Abstract
Aims/hypothesis
Contemporary data for the association of diabetes with haematological malignancies are lacking. We evaluated the risk of developing haematological malignancies and subsequent mortality in individuals with diabetes compared with those without diabetes.
Methods
We conducted a population-based observational study using healthcare databases from Ontario, Canada. All Ontario residents 30 years of age or older free of cancer and diabetes between 1 January 1996 and 31 December 2015 were eligible for inclusion. Using Cox regression analyses, we explored the association between diabetes and the risk and mortality of haematological malignancies (leukaemia, lymphoma, multiple myeloma). The impact of timing on associations was evaluated with analyses stratified by time since diabetes diagnosis (<3 months, 3 months to 1 year, ≥1 year).
Results
We identified 1,003,276 individuals with diabetes and age and sex matched these to 2,006,552 individuals without diabetes. Compared with individuals without diabetes, those with diabetes had a modest but significantly higher risk of a haematological malignancy (adjusted HR 1.10 [95% CI 1.08, 1.12] p < 0.0001). This association persisted across all time periods since diabetes diagnosis. Among those with haematological malignancies, diabetes was associated with a higher all-cause mortality (HR 1.36 [95% CI 1.31, 1.41] p < 0.0001) compared with no diabetes, as well as cause-specific mortality.
Conclusions/interpretation
Diabetes is associated with a higher risk of haematological malignancies and is an independent risk factor of all-cause and cause-specific mortality. Greater efforts for lifestyle modification may not only reduce diabetes burden and its complications but may also potentially lower risk of malignancy and mortality.

Graphical abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Diabetes and cancer are common conditions associated with significant morbidity and mortality. Epidemiological evidence indicates that diabetes is associated with higher incidence of several cancers and increased mortality after cancer [1,2,3]. Much of the data to date have focused on solid malignancies with increased risk for malignancies including colorectal, liver, pancreatic, breast and endometrial cancer [4,5,6], while less conclusive data exist for diabetes and haematological malignancy risk.
Haematological malignancies are the fourth leading cause of malignancy in North America. In 2020, an estimated 178,520 individuals in the USA are expected to be diagnosed with leukaemia, lymphoma or myeloma, with the number of deaths estimated at 56,840 individuals (9.4% of all deaths from malignancy) [7]. The exact aetiology of haematological malignancies has not been completely elucidated. Biological plausibility exists for the epidemiological association between diabetes and haematological malignancies. Diabetes is associated with immunosuppression, chronic inflammation and lymphocyte dysfunction [8], all of which are implicated in haematological malignancies [9, 10]. Furthermore, additional postulated mechanisms for increased risk of malignancy in diabetes include hyperinsulinaemia, IGF overproduction and upregulation of IGF-1 receptor [11]. Given that obesity is a known major risk factor for development of diabetes, obesity may be an important mediator of the relationship between diabetes and malignancy. However, the extent to which diabetes independently contributes to the risk of haematological malignancy has not been determined.
Nevertheless, as previously mentioned, prior studies evaluating the association between diabetes and haematological malignancies have yielded inconclusive results, limited by sample size and definition of diabetes [12,13,14,15,16]. Tsilidis et al conducted an umbrella meta-analysis to evaluate strength of current evidence for the association between type 2 diabetes and the risk of developing cancer and mortality, and concluded that significant heterogeneity exists for haematological malignancy associations, raising concern for validity of current evidence [6]. Accordingly, there is currently insufficient evidence to definitively establish the association between diabetes and haematological malignancies and whether diabetes is associated with worse prognosis.
Given the limited existing research, a large population-based study is required to investigate the association between diabetes and haematological malignancies, both overall and by subtype. Our secondary objective was to evaluate whether diabetes is an independent risk factor for mortality in those who develop a haematological malignancy.
Methods
Study design
We conducted a population-based retrospective cohort study using linked administrative databases, held at ICES in Ontario, Canada. This study complied with ICES data confidentiality and privacy guidelines and was approved by the Research Ethics Boards at the Sunnybrook Health Sciences Center and the University of Toronto (Toronto, Ontario, Canada).
Data sources
All data for eligible individuals identified were linked to multiple health databases held securely at ICES using an encrypted version of the Ontario Health Card number. Ontario is Canada’s most populous province, with an ethnically diverse population of 14 million, with medical care covered by the province’s universal, publicly funded single-payer health insurance plan (Ontario Health Insurance Plan, OHIP).
