Abstract
Aims/hypothesis
The prognostic importance of the ankle–brachial index (ABI) in individuals with diabetes is controversial. We aimed to evaluate the relationship between the ABI and the occurrence of micro- and macrovascular complications in individuals with type 2 diabetes.
Methods
The ABI was measured at baseline in 668 individuals with type 2 diabetes, and the individuals were followed-up for a median of 10 years. Multivariate Cox analysis was used to examine associations between the ABI and the occurrence of microvascular (retinopathy, microalbuminuria, renal function deterioration and peripheral neuropathy) and macrovascular (total cardiovascular events, major adverse cardiovascular events [MACE] and cardiovascular mortality) complications, and all-cause mortality. The improvement in risk stratification was assessed using the C statistic and the integrated discrimination improvement (IDI) index.
Results
During follow-up, 168 individuals had a cardiovascular event (140 MACE) and 191 individuals died (92 cardiovascular deaths); 156 individuals newly developed or experienced worsening diabetic retinopathy, 194 achieved the renal composite outcome (122 with newly developed microalbuminuria and 93 with deteriorating renal function) and 95 newly developed or experienced worsening peripheral neuropathy. The ABI, either analysed as a continuous or as a categorical variable, was significantly associated with all macrovascular and mortality outcomes, except for non-cardiovascular mortality. Individuals with a baseline ABI of ≤0.90 had a 2.1-fold increased risk of all-cause mortality (95% CI 1.3, 3.5; p = 0.004), a 2.7-fold excess risk of cardiovascular mortality (95% CI 1.4, 5.4; p = 0.004) and a 2.5-fold increased risk of MACE (95% CI 1.5, 4.4; p = 0.001). The ABI improved risk discrimination over classical risk factors, with relative IDIs ranging from 6.3% (for all-cause mortality) to 31% (for cardiovascular mortality). In addition, an ABI of ≤0.90 was associated with the development or worsening of peripheral neuropathy (2.1-fold increased risk [95% CI 1.1, 4.3]; p = 0.033), but not with retinopathy or renal outcomes.
Conclusions/interpretation
A low ABI is associated with excess risk of adverse cardiovascular outcomes, mortality and peripheral neuropathy development or worsening, and improves cardiovascular risk stratification. The ABI should therefore be routinely evaluated in individuals with type 2 diabetes.
Similar content being viewed by others

Introduction
The ankle–brachial index (ABI), defined as the ratio between systolic BP (SBP) measured at the tibial and brachial arteries, is the most widely used method to detect asymptomatic peripheral artery disease (PAD), with a generally accepted cut-off value of ≤0.90 [1]. Most importantly, the ABI has been consistently demonstrated to predict cardiovascular prognosis in population-based studies [2,3,4,5,6], and it may be capable of improving cardiovascular risk stratification over and above traditional cardiovascular risk factors [3, 7]. Indeed, ABI measurement has been recommended for individuals at moderate or high cardiovascular risk, such as the elderly or those with cardiovascular risk factors [1], although its general usefulness as a screening method in asymptomatic individuals is still undetermined [7, 8].
Despite this, the prognostic importance of the ABI in individuals with type 2 diabetes is controversial, mainly because the presence of characteristic medial-wall calcifications of the leg arteries might augment arterial stiffness and falsely increase ABI values [9, 10]. Indeed, some previous studies have demonstrated a lack of prognostic value for the ABI in diabetic individuals in contrast to non-diabetic individuals [11,12,13], although others have reported similar positive predictive performances in diabetic and non-diabetic individuals [14,15,16,17]. Similarly, conflicting results regarding the prognostic value of the ABI have been reported by cohort studies comprised exclusively of individuals with type 2 diabetes, with some studies negating [18, 19] and others demonstrating [20,21,22,23,24,25,26,27,28] its importance. Moreover, some of the positive studies [24, 25, 27, 28] assessed whether the ABI, beyond being a risk marker, was also capable of improving risk stratification for adverse outcomes, with contradictory findings. This is a fundamental step before more widespread use of the ABI in the clinical management of type 2 diabetes can be recommended. Currently, the ADA only recommends ABI measurement in individuals with symptoms (intermittent claudication) or signs (decreased pedal pulses) of PAD [29]. Finally, as far as we know, no previous studies have addressed the importance of the ABI as a risk marker for future microvascular complications, except for foot ulceration/amputation, although several cross-sectional analyses have reported associations between a reduced ABI and the prevalence of microvascular complications [30,31,32,33].
Therefore, the prespecified aim of this study, conducted within the Rio de Janeiro Type 2 Diabetes Cohort Study (RIO-T2D), an ongoing prospective cohort study of high cardiovascular risk individuals with type 2 diabetes followed for a median of 10 years, was to evaluate the prognostic value of the ABI for the occurrence of separate microvascular (retinopathy, microalbuminuria, renal function deterioration and peripheral neuropathy) and macrovascular (total cardiovascular events [CVEs], major CVEs [MACE] and cardiovascular mortality) complications, and of all-cause mortality; and to assess whether the ABI is able to improve risk stratification beyond traditional risk factors.
Methods
Participants and baseline procedures
This was a prospective study, the RIO-T2D, with 668 individuals with type 2 diabetes enrolled between August 2004 and December 2008 and followed until December 2017 in the diabetes outpatient clinic of our tertiary-care university hospital. All participants gave written informed consent, and the local ethics committee had previously approved the study protocol. The characteristics of this cohort, baseline procedures and diagnostic definitions have been detailed elsewhere [34,35,36,37]. In brief, inclusion criteria were adults with type 2 diabetes, up to 80 years old, with any microvascular or macrovascular complication, or with at least two other modifiable cardiovascular risk factors. Exclusion criteria were morbid obesity, advanced renal failure (serum creatinine >180 μmol/l or eGFR <30 ml min−1 [1.73 m]−2) or the presence of any serious concomitant disease limiting life expectancy. For this specific analysis, individuals with clinical PAD, defined by a history of typical intermittent claudication, limb revascularisation procedures, foot ulceration or lower-extremity amputations, were excluded.
All participants were submitted to a standard baseline protocol that included a thorough clinical examination (including ABI measurement), laboratory evaluation and 24 h ambulatory BP monitoring. Diagnostic criteria for diabetes-related chronic complications have been detailed previously [34,35,36,37]. In brief, coronary heart disease was diagnosed by clinical and electrocardiographic criteria, or by positive ischaemic stress tests; and cerebrovascular disease by history and physical examination. A diagnosis of nephropathy needed at least two albuminuria measurements of at least 30 mg/24 h or a confirmed reduction in the GFR (eGFR ≤60 ml min−1 [1.73 m]−2 or serum creatinine >130 μmol/l). Peripheral neuropathy was determined by clinical examination (knee and ankle reflex activities, and foot sensation using the Semmes–Weinstein monofilament, vibration with a 128 Hz tuning fork and pinprick and temperature sensations) and neuropathic symptoms were assessed using a standard validated questionnaire [35]. Clinic BP was measured three times using a digital oscillometric BP monitor (HEM-907XL, Omron Healthcare, Kyoto, Japan) with a suitably sized cuff on two occasions 2 weeks apart at study entry. The first measure of each visit was discarded and the BP used was the mean of the last two readings from each visit. Arterial hypertension was diagnosed if mean SBP was 140 mmHg or higher or diastolic BP (DBP) was 90 mmHg or higher, or if anti-hypertensive drugs had been prescribed. Ambulatory BP monitoring was conducted in the following month using Mobil-O-Graph version 12 (Dyna Mapa, Cardios, Sao Paulo, Brazil), and average 24 h SBP and DBP values were registered [36, 37]. Laboratory evaluations included fasting glycaemia, HbA1c, serum creatinine and lipids. Albuminuria was evaluated in two non-consecutive sterile 24 h urine collections.
ABI measurement
After resting supine for at least 5 min, two BP readings were taken sequentially from each brachial and posterior tibial artery (total of eight measurements: four brachial and four tibial) using the same digital oscillometric BP monitor (HEM-907XL, Omron Healthcare) and were validated for ABI measurement [38, 39]. The ABI was calculated as the lowest tibial BP in either leg divided by the highest brachial BP in either arm [40]. An ABI value of ≤0.90 was considered indicative of PAD. All ABI measurements were performed at baseline by a single independent examiner who was unaware of other clinical data.
Follow-up and outcomes assessment
The participants were followed regularly at least three times a year until December 2017 under standardised treatment. The observation period for each individual was the number of months from the date of the first clinical examination to the date of the last clinic visit in 2017 or the date of the first endpoint, whichever came first. The primary endpoints were the occurrence of any micro- or macrovascular outcomes. Macrovascular outcomes were total CVEs (fatal or non-fatal myocardial infarction, sudden cardiac death, new-onset heart failure, death from progressive heart failure, any myocardial revascularisation procedure, fatal or non-fatal stroke, any aortic or lower-limb revascularisation procedure, any amputation above the ankle and death from aortic disease or PAD), MACE (non-fatal myocardial infarction and stroke, plus all cardiovascular deaths) and all-cause and cardiovascular mortality [34]. Microvascular outcomes were retinopathy development or worsening [36], renal outcomes [37] (new microalbuminuria development, new renal function deterioration [defined as doubling of serum creatinine to a value of ≥200 μmol/l, end-stage renal failure needing dialysis or death from renal failure] and a composite of the two) and peripheral neuropathy development or worsening [35]. Retinopathy and renal outcomes were evaluated by annual examinations [36, 37], whereas peripheral neuropathy was evaluated during a second specific examination performed after a median of 6 years from the baseline examination [35]. Peripheral neuropathy development or worsening was determined by a combination of signs (assessed using the Neuropathy Disability Score) and symptoms (assessed using the Neuropathy Symptom Score), as previously defined [35]. The presence and severity of retinopathy was determined by a single retinal specialist, following the International Clinical Diabetic Retinopathy and Diabetic Macular Edema Disease grading [41].
Statistical analyses
Continuous data are described as means ± SD or as medians (interquartile range [IQR]). The baseline characteristics of individuals with an ABI of ≤0.90 and >0.90 were compared using unpaired t tests, Mann–Whitney U tests or χ2 tests, where appropriate. Kaplan–Meier curves of the incidence of cumulative endpoints during follow-up, compared with log-rank tests, were used to assess different incidences of outcomes between individuals with ABI values of ≤0.90 and >0.90. To assess the prognostic value of the ABI for each macro- and microvascular outcome, except for peripheral neuropathy, a time-to-event Cox analysis was undertaken. First, analyses were only adjusted for age and sex, and then further adjusted for other potential confounders and risk factors (diabetes duration, BMI, smoking, physical activity, diabetes treatment, arterial hypertension, number and classes of anti-hypertensive drugs in use, ambulatory 24 h SBP, presence of micro- and macrovascular complications at baseline, serum mean first-year HbA1c, HDL- and LDL-cholesterol levels, and use of statins and aspirin). Information on all of these covariates was obtained at baseline, except for HbA1c and HDL- and LDL-cholesterol, for which mean values obtained during the first year of follow-up were used. These results are presented as HRs with their 95% CIs. For peripheral neuropathy analyses, a multiple logistic regression model was used with the same statistical adjustments, except that height (instead of BMI) and the interval between the baseline and second neuropathy evaluations were included as adjusting covariates. These results are reported as ORs with their respective 95% CIs. In both analyses, the ABI was assessed as a continuous variable (with risks estimated for a 0.10 decrement in the ABI) and also as a categorical variable (with risks estimated for individuals with an ABI of ≤0.90 in relation to those with an ABI of >0.90). In separate analyses, individuals were further divided into three ABI subgroups (≤0.90, 0.91–1.00 and ≥1.01–<1.3), with the subgroup with ABI ≥1.01 considered as the reference.
To assess the improvement in discrimination performance after the addition of the ABI to the models, we used the C statistic (analogous to the area under the receiver operating characteristic curve applied to time-to-event analysis), compared by the method proposed by DeLong and colleagues [42] and the integrated discrimination improvement (IDI) index [43, 44]. The IDI is equivalent to the difference in discrimination slopes between models with and without the new variable, and its calculation is based on continuous differences in predicted risk in new and old models for individual participants with and without the outcome under study. Thus, the IDI is free from the dependence on empirical risk categories that is inherent to reclassification tables and can be used as an objective indicator of reclassification improvement. Both the absolute and the relative IDI were calculated. The relative IDI, reported as a percentage, facilitates interpretation of the IDI, and is defined as the increase in discrimination slope divided by the slope of the standard model including only traditional cardiovascular risk factors [43, 44]. In sensitivity and interaction analyses, interactions between the ABI and age (<65 vs ≥65 years), sex, diabetes duration (<10 vs ≥10 years), presence of micro- and macrovascular complications at baseline and glycaemic control (mean HbA1c <58.5 vs ≥58.5 mmol/mol; <7.5% vs ≥7.5%) were tested for all endpoints and whenever there was evidence of interaction (p < 0.10 for interaction term), the interaction term was kept within the whole model analysis and a further stratified analysis for that specific characteristic was performed. In addition, separate analyses were performed for each outcome after excluding those participants with this specific complication at baseline.
Finally, to determine the presence of possible reverse causality between the ABI and outcomes, separate analyses were performed excluding 35 individuals who had any of the endpoints (death or non-fatal CVEs) during the first 2 years of follow-up. Statistical analyses were performed using SPSS version 19.0 (SPSS, Chicago, IL., USA) and R version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria), and a two-tailed p value of <0.05 was considered significant.
Results
Baseline characteristics according to ABI value
The mean ± SD ABI was 0.98 ± 0.19 and the median was 1.02 (IQR 0.92–1.11). A total of 156 participants (23.4%) had an ABI of ≤0.90 and only one individual had an ABI of ≥1.30 (meaning non-compressible arteries); this individual was excluded from further analyses. Table 1 outlines the baseline characteristics of the entire cohort of 668 participants and of those divided according to an ABI >0.90 or ≤0.90. Individuals with an ABI of ≤0.90 were older, had a longer duration of diabetes and lower BMI, were more frequently current or past smokers and had higher prevalences of all micro- and macrovascular diabetic complications than those with an ABI of >0.9. They also had a higher prevalence of dyslipidaemia and more participants used statins, but had comparable serum lipid levels, except for a marginally higher LDL-cholesterol level, than those with an ABI of >0.9. Regarding BP levels, individuals with an ABI of ≤0.90 had a higher prevalence of arterial hypertension, used more anti-hypertensive medications, particularly diuretics and calcium-channel blockers, and had higher clinic and ambulatory SBP but equal DBP levels, compared with their counterparts with an ABI of >0.9. Regarding glycaemic control, fewer individuals with an ABI of ≤0.90 used metformin (because of the higher prevalence of reduced renal function), but HbA1c and fasting glycaemia levels were similar between the two groups.
Endpoints occurrence during follow-up
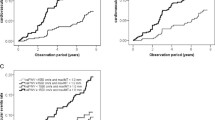
During a median follow-up of 10 years (IQR 5.7–11.7 years, maximum 13.3 years), 168 CVEs occurred (140 MACE) and 191 individuals died (92 from cardiovascular diseases); 156 individuals newly developed or experienced worsening diabetic retinopathy, 194 achieved the renal composite endpoint (122 with newly developed microalbuminuria and 93 with deteriorating renal function) and 95 newly developed or experienced worsening peripheral neuropathy. Table 1 shows the crude incidence rate for each of the outcomes in individuals with ABI values of ≤0.90 and >0.90. All cardiovascular endpoints and all-cause mortality incidences were higher in individuals with an ABI of ≤0.90 than in individuals with values of >0.90. Kaplan–Meier curves of cumulative incidences over time (Fig. 1) confirmed these findings. Regarding microvascular outcomes, individuals with an ABI of ≤0.90 had a higher incidence of renal function deterioration and of peripheral neuropathy development or worsening, but not of retinopathy development/worsening or of new microalbuminuria development.
Kaplan–Meier estimates of cumulative incidence of (a) total CVEs, (b) MACE, (c) cardiovascular mortality and (d) all-cause mortality. Grey lines, follow-up in individuals with an ABI of >0.90 at baseline. Black lines, follow-up in individuals with an ABI of ≤0.90 at baseline. Logrank tests for comparisons between incidence curves showed p < 0.001 for all outcomes
Risks associated with a reduced ABI
Table 2 presents the risks associated with the ABI, analysed as a continuous and as a categorical variable, after multivariable adjustment for other potential risk factors by Cox survival analyses. The ABI, either analysed as a continuous or as a categorical variable, was significantly associated with all macrovascular and mortality outcomes, except non-cardiovascular mortality. As a continuous variable, excess risks varied from 14% (for all-cause mortality) to 26% (for cardiovascular mortality) for decrements of 0.1 in the ABI. Individuals with an ABI ≤0.90 had a 2.1- to 2.7-fold increased risk of adverse cardiovascular outcomes and mortality in contrast to those with an ABI of >0.9, after extensive statistical adjustments for other potential risk factors. Regarding microvascular outcomes, a reduced ABI, either analysed as a continuous or as a categorical variable, was associated only with peripheral neuropathy development or worsening (19% excess risk for each 0.1 decrement and 2.2-fold increased risk for ABI ≤0.90), but not of retinopathy or renal outcomes. In analyses with participants divided into three ABI subgroups (≤0.90, 0.91–1.00 and ≥1.01–<1.3), no worse prognosis for any of the outcomes was associated with the intermediary ABI subgroup (data not shown).
Evidence of an interaction (p < 0.10) was found between the ABI and age for cardiovascular and mortality outcomes. The ABI was a stronger risk marker in younger individuals (<65 years) than in older individuals. For example, younger people with an ABI of ≤0.90 had a 2.5-fold higher risk (95% CI 1.4, 4.6, p = 0.003) of having a MACE, whereas older individuals had a 1.1 increased risk (95% CI 0.6, 2.1, p = 0.76) in fully adjusted analyses (p for interaction = 0.007). No evidence of an interaction was detected for sex, diabetes duration, presence of micro- or macrovascular complications at baseline or glycaemic control—meaning that the predictive capacity of the ABI for cardiovascular and mortality prognosis was equal in men and women, individuals with a longer and shorter duration of diabetes, those with or without diabetic complications and those with good or poor glycaemic control. Excluding participants with prevalent complications at baseline did not qualitatively change the results of the macrovascular outcomes, but attenuated the associations between the ABI and peripheral neuropathy development (electronic supplementary material [ESM] Table 1). In addition, excluding those individuals who experienced any of the endpoints in the first 2 years of follow-up did not change any of the results (ESM Table 2), signifying that there was no reverse causality between a reduced ABI and cardiovascular and mortality outcomes.
Improvement in risk stratification with the ABI
Table 3 shows the results of analyses of improvement in risk stratification after adding the ABI to a standard risk factor model. According to the C statistic, addition of the ABI marginally improved risk discrimination for total CVEs, both as a categorical variable and a continuous variable (although the latter was not significant, p = 0.06). According to the IDI index, adding the ABI significantly improved risk discrimination for all macrovascular outcomes and for all-cause mortality, with improvements ranging from 6.3% (for all-cause mortality) to 31% (for cardiovascular mortality with ABI as a continuous variable). However, the ABI did not improve risk discrimination for peripheral neuropathy development or worsening during follow-up.
Discussion
This long-term (median 10 years) prospective study has three main findings with potential clinical impact. First, it demonstrated that the ABI, either analysed as a continuous or as a categorical variable, is a strong risk marker for macrovascular complications and mortality in high cardiovascular risk individuals with type 2 diabetes, particularly in younger (<65 years) individuals. Indeed, a reduced ABI (≤0.90) was associated with at least a twofold excess risk of these adverse outcomes. Second, the ABI improved risk discrimination for these outcomes over and beyond a standard risk factor model, although the magnitude of improvement might be considered rather modest. Finally, the ABI was also associated with the future development or worsening of peripheral neuropathy but did not improve risk discrimination, which was already quite high with the standard model. As a whole, our findings support the recommendation that the ABI should be more widely used in the routine clinical management of individuals with type 2 diabetes, not only in those with signs or symptoms suggesting PAD, as currently recommended.
Some previous longitudinal studies in individuals with type 2 diabetes [20,21,22,23,24,25,26,27,28] and in individuals with and without diabetes [14,15,16,17] have reported that the ABI is a risk marker for future CVE occurrence and mortality, whereas other studies have contradicted this finding [11,12,13, 18, 19]. Our findings corroborate the studies reporting positive results. The reasons for these opposing findings are not clear, but they might include differences in the studied diabetic populations (e.g. older or younger, higher or lower baseline cardiovascular risk profile), study designs (e.g. retrospective or prospective, different duration of follow-ups and definition of endpoints) or data analyses (e.g. ABI as continuous or categorical variable, or different cut-off values). Of most relevance, few previous studies [24, 25, 27, 28] have addressed whether the ABI is capable of improving risk discrimination beyond a standard risk factor model, which is an important step for recommending the routine use of the ABI in the clinical management of type 2 diabetes. However, the results of these previous studies were contradictory, with two of them showing that the ABI improved risk discrimination [25, 28] and the other two failing to demonstrate any improvement [24, 27]. The first study [24] evaluated 151 Chinese individuals with type 2 diabetes who were followed for 5 years, with 16 CVEs during follow-up. An ABI of ≤0.98 was associated with CVEs, but did not improve risk discrimination as evaluated by increase in the C statistic, although the AUC increased from 0.59 (with the Framingham risk score as the standard model) to 0.67 after adding the ABI. The second study [25] used data from the Cardiovascular Health Study (782 elderly diabetic individuals with 265 CVEs over a 10 year follow-up) and the Multi-Ethnic Study on Atherosclerosis (MESA) (843 middle-aged individuals with type 2 diabetes, who experienced 71 CVEs over a 7 year follow-up). In both cohorts, an ABI of <1.0 was associated with CVEs and improved risk discrimination, but with a modest increase in the C statistic (from 0.64 to 0.68, significant only in the Cardiovascular Health Study) and with a net reclassification improvement (similar to IDI but dependent on arbitrary risk categories) of 0.09 in MESA and 0.12 in the Cardiovascular Health Study. The third report [27] joined data from MESA and the Heinz Nixdorf Recall Study (a total of 1343 diabetic individuals with 85 coronary events over 8.5 years of follow-up). An ABI of <0.9 was associated with coronary events in Cox analysis, but it did not enter the final Bayesian risk model or improve risk discrimination. Finally, the fourth study [28] evaluated only 179 individuals with type 2 diabetes and microalbuminuria, with 40 CVEs and 26 all-cause deaths during a 6 year follow-up. The ABI, either as a continuous or categorical variable (<0.9), was associated with CVEs and mortality and improved risk discrimination with relative IDIs of 51.8% for CVEs and 53.6% for all-cause mortality, but with a non-significant C statistic increase (from 0.76 to 0.82 for CVEs). Our study advances these previous disparate findings by demonstrating that the ABI indeed improves risk discrimination for cardiovascular morbidity and mortality, with relative improvements of 9–14% for an ABI of ≤0.9, which has more clinical applicability. The finding of only modest, mostly non-significant increases in the C statistic, corroborating previous studies [24, 25, 27, 28], was expected. It has been consistently demonstrated that for standard risk factor models with fairly good discriminations (generally AUC >0.70), only very large effect sizes of the new marker on the outcome will result in a meaningfully larger AUC, which is unrealistic for most variables [43,44,45].
Despite several previous cross-sectional studies reporting associations between a reduced ABI and the presence of diabetic microvascular complications [30,31,32,33] this is, as far as we know, the first prospective study to evaluate the ABI as a marker of future development or worsening of microvascular complications. We have demonstrated that a reduced ABI is not associated with diabetic retinopathy development or worsening, diabetic kidney disease, new microalbuminuria development or renal function deterioration. However, the ABI, either evaluated as a continuous or as a categorical variable, was associated with peripheral neuropathy development or worsening, although its inclusion did not improve risk discrimination, which was already high in the standard risk model (AUC 0.78). The pathophysiological mechanisms underlying the associations between asymptomatic PAD, reflected by a reduced ABI, and peripheral neuropathy possibly involve microvascular ischaemic neuropathy or shared pathways such as insulin resistance, oxidative stress and endothelial dysfunction [33, 46]. Most importantly, the concomitance of a reduced ABI and peripheral neuropathy greatly increases the risk of foot ulceration and lower-extremity amputations [47].
The findings of the present study should be interpreted within the context of its limitations. First, this was a prospective observational cohort; hence, no causal relationships or pathophysiological inferences can be made, but only speculated upon. Moreover, as with any cohort study, residual confounding due to unmeasured or unknown factors cannot be ruled out. Second, we enrolled mainly middle-aged to elderly individuals with longstanding type 2 diabetes, who were followed in a tertiary-care university hospital. Therefore, our results might not be generalisable to younger individuals with recent-onset type 2 diabetes or who are being managed in primary care. Finally, peripheral neuropathy was not assessed annually during our follow-up, as for the other outcomes, but at two specific timepoints (at baseline and after a median of 6 years), which might have affected the evaluation of this endpoint, although this specific analysis took into account the differential time interval between neuropathy assessments. Moreover, the evaluation of this outcome was possibly affected by survival bias, as most of the participants who did not undergo the second neuropathy examination (181 out of 197 participants) did not do so because they had died. Hence, the analysis of the peripheral neuropathy outcome was mainly restricted to the survivors. Apart from these considerations, the main strength of this study is its well-documented cohort, who underwent standardised care and annual evaluations of outcomes over a long (10 year) follow-up, which allowed a comprehensive analysis of the excess risks associated with the ABI for separate micro- and macrovascular complications and for mortality in individuals with type 2 diabetes.
In conclusion, this prospective study, with a median follow-up of 10 years, provides evidence that an ABI of ≤0.90 is associated with increased risk of adverse cardiovascular outcomes, mortality, and development or worsening of peripheral neuropathy; and that the ABI improves risk discrimination for cardiovascular outcomes. Indeed, in our multivariate analyses of cardiovascular outcomes, the excess risk associated with a reduced ABI was comparable to or greater than the risk associated with pre-existing cardiovascular disease, which ranged from 1.5 to 2.0 (data not shown). However, it has been demonstrated that diabetic individuals with asymptomatic PAD are generally undertreated and poorly controlled in relation to those with coronary or cerebrovascular disease [20, 48]. Whether the prognosis of these high-risk diabetic individuals with a reduced ABI can be improved by more aggressive medical therapy [49] or by exercise training [50] should be investigated in future studies. Until then, at least annual ABI measurement should be included in the routine clinical management of individuals with type 2 diabetes for better cardiovascular risk stratification.
Data availability
The Rio de Janeiro Type 2 Diabetes Cohort Study is an ongoing study and its dataset is not publicly available to maintain the privacy of the participants. However, it may be available from the corresponding author on reasonable request.
Abbreviations
- ABI:
-
Ankle–brachial index
- CVE:
-
Cardiovascular event
- DBP:
-
Diastolic BP
- IDI:
-
Integrated discrimination improvement
- IQR:
-
Interquartile range
- MACE:
-
Major adverse cardiovascular events
- MESA:
-
Multi-Ethnic Study on Atherosclerosis
- PAD:
-
Peripheral arterial disease
- RIO-T2D:
-
Rio de Janeiro Type 2 Diabetes Cohort Study
- SBP:
-
Systolic BP
References
Gerhard-Herman MD, Gornik HL, Barrett C et al (2017) 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 69:e71–e126. https://doi.org/10.1016/j.jacc.2016.11.007
O’Hare AM, Katz R, Shlipak MG, Cushman M, Newman AB (2006) Mortality and cardiovascular risk across the ankle-arm index spectrum: results from the Cardiovascular Health Study. Circulation 113:388–393. https://doi.org/10.1161/CIRCULATIONAHA.105.570903
Ankle Brachial Index Collaboration, Fowkes FG, Murray GD, Butcher I et al (2008) Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA 300:197–208. https://doi.org/10.1001/jama.300.2.197
Diehm C, Allenberg JR, Pittrow D, German Epidemiological Trial on Ankle Brachial Index Study Group et al (2009) Mortality and vascular morbidity in older adults with asymptomatic versus symptomatic peripheral artery disease. Circulation 120:2053–2061. https://doi.org/10.1161/CIRCULATIONAHA.109.865600
Murphy TP, Dhangana R, Pencina MJ, D’Agostino RB Sr (2012) Ankle-brachial index and cardiovascular risk prediction: an analysis of 11,594 individuals with 10-year follow-up. Atherosclerosis 220:160–167. https://doi.org/10.1016/j.atherosclerosis.2011.10.037
Yeboah J, Young R, McClelland RL et al (2016) Utility of nontraditional risk markers in atherosclerotic cardiovascular disease risk assessment. J Am Coll Cardiol 67:139–147. https://doi.org/10.1016/j.jacc.2015.10.058
Lin JS, Olson CM, Johnson ES, Whitlock EP (2013) The ankle-brachial index for peripheral artery disease screening and cardiovascular disease prediction among asymptomatic adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 159:333–341. https://doi.org/10.7326/0003-4819-159-5-201309030-00007
Alahdab F, