurses. Intensive Care Med 28:576–580
Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G (2006) Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med 354:1775–1786
Taccone P, Pesenti A, Latini R, Polli F, Vagginelli F, Mietto C, Caspani L, Raimondi F, Bordone G, Iapichino G, Mancebo J, Guérin C, Ayzac L, Blanch L, Fumagalli R, Tognoni G, Gattinoni L (2009) Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. JAMA 302:1977–1984
Meade MO, Richardson WS (1997) Selecting and appraising studies for a systematic review. Ann Intern Med 127:531–537
Cook DJ, Guyatt GH, Ryan G, Clifton J, Buckingham L, Willan A, McIlroy W, Oxman AD (1993) Should unpublished data be included in meta-analyses? Current convictions and controversies. JAMA 269:2749–2753
Egger M, Zellweger-Zahner T, Schneider M, Junker C, Lengeler C, Antes G (1997) Language bias in randomised controlled trials published in English and German. Lancet 350:326–329
Berlin JA (1997) Does blinding of readers affect the results of meta-analyses? University of Pennsylvania Meta-analysis Blinding Study Group. Lancet 350:185–186
Schulz KF, Chalmers I, Hayes RJ, Altman DG (1995) Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 273:408–412
Higgins JPT, Green S (eds) (2005) Identifying and measuring heterogeneity. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5. Wiley, Chichester, UK
Montori VM, Devereaux PJ, Adhikari NK, Burns KE, Eggert CH, Briel M, Lacchetti C, Leung TW, Darling E, Bryant DM, Bucher HC, Schunemann HJ, Meade MO, Cook DJ, Erwin PJ, Sood A, Sood R, Lo B, Thompson CA, Zhou Q, Mills E, Guyatt GH (2005) Randomized trials stopped early for benefit: a systematic review. JAMA 294:2203–2209
Friedrich JO, Adhikari NK, Beyene J (2008) The ratio of means method as an alternative to mean differences for analyzing continuous outcome variables in meta-analysis: a simulation study. BMC Med Res Methodol 8:32
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1101
Macaskill P, Walter SD, Irwig L (2001) A comparison of methods to detect publication bias in meta-analysis. Stat Med 20:641–654
Chan MC, Hsu JY, Liu HH, Lee YL, Pong SC, Chang LY, Kuo BI, Wu CL (2007) Effects of prone position on inflammatory markers in patients with ARDS due to community-acquired pneumonia. J Formos Med Assoc = Taiwan yi zhi 106:708–716
Curley MA, Hibberd PL, Fineman LD, Wypij D, Shih MC, Thompson JE, Grant MJ, Barr FE, Cvijanovich NZ, Sorce L, Luckett PM, Matthay MA, Arnold JH (2005) Effect of prone positioning on clinical outcomes in children with acute lung injury: a randomized controlled trial. JAMA 294:229–237
Fernandez R, Trenchs X, Klamburg J, Castedo J, Serrano JM, Besso G, Tirapu JP, Santos A, Mas A, Parraga M, Jubert P, Frutos F, Anon JM, Garcia M, Rodriguez F, Yebenes JC, Lopez MJ (2008) Prone positioning in acute respiratory distress syndrome: a multicenter randomized clinical trial. Intensive Care Med 34:1487–1491
Voggenreiter G, Aufmkolk M, Stiletto RJ, Baacke MG, Waydhas C, Ose C, Bock E, Gotzen L, Obertacke U, Nast-Kolb D (2005) Prone positioning improves oxygenation in post-traumatic lung injury–a prospective randomized trial. J Trauma 59:333–341 discussion 341-333
Watanabe I, Fujihara H, Sato K, Honda T, Ohashi S, Endoh H, Yamakura T, Taga K, Shimoji K (2002) Beneficial effect of a prone position for patients with hypoxemia after transthoracic esophagectomy. Crit Care Med 30:1799–1802
Beuret P, Carton MJ, Nourdine K, Kaaki M, Tramoni G, Ducreux JC (2002) Prone position as prevention of lung injury in comatose patients: a prospective, randomized, controlled study. Intensive Care Med 28:564–569