Demographic, comorbidity, medication, exposure and outcome data were obtained from the appropriate databases. Diabetes status was identified from the Ontario Diabetes Database (ODD). The ODD is a validated administrative database registry containing data for people diagnosed with diabetes, whereby diabetes diagnosis is defined based on two physician OHIP claims or one diabetes Ontario Drug Database (ODB) claim or one Canadian Institute of Health Information (CIHI) Discharge Abstract Database (DAD) admission within 1 year [17]. This database has been validated against primary care records with high sensitivity (90%) and specificity (98%) for identifying individuals clinically diagnosed with diabetes. Demographic and vital status data were ascertained from the Registered Persons Database (RPDB). The RPDB obtains neighbourhood income data from Statistics Canada to determine quintile of median income based on postal code. Covariate data were ascertained from the DAD and OHIP physician claims. The CIHI DAD database collect data on all hospitalisations to all Ontario hospitals, including in-hospital diagnosis and comorbidities. These datasets are highly complete as submission of records to CIHI is mandated. Given Ontario’s universal health insurance, OHIP contains physician claims for all outpatient visits and identified comorbidities. Finally, haematological malignancy diagnoses were ascertained from the Ontario Cancer Registry (OCR). The OCR is a population-based provincial-wide cancer registry that captures all incident cancer diagnoses and all cancer deaths in Ontario residents since 1964 (except for non-melanoma skin cancers). The OCR cancer case ascertainment is estimated to be over 95% complete [18, 19]. The current OCR follows the National Cancer Institute’s Surveillance, Epidemiology, and End Results coding rules. Haematological malignancies were ascertained using the International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) codes (electronic supplementary material [ESM] Table 1).
Additional details around these databases can be found at: https://www.ices.on.ca/Data-and-Privacy/ICES-data/Data-dictionary.
Study population
All Ontario residents ≥30 years of age with no previous history of cancer from 1 January 1996 to 31 December 2015 were eligible for inclusion. The exclusion criteria were as follows: diabetes diagnosis before age 30 (to avoid inclusion of people with type 1 diabetes); any malignancy prior to diabetes diagnosis; those with invalid health card numbers; palliative and long-term care residents; and individuals with no healthcare contact within 2 years of the index date.
Exposure
The exposure of interest was a diabetes diagnosis between 1 January 1996 and 31 December 2015. We first identified individuals diagnosed with diabetes during the study period, with the date of diabetes diagnosis serving as their index date. We then matched each individual with diabetes with up to two eligible individuals without diabetes in the RPDB database based on age (within 1 year) and sex, followed by assigning them the same index date as their matched diabetes counterpart.
Study outcomes
The primary outcome was incident haematological malignancy, which was a composite of leukaemia, lymphoma or multiple myeloma. Lymphoma includes all Hodgkin lymphoma and non-Hodgkin lymphoma. In secondary analyses, we evaluated the incidence of each individual haematological malignancy type. For subgroup analysis, we examined the incidence for acute vs chronic leukaemia, and indolent-histology vs aggressive-histology lymphoma (ESM Table 1). Of note, chronic myelogenous leukaemia was categorised as a chronic leukaemia while chronic lymphocytic leukaemia was categorised as an indolent lymphoma as per WHO classification [20].
In the subset of patients who developed a haematological malignancy, the primary outcome was all-cause mortality based on death certificate records from the RPDB and the secondary outcome was cancer-specific mortality based on OCR death records by ICD-9/10 codes (www.icd9data.com/2007/Volume1;http://apps.who.int/classifications/icd10/browse/2016/en), to compare the impact of diabetes vs no diabetes on mortality risk.
Individuals were followed from index date until diagnosis of a haematological malignancy, death, or end of follow-up (31 December 2016), whichever came first. Individuals were censored at the time of haematological malignancy, death, diagnosis of a non-haematological malignancy, or the end of follow-up. The subgroup of patients who developed a haematological malignancy were followed until death or end of follow-up (31 December 2016).
Statistical analysis
Baseline data were analysed using descriptive statistics, with standardised differences between diabetes vs no diabetes shown in Table 1. We used univariate and multivariable Cox proportional hazard regression to examine the association between diabetes and haematological malignancies and estimated the HR and 95% CI. Subgroup analysis was also conducted for haematological malignancy subtypes, as well as acute vs chronic leukaemia, and indolent vs aggressive lymphoma. The models were adjusted for the following covariates: age, sex, region of residence, neighbourhood income quintile, hospitalisations in the prior year, healthcare visits in the prior year, and baseline comorbidities using diagnostic codes from physician claims and hospital discharge abstracts (anaemia, dyslipidaemia, myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, chronic obstructive pulmonary disease, chronic kidney disease, solid organ transplantation, connective tissue disease) (ESM Table 2).
We carried out subgroup analyses among those who developed a haematological malignancy to estimate the associations between diabetes and all-cause and cancer-specific mortality overall and by cancer site. We then conducted univariate and multivariable Cox regression analyses, and the cause-specific HR were estimated for cancer-specificity mortality outcomes to account for the competing risk of non-cancer deaths. Cause-specific ICD codes are provided in ESM Table 3. Analyses were also stratified by age (<65 vs ≥65) and sex.
We conducted two sensitivity analyses to examine the potential influence of detection bias—whereby increased healthcare contact associated with a new diagnosis of diabetes leads to the detection of cancers—on our findings. First, we stratified follow-up time (0–3 months, 3 months–1 year, >1 year), to determine whether cancer events were higher in the period immediately after a diabetes diagnosis when health contact is highest. Second, we determined whether diabetes is associated with a higher incidence of osteoporosis, which would suggest a detection bias rather than a causal effect.
For all analyses, a two-tailed p value <0.05 was considered statistically significant. Analyses were conducted using SAS version 9.4 (Cary, NC, USA).
Results
Participant characteristics
We identified 1,003,276 individuals with diabetes, and they were age (within 1 year) and sex matched to 2,006,552 control participants without diabetes, whereby 47.8% were female and mean age was 57.6 years (SD 13.3 years) (Table 1, Fig. 1). Compared with control participants, individuals with diabetes were more likely to have pre-existing hypertension and congestive heart failure, as well as a greater number of physician visits within 2 years of index date. For the entire cohort, the median follow-up time between diagnosis of diabetes and malignancy diagnosis, censoring or end of follow-up was 11.0 years (IQR range 6.7–15.6 years).
Association between diabetes and haematological malignancies
Among individuals with diabetes, 15,856 (138.6 per 100,000 person-years) developed an incident haematological malignancy, and 21,748 individuals without diabetes developed an incident haematological malignancy (104.0 per 100,000 person-years) (Table 2).
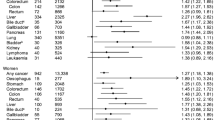
Diabetes was associated with a significant increase in risk of developing a haematological malignancy with univariate analysis (HR 1.14 [95% CI 1.12, 1.16] p < 0.0001) and multivariable Cox regression (adjusted HR 1.10 [95% CI 1.08, 1.12] p < 0.0001; Table 2). Solid organ transplantation (HR 2.49 [95% CI 2.09, 2.96] p < 0.0001) and connective tissue disease (HR 1.60 [95% CI 1.43, 1.79] p < 0.0001) were associated with increased risk of developing a haematological malignancy (data not shown). No major differences were observed for stratified analyses comparing HRs between men and women or age <65 and ≥65 years of age (Table 2). Results were consistent across haematological malignancy subtypes (Table 2). In subgroup analysis, diabetes was associated with an increased risk for both acute (adjusted HR 1.20 [95% CI 1.12, 1.27] p < 0.0001) and chronic leukaemia (adjusted HR 1.27 [95% CI 1.14, 1.41] p < 0.0001), as well as aggressive lymphoma (adjusted HR 1.14 [95% CI 1.10, 1.18] p < 0.0001) but not indolent lymphoma (adjusted HR 1.02 [95% CI 0.98, 1.05] p = 0.37).
Subgroup analysis: all-cause and cancer-specific mortality
The median time from haematological malignancy diagnosis to end of follow-up, censoring or death was 3.0 years (IQR 0.8–6.3). There were 21,985 overall deaths, of which 4475 (33.78 per 100 person-years), 12,789 (10.26 per 100 person-years) and 4721 (19.92 per 100 person-years) occurred in the leukaemia, lymphoma and multiple myeloma subgroups, respectively. People with diabetes had significantly more deaths from any cause than individuals without diabetes (60.6% vs 56.4%, adjusted HR 1.36 [95% CI 1.31, 1.41] p < 0.0001; Table 3). Similar findings were seen for cancer subtypes (Table 3). Diabetes was also associated with a higher risk of cancer-specific mortality compared with no diabetes among those who developed leukaemia (adjusted HR 1.13 [95% CI 1.00, 1.27] p = 0.049), lymphoma (adjusted HR 1.14 [95% CI 1.05, 1.24] p = 0.0017), or multiple myeloma (adjusted HR 1.29 [95% CI 1.15, 1.44] p < 0.0001) (Table 4). No major differences were observed when comparing HRs between men and women or age <65 and ≥65 (Tables 3 and 4 for all-cause and cancer-specific mortality, respectively).
Sensitivity analyses
Temporal relationship between diabetes and haematological malignancy
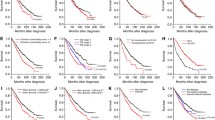
Findings were robust across all time periods after a diabetes diagnosis, although differences in haematological malignancy risk in the <3 month and 3 months to 1 year periods did not reach statistical significance (Fig. 2). This is likely due to fewer cases during the initial time windows, with incidence rates of 2.48 and 9.90 per 100,000 person-years in patients with diabetes for <3 months and 3 months to 1 year, respectively, compared with 110.18 per 100,000 person-years for the period beyond 1 year. Notably, the risk of haematological malignancy associated with diabetes remained significantly increased for malignancies diagnosed beyond 1 year after diabetes diagnosis (HR 1.10 [95% CI 1.08, 1.12] p < 0.0001), arguing against the presence of a detection bias. These results were similar for haematological malignancy subtypes leukaemia, lymphoma and multiple myeloma (Fig. 2).
Diabetes and risk of osteoporosis
We evaluated the risk of diabetes with osteoporosis, a negative tracer observed less frequently in diabetes, to examine whether the elevated haematological malignancy risk among individuals with new diagnosis of diabetes is due to enhanced healthcare contact. There was a significantly lower risk of osteoporosis in individuals with diabetes (HR 0.57 [95% CI 0.57, 0.58] p < 0.0001) compared with no diabetes. This was similarly observed during all three time periods after diabetes diagnosis (data not shown).
Discussion
In this large, population-based cohort study, we demonstrated that diabetes is associated with a modestly increased risk of a subsequent haematological malignancy. This association persisted beyond the period after a diabetes diagnosis, which argues against a detection bias due to enhanced health contact. We also showed that people with diabetes who develop a haematological malignancy have a 36% higher risk of all-cause mortality compared with those without diabetes. These findings indicate that, similar to solid malignancies, diabetes may represent an under-recognised risk factor for haematological cancers.
Our study is concordant with a 2012 meta-analysis of 26 observational studies (13 case–control, 13 cohort studies) demonstrating that diabetes was associated with a 22% increased risk of incident haematological malignancy (non-Hodgkin lymphoma, leukaemia and multiple myeloma) [21]. Subsequently, Tsilidis et al conducted an umbrella meta-analysis to evaluate strength of current evidence for the association between type 2 diabetes and the risk of developing or dying from cancer [6]. They concluded that significant heterogeneity exists for haematological malignancy associations, raising concern for validity of current evidence [6]. There were also methodological concerns in the included studies. First, diabetes was ascertained based on self-report in the majority of studies [21]. Second, residual confounding is an important concern as many studies adjusted for basic demographic variables without adjusting for comorbidities. In this study we used a validated algorithm for identifying diabetes at the population level and adjusted for confounders to better model the association between diabetes and haematological malignancy. To the best of our knowledge, this is the largest study to date evaluating the association between diabetes and haematological malignancies.
There have been several potential biological explanations underlying the relationship between diabetes and malignancies. A joint consensus report on diabetes and cancer published by the ADA and the American Cancer Society highlighted hyperinsulinaemia, hyperglycaemia, inflammatory cytokines, IGF overproduction and upregulation of IGF-1 receptors as potential mechanisms for malignant transformation and progression of tumours [22]. Although these mechanisms have been proposed to explain the observed association between diabetes and higher risk of cancer in general, causality has yet to be formally established. Of note, the epidemiological association between diabetes and cancer may be related to residual confounding from shared risk factors such as adiposity, diet, lifestyle factors such as physical inactivity, smoking and alcohol consumption which are not easily obtained in a population-based cohort study. Indeed, increased BMI has been positively associated with an increased risk of haematological malignancies including certain subtypes of non-Hodgkin lymphoma, acute myelogenous and acute lymphoblastic leukaemia, and multiple myeloma [23]. For instance, a pooled analysis conducted by the InterLymph consortium demonstrated that obesity was mainly associated with increased risk of diffuse large B cell lymphoma (DLBCL), but not other non-Hodgkin lymphoma [24]. A subsequent meta-analysis by Castillo et al demonstrated a 14% increase in DLBCL incidence for each 10 kg/m2 increase in BMI [25]. Given that obesity is a known major risk for development of insulin resistance and type 2 diabetes, we recognise that obesity may be an important potential mediator of malignancy risk associated with diabetes. However, there are currently insufficient studies evaluating the mediation of obesity on diabetes and haematological malignancy risk. A recent study by Pearson-Stuttard et al used RRs from published meta-analyses to estimate the independent risk of incident cancers attributable to obesity and diabetes [26]. In that study, they estimated that 5.6% of all incident cancers in 2012 were attributable to the combined effects of diabetes and high BMI. Although BMI accounted for twice as many incident cancer cases as diabetes, diabetes remained an independent risk factor of incident cancer after accounting for BMI. Taken together, future studies incorporating BMI and diabetes will help to separate effects of BMI on diabetes and haematological malignancy risk.
Haematological malignancies are a heterogenous group of cancers characterised by uncontrolled growth of haematopoietic or lymphoid tissues, which can exhibit an indolent to aggressive clinical course [27]. Known risk factors include age, toxic exposures such as benzene and ionising radiation, genetic syndromes, as well as viruses such as HIV, Epstein–Barr virus and human T-lymphotropic virus type 1. One biological plausibility for the association between diabetes and haematological malignancy is the notion that diabetes can result in immunosuppression, chronic inflammation and lymphocyte (B and T cells) dysfunction in the form of impaired neutrophil activity, suppression of cellular immunity and alterations in serum immunoglobulins [8]. Immune dysfunction has been implicated in the pathogenesis of haematological malignancies, particularly for lymphoproliferative disorders [9, 10]. As highlighted above, previous research has suggested that insulin and IGF-1 are important in the pathogenesis of multiple myeloma [11]. Further supporting the role of diabetes on malignancy risk, metformin use has been associated with reduced progression from monoclonal protein of undetermined significance to multiple myeloma [28]. Interestingly, previous studies demonstrated that the use of metformin was associated with improved outcomes in cancer patients and perhaps even reduced risk of incident cancer in metformin users [16, 29,30,31].
In contrast, some have argued that the increase in cancer risk in patients with diabetes is due to a detection bias. Detection bias refers to increased detection of malignancy in individuals with new diagnosis of diabetes, attributed to increased healthcare contact and investigations [32,33,34]. Prior studies by our group [5] and others [35, 36] have shown that the strongest association between diabetes and solid cancer is found in the immediate post-diabetes diagnosis period (i.e. 3 months, 6 months), followed by a decline as duration of diabetes increases. In this study, while point estimates appeared modestly higher in the first 3 months after diabetes diagnosis, the strength of association between diabetes and haematological cancers did not vary significantly across time, and remained significantly increased in the period ≥1 year following diabetes diagnosis. We also failed to show an increase in risk of osteoporosis, a condition that tends to be less common in individuals with diabetes, in the early period after diabetes diagnosis, which would have confirmed the presence of a detection bias if general enhanced screening around time of diabetes diagnosis occurred [37]. Taken together, these results argue against detection bias as a primary mechanism for our findings.
Herein, we demonstrated that diabetes was an independent predictor of both all-cause and cause-specific mortality among patients with haematological malignancies. Not surprisingly, the increase in all-cause mortality was greater than for cause-specific mortality, suggesting that diabetes has a greater impact on non-cancer-related mortality than on cancer-specific mortality. This finding is consistent with other studies, and likely reflects the added burden of diabetes-related causes of death. This emphasises the importance of providing ongoing diabetes management and optimisation of cardiovascular health to improve clinical outcomes after malignancy diagnosis. Nevertheless, we also found that diabetes was associated with a significant 13–29% rise in cancer-specific deaths among patients with leukaemia, lymphoma and multiple myeloma, respectively, suggesting a unique association between diabetes and haematological malignancies. To the best of our knowledge, our study is the largest study to date to investigate the role of diabetes on mortality risk using population-based data spanning several decades, pertinent to the growing incidence of both diabetes and haematological malignancies. The fact that this trend is observed despite advances in diagnosis and treatment of both disease states suggests that further awareness of the association is needed. We postulate several potential mechanisms for the observed relationship between diabetes and cancer-related mortality, including diabetes-related complications such as autonomic dysfunction that may decrease tolerability of chemotherapy, as well as potential decrease in adherence with follow-up and therapies.
As previously mentioned, diabetes has been independently associated with higher mortality after a cancer diagnosis, with strongest risks for breast and colorectal cancer. A recent pooled analysis of 97 prospective studies conducted by the Emerging Risk Factors Collaboration demonstrated that diabetes is associated with a 25% increase in mortality risk [38]. The majority of studies used all-cause mortality and while some reports demonstrated increased risk of cancer-specific mortality in patients with diabetes [16, 39], others did not [40, 41]. Recent studies conducted by our group reported that breast and colorectal cancer patients with diabetes had higher all-cause mortality but similar cause-specific mortality compared with those without diabetes [5, 42]. There have been several studies evaluating the prognostic role of diabetes on mortality risk of individuals with haematological malignancy, demonstrating variable risk of diabetes on mortality.
In the largest cohort study (aside from ours), of 80,397 individuals with diabetes between 1995 and 1998, there was a modest increased risk and mortality of non-Hodgkin lymphoma [14], while a small cohort study of 242 patients with non-Hodgkin lymphoma found that those with diabetes had a 20-fold increased mortality risk compared with those without diabetes [43]. The variable effect size reported in these studies and ours is likely related to heterogeneity of the studies in study design, cohort size and the adjusted confounders. Results from this study and others highlight diabetes as a potential adverse prognostic indicator for haematological malignancies. Given that type 2 diabetes may be preventable by lifestyle factors, lifestyle modification with diet and exercise should be encouraged and treatment should be optimised. Further research is required to evaluate whether severity of diabetes further promotes the risk and adverse prognosis of haematological malignancies, and whether particular glucose-lowering medications may influence these associations.
Our study has several limitations. As in all observational studies, there is a risk of misclassification and selection bias. We aimed to minimise these biases with validated database definitions for diabetes and evaluated the potential for detection bias through cancer and sensitivity analysis. We did not have access to important potential risk factors such as BMI, family history, dietary and lifestyle choices or laboratory data such as HbA1c to ascertain severity of diabetes. We also did not have access to medications received for diabetes treatment and could not adjust for its impact on development of haematological malignancy. Haematological malignancy-related factors such as stage, remission status, recurrence and malignancy treatment regimens received were also not available. Glucose-lowering medications were not ascertained in this study and may influence our outcomes. The exact time of onset of diabetes or haematological malignancy could not be determined through administrative databases, as we are only able to access the time of established diagnosis. Finally, our observational study sought to evaluate the association of diabetes with haematological malignancies, and as such we cannot establish causality based on these findings.
Despite these limitations, our study has several strengths. To the best of our knowledge, our study is one of the largest contemporary population-based cohort studies to examine the association between diabetes and haematological malignancies, as well as the impact of diabetes on mortality risk. Our study used population-based data increasing the generalisability of our findings. We also had a large sample size of over 3 million and over 30,000 cancer cases, which provided the power to examine haematological cancer subtypes and impact on cancer-specific mortality. We also adjusted for several important risk factors for haematological malignancies that were not included in prior studies. We followed all individuals from the time of diabetes diagnosis, allowing for evaluation of a homogenous population to study our outcomes.
Conclusions
In this study of over 1 million adults with diabetes, we demonstrated a small but significant association between diabetes and haematological malignancy, as well as all-cause and cancer-specific mortality. Future studies to evaluate the independent risk associated with diabetes beyond BMI, severity of diabetes, malignancy stage and glucose-lowering medications should be conducted to further characterise the relationship between diabetes and haematological malignancies. Greater efforts for lifestyle modification may not only reduce diabetes burden and its complications but may also potentially lower risk of malignancy and mortality.
Data availability
The dataset from this study is held securely in coded form at ICES. While data sharing agreements prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS. The full dataset creation plan and underlying analytic code are available from the authors upon reasonable request, understanding that the programs may rely upon coding templates or macros that are unique to ICES.
Abbreviations
- CIHI:
-
Canadian Institute of Health Information
- DAD:
-
Discharge Abstract Database
- DLBCL:
-
Diffuse large B cell lymphoma
- OCR:
-
Ontario Cancer Registry
- ODD:
-
Ontario Diabetes Database
- OHIP:
-
Ontario Health Insurance Plan
- RPDB:
-
Registered Persons Database
References
Jafri H, Alsheikh-Ali AA, Karas RH (2010) Baseline and on-treatment high-density lipoprotein cholesterol and the risk of cancer in randomized controlled trials of lipid-altering therapy. J Am Coll Cardiol 55(25):2846–2854. https://doi.org/10.1016/j.jacc.2009.12.069
Scappaticcio L, Maiorino MI, Bellastella G, Giugliano D, Esposito K (2017) Insights into the relationships between diabetes, prediabetes, and cancer. Endocrine 56(2):231–239. https://doi.org/10.1007/s12020-016-1216-y
Steele CB, Thomas CC, Henley SJ et al (2017) Vital signs: trends in incidence of cancers associated with overweight and obesity - United States, 2005-2014. MMWR Morb Mortal Wkly Rep 66(39):1052–1058. https://doi.org/10.15585/mmwr.mm6639e1
Noto H, Tsujimoto T, Sasazuki T, Noda M (2011) Significantly increased risk of cancer in patients with diabetes mellitus: a systematic review and meta-analysis. Endocr Pract 17(4):616–628. https://doi.org/10.4158/EP10357.RA
Lega IC, Wilton AS, Austin PC, Fischer HD, Johnson JA, Lipscombe LL (2016) The temporal relationship between diabetes and cancer: a population-based study. Cancer 122(17):2731–2738. https://doi.org/10.1002/cncr.30095
Tsilidis KK, Kasimis JC, Lopez DS, Ntzani EE, Ioannidis JP (2015) Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ 350:g7607. https://doi.org/10.1136/bmj.g7607
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70(1):7–30. https://doi.org/10.3322/caac.21590
Moutschen MP, Scheen AJ, Lefebvre PJ (1992) Impaired immune responses in diabetes mellitus: analysis of the factors and mechanisms involved. Relevance to the increased susceptibility of diabetic patients to specific infections. Diabetes Metab 18(3):187–201
Engels EA, Cerhan JR, Linet MS et al (2005) Immune-related conditions and immune-modulating medications as risk factors for non-Hodgkin’s lymphoma: a case-control study. Am J Epidemiol 162(12):1153–1161. https://doi.org/10.1093/aje/kwi341
Smedby KE, Hjalgrim H, Askling J et al (2006) Autoimmune and chronic inflammatory disorders and risk of non-Hodgkin lymphoma by subtype. J Natl Cancer Inst 98(1):51–60. https://doi.org/10.1093/jnci/djj004
Birmann BM, Neuhouser ML, Rosner B et al (2012) Prediagnosis biomarkers of insulin-like growth factor-1, insulin, and interleukin-6 dysregulation and multiple myeloma risk in the Multiple Myeloma Cohort Consortium. Blood 120(25):4929–4937. https://doi.org/10.1182/blood-2012-03-417253
Chao C, Page JH (2008) Type 2 diabetes mellitus and risk of non-Hodgkin lymphoma: a systematic review and meta-analysis. Am J Epidemiol 168(5):471–480. https://doi.org/10.1093/aje/kwn160
Mitri J, Castillo J, Pittas AG (2008) Diabetes and risk of non-Hodgkin’s lymphoma: a meta-analysis of observational studies. Diabetes Care 31(12):2391–2397. https://doi.org/10.2337/dc08-1034
Tseng CH (2012) Diabetes, insulin use, and non-Hodgkin lymphoma mortality in Taiwan. Metabolism 61(7):1003–1009. https://doi.org/10.1016/j.metabol.2011.11.015
Tseng CH (2019) Metformin is associated with a lower risk of non-Hodgkin lymphoma in patients with type 2 diabetes. Diabetes Metab 45(5):458–464. https://doi.org/10.1016/j.diabet.2019.05.002
Wu W, Merriman K, Nabaah A et al (2014) The association of diabetes and anti-diabetic medications with clinical outcomes in multiple myeloma. Br J Cancer 111(3):628–636. https://doi.org/10.1038/bjc.2014.307
Lipscombe LL, Hwee J, Webster L, Shah BR, Booth GL, Tu K (2018) Identifying diabetes cases from administrative data: a population-based validation study. BMC Health Serv Res 18(1):316. https://doi.org/10.1186/s12913-018-3148-0
Holowaty EJ, Norwood TA, Wanigaratne S, Abellan JJ, Beale L (2010) Feasibility and utility of mapping disease risk at the neighbourhood level within a Canadian public health unit: an ecological study. Int J Health Geogr 9:21. https://doi.org/10.1186/1476-072X-9-21
McLaughlin JR, Kreiger N, Marrett LD, Holowaty EJ (1991) Cancer incidence registration and trends in Ontario. Eur J Cancer 27(11):1520–1524. https://doi.org/10.1016/0277-5379(91)90041-b
Swerdlow SH, Campo E, Harris NL et al (2008) WHO classification of tumours of haematopoietic and lymphoid tissues. IARC Publications
Castillo JJ, Mull N, Reagan JL, Nemr S, Mitri J (2012) Increased incidence of non-Hodgkin lymphoma, leukemia, and myeloma in patients with diabetes mellitus type 2: a meta-analysis of observational studies. Blood 119(21):4845–4850. https://doi.org/10.1182/blood-2011-06-362830
Clark AM, Raine K, Raphael D (2004) The American Cancer Society, American Diabetes Association, and American Heart Association joint statement on preventing cancer, cardiovascular disease, and diabetes: where are the social determinants? Diabetes Care 27(12):3024. https://doi.org/10.2337/diacare.27.12.3024
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371(9612):569–578. https://doi.org/10.1016/S0140-6736(08)60269-X
Morton LM, Turner JJ, Cerhan JR et al (2007) Proposed classification of lymphoid neoplasms for epidemiologic research from the Pathology Working Group of the International Lymphoma Epidemiology Consortium (InterLymph). Blood 110(2):695–708. https://doi.org/10.1182/blood-2006-11-051672
Castillo JJ, Ingham RR, Reagan JL, Furman M, Dalia S, Mitri J (2014) Obesity is associated with increased relative risk of diffuse large B-cell lymphoma: a meta-analysis of observational studies. Clin Lymphoma Myeloma Leuk 14(2):122–130. https://doi.org/10.1016/j.clml.2013.10.005
Pearson-Stuttard J, Zhou B, Kontis V, Bentham J, Gunter MJ, Ezzati M (2018) Worldwide burden of cancer attributable to diabetes and high body-mass index: a comparative risk assessment. Lancet Diabetes Endocrinol 6(2):95–104. https://doi.org/10.1016/S2213-8587(17)30366-2
Taylor J, Xiao W, Abdel-Wahab O (2017) Diagnosis and classification of hematologic malignancies on the basis of genetics. Blood 130(4):410–423. https://doi.org/10.1182/blood-2017-02-734541
Chang S-H, Luo S, O’Brian KK et al (2015) Association between metformin use and progression of monoclonal gammopathy of undetermined significance to multiple myeloma in US veterans with diabetes mellitus: a population-based retrospective cohort study. Lancet Haematol 2(1):e30–e36. https://doi.org/10.1016/s2352-3026(14)00037-4
Currie CJ, Poole CD, Gale EA (2009) The influence of glucose-lowering therapies on cancer risk in type 2 diabetes. Diabetologia 52(9):1766–1777. https://doi.org/10.1007/s00125-009-1440-6
Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD (2005) Metformin and reduced risk of cancer in diabetic patients. BMJ 330(7503):1304–1305. https://doi.org/10.1136/bmj.38415.708634.F7
Libby G, Donnelly LA, Donnan PT, Alessi DR, Morris AD, Evans JM (2009) New users of metformin are at low risk of incident cancer: a cohort study among people with type 2 diabetes. Diabetes Care 32(9):1620–1625. https://doi.org/10.2337/dc08-2175
de Jong R, Burden AM, de Kort S et al (2017) Impact of detection bias on the risk of gastrointestinal cancer and its subsites in type 2 diabetes mellitus. Eur J Cancer 79:61–71. https://doi.org/10.1016/j.ejca.2017.03.039
Harding JL, Shaw JE, Peeters A, Cartensen B, Magliano DJ (2015) Cancer risk among people with type 1 and type 2 diabetes: disentangling true associations, detection bias, and reverse causation. Diabetes Care 38(2):264–270. https://doi.org/10.2337/dc14-1996
Lega IC, Lipscombe LL (2019) Review: diabetes, obesity and cancer - pathophysiology and clinical implications. Endocr Rev. https://doi.org/10.1210/endrev/bnz014
Carstensen B, Witte DR, Friis S (2012) Cancer occurrence in Danish diabetic patients: duration and insulin effects. Diabetologia 55(4):948–958. https://doi.org/10.1007/s00125-011-2381-4
Johnson JA, Bowker SL, Richardson K, Marra CA (2011) Time-varying incidence of cancer after the onset of type 2 diabetes: evidence of potential detection bias. Diabetologia 54(9):2263–2271. https://doi.org/10.1007/s00125-011-2242-1
de L II, van der Klift M, de Laet CE, van Daele PL, Hofman A, Pols HA (2005) Bone mineral density and fracture risk in type-2 diabetes mellitus: the Rotterdam Study. Osteoporos Int 16(12):1713–1720. https://doi.org/10.1007/s00198-005-1909-1
Rao Kondapally Seshasai S, Kaptoge S, Thompson A et al (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364(9):829–841. https://doi.org/10.1056/NEJMoa1008862
Srokowski TP, Fang S, Hortobagyi GN, Giordano SH (2009) Impact of diabetes mellitus on complications and outcomes of adjuvant chemotherapy in older patients with breast cancer. J Clin Oncol 27(13):2170–2176. https://doi.org/10.1200/JCO.2008.17.5935
Luo J, Hendryx M, Virnig B et al (2015) Pre-existing diabetes and breast cancer prognosis among elderly women. Br J Cancer 113(5):827–832. https://doi.org/10.1038/bjc.2015.249
Stein KB, Snyder CF, Barone BB et al (2010) Colorectal cancer outcomes, recurrence, and complications in persons with and without diabetes mellitus: a systematic review and meta-analysis. Dig Dis Sci 55(7):1839–1851. https://doi.org/10.1007/s10620-009-0944-8
Qiang JK, Sutradhar R, Giannakeas V, Bhatia D, Singh S, Lipscombe LL (2020) Impact of diabetes on colorectal cancer stage and mortality risk: a population-based cohort study. Diabetologia 63(5):944–953. https://doi.org/10.1007/s00125-020-05094-8
Lin SY, Hsieh MS, Chen LS, Chiu YH, Yen AM, Chen TH (2007) Diabetes mellitus associated with the occurrence and prognosis of non-Hodgkin’s lymphoma. Eur J Cancer Prev 16(5):471–478. https://doi.org/10.1097/01.cej.0000236253.93984.8f
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
LLL is supported by Diabetes Investigator Award by Diabetes Canada. This study was supported by ICES (formerly the Institute for Clinical Evaluative Sciences), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The funder had no role in the design of the study, in the collection, analysis and interpretation of the data, or in writing the manuscript. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI) and Cancer Care Ontario (CCO). The opinions, analyses, results, conclusions and statements reported in this manuscript are those of the authors and are independent from the funding and data/information sources. No endorsements by ICES, the Ontario MOHLTC, CIHI or CCO are intended or should be inferred.
Author information
Authors and Affiliations
Contributions
All authors fulfil the following criteria: (1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published. IYG and LLL drafted the manuscript. LLL is the guarantor of this work.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM
(PDF 125 kb)
Rights and permissions
About this article
Cite this article
Gong, I.Y., Cheung, M.C., Read, S. et al. Association between diabetes and haematological malignancies: a population-based study. Diabetologia 64, 540–551 (2021). https://doi.org/10.1007/s00125-020-05338-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-020-05338-7