Abstract
Background
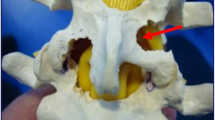
Sufficient decompression of the nerve root canal is still regarded as the method of choice when operating on patients with lumbar disc herniation (LDH) with lumbar lateral recess stenosis; however, tissue-sparing procedures are becoming more popular. Endoscopic techniques offer advantages and the benefits of rehabilitation, which have become the standard in many surgical operations when operating on the spine. A significant issue has been the upgrading of instruments to provide enough bone resection under continuous visual control.
Material and methods
We examined patients who had LDH with lateral recess stenosis and compared the results of nerve root canal decompression using percutaneous endoscopic lumbar discectomy (PELD) with a microsurgical laminotomy (ML) technique. In this study 40 patients with full endoscopic decompression or microsurgery were followed up for 2 years. In addition to general and specific parameters, the following two parameters were also used for the investigation: the Visual Analog Scale (VAS) and the Oswestry Disability Index (ODI).
Results
Except for 1 patient in whom repair was done by fusion and 1 who was lost to follow-up, 38 patients remained in the study over the 2 years. The mean operating time in the PELD group was longer (p < 0.05), but intraoperative and postoperative blood loss was less than in the ML group (p < 0.05). The postoperative results were better than before surgery, and the VAS and ODI parameters indicated a clear improvement in leg pain and daily activities in both groups (p > 0.05). Of the patients three suffered increasing back pain (2 ML, 1 PELD).
Conclusion
The results indicated that the PELD can provide an effective supplement and serve as an alternative for LDH with lateral recess stenosis compared with the ML technique when the indication criteria are fulfilled. The PELD also has the advantage of being a minimally invasive intervention.
Zusammenfassung
Hintergrund
Die ausreichende Dekompression des Nervenwurzelkanals wird bei der Operation von Patienten mit einem Bandscheibenvorfall an der Lendenwirbelsäule (LDH) mit lumbaler lateraler Rezessusstenose nach wie vor als Methode der Wahl angesehen, jedoch werden gewebeerhaltende Verfahren immer beliebter. Endoskopische Verfahren, die bei vielen chirurgischen Eingriffen an der Wirbelsäule Standard sind, bieten Vorteile und eine bessere Rehabilitation. Ein signifikantes Problem war das Upgrading der Instrumente, um unter kontinuierlicher visueller Kontrolle ausreichend Knochenresektion zu gewährleisten.
Material und Methoden
Patienten mit einem Bandscheibenvorfall an der Lendenwirbelsäule mit lateraler Rezessusstenose wurden untersucht und die Ergebnisse der Nervenwurzelkanaldekompression mittels perkutaner endoskopischer lumbaler Diskektomie (PELD) mit einer mikrochirurgischen Laminotomie (ML) verglichen. In dieser Studie wurden 40 Patienten mit einer vollständigen endoskopischen Dekompression oder Mikrochirurgie für 2 Jahre nachbeobachtet. Zusätzlich zu den allgemeinen und spezifischen Parametern wurden noch die 2 folgenden Parameter für die Untersuchung verwendet: die visuelle Analogskala (VAS) und der Oswestry Disability Index (ODI).
Ergebnisse
Außer einem Patienten, der mittels Fusion behandelt wurde, und einem Patienten, der für die Nachbeobachtung nicht mehr zur Verfügung stand („lost to follow up“), blieben 38 Patienten für 2 Jahre in der Studie. Die mittlere Operationszeit in der PELD-Gruppe war länger (p < 0,05), aber der intraoperative und postoperative Blutverlust waren geringer als in der ML-Gruppe (p < 0,05). Die postoperativen Ergebnisse waren besser als vor dem Eingriff, und die Parameter von VAS und ODI zeigten eine deutliche Verbesserung der Beinschmerzen sowie der täglichen Aktivitäten in beiden Gruppen (p > 0,05). Drei Patienten hatten zunehmende Rückenschmerzen (2 ML, 1 PELD).
Schlussfolgerung
Die Ergebnisse zeigten, dass die PELD eine effektive Ergänzung sein kann und eine Alternative für LDH mit lateraler Rezessusstenose darstellt im Vergleich zur ML-Technik, sofern die Indikationskriterien erfüllt sind. Vorteil der PELD ist auch, dass es sich dabei um ein minimal-invasives Verfahren handelt.





Similar content being viewed by others
Abbreviations
- LDH:
-
Lumbar disc herniation
- MISTLIF:
-
Minimally invasive surgery transforaminal lumbar interbody fusion
- ML:
-
Microsurgical laminotomy
- MRI:
-
Magnetic resonance imaging
- NSAID:
-
Non-steroidal anti-inflammatory drugs
- ODI:
-
Oswestry disability index
- PELD:
-
Percutaneous endoscopic lumbar discectomy
- TLIF:
-
Transforaminal lumbar interbody fusion
- VAS:
-
Visual analog scale
References
Parke WW (1991) The significance of venous return in ischemic radiculopathy and myelopathy. Orthop Clin North Am 22:213–220
Schick U, Doehnert J, Richter A et al (2002) Microendoscopic lumbar discectomy versus open surgery: anintraoperative EMG study. Eur Spine J 11:20–26
Weber BR, Grob D, Dvorak J et al (1997) Posterior surgical approach to the lumbar spine and its effect on the multifidusmuscle. Spine 22:1765–1772
Ruetten S, Komp M, Merk H et al (2008) Full-endoscopic anterior decompression versus conventional anterior decompression and fusion in cervical disc herniations. Int Orthop 33:1677
Ruetten S, Komp M, Merk H et al (2009) Recurrent lumbar disc herniation following conventional discectomy: a prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech 22:122–129
Ruetten S, Komp M, Merk H et al (2008) Full-endoscopic cervical posterior foraminotomy for the operation of lateraldisc herniations using 5.9 mm endoscopes: A prospective, randomized, controlled study. Spine 33:940–948
Ruetten S, Komp M, Merk H et al (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versusconventional microsurgical technique: a prospective, randomized, controlled study. Spine 33:931–939
Ruetten S, Komp M, Merk H et al (2007) Use of newly developed instruments and endoscopes: full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine 6(6):521–530
Ruetten S, Komp M, Godolias G (2005) An extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using the full-endoscopic uniportal transforaminal approach, techniqueand prospective results of 463 patients. Spine 30:2570–2578
Komp M, Hahn P et al (2015) Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomytechnique: a prospective, randomized, controlled study. Pain Physician 18:61–70
Jasper GP, Francisco GM, Telfeian AE (2014) Transforaminal endoscopicdiscectomy with foraminoplasty for the treatment of spondylolisthesis. Pain Physician 17:E703–E708
Kitahama Y, Sairyo K, Dezawa A (2013) Percutaneous endoscopic transforaminalapproach to decompress the lateral recess in an elderly patient with spinalcanal stenosis, herniated nucleus pulposus and pulmonary comorbidities. Asian J Endosc Surg 6:130–133
Caputy AJ, Luessenhop AJ (1992) Long-term evaluation of decompressive surgery for degenerative lumbar stenosis. J Neurosurg 7:669–676
Fox MW, Onofrio BM, Hanssen AD (1996) Clinical outcomes and radiological instability following decompressive lumbarlaminectomy for degenerative spinal stenosis: a comparison of patients undergoing concomitant arthrodesis versus decompression alone. J Neurosurg 85:793–802
Schoeggl A, Maier H, Saringer W et al (2002) Outcome after chronic sciatica as the only reason for lumbar microdiscectomy. J Spinal Disord Tech 15:415–419
Ragab AA, Fye MA, Bohlmann HH (2003) Surgery of the lumbar spine for spinal stenosis in 118 patients 70 years of age or older. Spine 28:348–353
Cooper R, Mitchell W, Illingworth K et al (1991) The role of epidural fibrosis and defective fibrinolysis in the persistence of postlaminectomy back pain. Spine 16:1044–1048
Lewis PJ, Weir BKA, Broad RW et al (1987) Long-term prospective study of lumbosacral discectomy. J Neurosurg 67:49–54
Waddell G, Reilly S, Torsney B et al (1988) Assessment of the outcome of low back surgery. J Bone Joint Surg Br 70:723–727
Yamashita K, Ohzono K, Hiroshima K (2006) Five-year outcomes of surgical treatment for degenerative lumbar spinalstenosis. Spine 31:1484–1490
Malmivaara A, Slaetis P, Helioevaara M et al (2007) Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine 32:1–8
Podichetty VK, Spears J, Isaacs RE et al (2006) Complications associated with minimally invasive decompressionfor lumbar spinal stenosis. J Spinal Disord Tech 19:161–166
Ruetten S, Komp M, Merk H et al (2008) Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar and transforaminal approach versus conventional microsurgicaltechnique: a prospective, randomized, controlled study. J Neurosurg Spine 10:476–485
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
L. Kong, X.-F. Shang, W.-Z. Zhang, L.-Q. Duan, Y. Yu, W.-J. Ni and Y. Huang declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki Declaration of 1975 (in its current revised form). Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kong, L., Shang, XF., Zhang, WZ. et al. Percutaneous endoscopic lumbar discectomy and microsurgical laminotomy. Orthopäde 48, 157–164 (2019). https://doi.org/10.1007/s00132-018-3610-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-018-3610-z