Friedrich JO, Sud S, Sud M, Adhikari NK (2008) Prone position ventilation for community-acquired pneumonia (letter). J Formos Med Assoc = Taiwan yi zhi 107:191 author reply 192
Chan MC, Hsu JY, Liu HH, Lee YL, Pong SC, Chang LY, Kuo BI, Wu CL (2008) Reply to Friedrich et al. (letter). J Formos Med Assoc = Taiwan yi zhi 107:192
Aufmkolk M, Voggenreiter G, Mattern T (2005) Effect of prone position on lung surfactant composition and function in multiple trauma patients with respiratory dysfunction. Eur J Trauma 31:33–38
Curley MA, Arnold JH, Thompson JE, Fackler JC, Grant MJ, Fineman LD, Cvijanovich N, Barr FE, Molitor-Kirsch S, Steinhorn DM, Matthay MA, Hibberd PL (2006) Clinical trial design–effect of prone positioning on clinical outcomes in infants and children with acute respiratory distress syndrome. J Crit Care 21:23–32 discussion 32–27
Fineman LD, LaBrecque MA, Shih MC, Curley MA (2006) Prone positioning can be safely performed in critically ill infants and children. Pediatr Crit Care Med 7:413–422
Gattinoni L, Tognoni G, Brazzi L, Latini R (1997) Ventilation in the prone position. The Prone-Supine Study Collaborative Group. Lancet 350:815
Gattinoni L, Vagginelli F, Carlesso E, Taccone P, Conte V, Chiumello D, Valenza F, Caironi P, Pesenti A (2003) Decrease in PaCO2 with prone position is predictive of improved outcome in acute respiratory distress syndrome. Crit Care Med 31:2727–2733
Lemasson S, Ayzac L, Girard R, Gaillard S, Pavaday K, Guerin C (2006) Does gas exchange response to prone position predict mortality in hypoxemic acute respiratory failure? Intensive Care Med 32:1987–1993
Leal RP, Gonzalez R, Gaona C, Garcia G, Maldanado A, Dominguez-Cherit G (1997) Randomized trial compare prone vs supine position in patients with ARDS (abstract). Am J Respir Crit Care Med 155:A745
Gaillard S, Guerin C, Avzac L, Girard R (2000) A multicenter randomized controlled trial of prone position in acute respiratory failure [abstract]. Am J Respir Crit Care Med 161:A380
Papazian L, Gainnier M, Marin V, Donati S, Arnal JM, Demory D, Roch A, Forel JM, Bongrand P, Bregeon F, Sainty JM (2005) Comparison of prone positioning and high-frequency oscillatory ventilation in patients with acute respiratory distress syndrome. Crit Care Med 33:2162–2171
Demory D, Michelet P, Arnal JM, Donati S, Forel JM, Gainnier M, Bregeon F, Papazian L (2007) High-frequency oscillatory ventilation following prone positioning prevents a further impairment in oxygenation. Crit Care Med 35:106–111
Ibrahim TS, El-Mohamady HS (2007) Inhaled nitric oxide and prone position: How far they can improve oxygenation in pediatric patients with acute respiratory distress syndrome? J Med Sci 7:390–395
Guerin C (2009) Effect of early prone postioning on mortality in patients with severe and persistent acute respiratory distress syndrome. Reanimation 18:146–153
Gattinoni L, Pesenti A (2005) The concept of “baby lung”. Intensive Care Med 31:776–784
Greenland S, Morgenstern H (1989) Ecological bias, confounding, and effect modification. Int J Epidemiol 18:269–274
Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG, Carlin B, Lowson S, Granton J (2002) High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. Am J Respir Crit Care Med 166:801–808
Adhikari NK, Burns KE, Friedrich JO, Granton JT, Cook DJ, Meade MO (2007) Effect of nitric oxide on oxygenation and mortality in acute lung injury: systematic review and meta-analysis. BMJ 334:779
Bein T, Ritzka M, Schmidt F, Taeger K (2007) Positioning therapy in intensive care medicine in Germany. Results of a national survey (German). Der Anaesthesist 56:226–231
Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD (2006) Hospital volume and the outcomes of mechanical ventilation. N Engl J Med 355:41–50
Assmann SF, Pocock SJ, Enos LE, Kasten LE (2000) Subgroup analysis and other (mis)uses of baseline data in clinical trials. Lancet 355:1064–1069
Oxman AD, Guyatt GH (1992) A consumer’s guide to subgroup analyses. Ann Intern Med 116:78–84
Sud S, Douketis J (2009) ACP Journal Club. The devil is in the details… or not? A primer on individual patient data meta-analysis. Ann Intern Med 151:JC1-2, JC1-3
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American–European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
Haynes RB, McKibbon KA, Wilczynski NL, Walter SD, Werre SR (2005) Optimal search strategies for retrieving scientifically strong studies of treatment from Medline: analytical survey. BMJ 330:1179
Wong SS, Wilczynski NL, Haynes RB (2006) Developing optimal search strategies for detecting clinically sound treatment studies in EMBASE. J Med Libr Assoc 94:41–47
Acknowledgments
The authors would like to thank Ippei Watanabe and Hideyoshi Fujihara (see reference [44]) for providing additional trial data, Elizabeth Uleryk for assistance with the search strategy, and an anonymous reviewer for suggesting the post hoc subgroup analysis using a range of PaO2/FiO2 thresholds. Dr. Friedrich is a clinician–scientist of the Canadian Institutes of Health Research (CIHR). Dr. Curley was funded by the National Institutes of Health/National Institute of Nursing Research (NIH/NINR) (Grant No. RO1NR05336).
Conflict of interest statement
Dr. Gattinoni received a fee of 1,500 USD 5 years ago for one meeting at KCI Medical Products headquarters, as a member of an advisory board. The other authors declare no financial or other conflicts of interest to disclose. None of the funding agencies had any involvement in the study. The authors declare that they had full control of all primary data and that they agree to allow the journal to review their data if requested.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: doi:10.1007/s00134-009-1749-0.
Appendix: Literature search
Appendix: Literature search
The following databases were searched in OVID on November 14, 2009: MEDLINE (1950 to present), EMBASE (1980 to week 46, 2009), and Cochrane Central Register of Controlled Trials (fourth quarter 2009).
MEDLINE
-
1.
(pron$ adj4 position$).mp.
-
2.
clinical trial.mp. or clinical trial.pt. or random:.mp. or tu.xs.
-
3.
1 and 2
EMBASE
-
4.
(pron$ adj4 position$).mp.
-
5.
random:.tw. or clinical trial:.mp. or exp health care quality/
-
6.
1 and 2
Cochrane Central Register of Controlled Trials
-
7.
(pron$ adj4 position$).mp.
MEDLINE, 1,491 records
EMBASE, 807 records
CENTRAL, 385 records
Total records retrieved, 2,683
Number after duplicates manually removed, 1,870
Retrieved for more detailed evaluation, 52
Notes: “$” retrieves unlimited suffix variations. The “.mp.” extension includes the title, original title, and abstract fields in all databases, in addition to the subject heading of “prone position” in MEDLINE. Filters for MEDLINE [70] (line 2) and EMBASE [71] (line 5) are based on published sensitive strategies for retrieving randomized trials.
Rights and permissions
About this article
Cite this article
Sud, S., Friedrich, J.O., Taccone, P. et al. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med 36, 585–599 (2010). https://doi.org/10.1007/s00134-009-1748-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1748-1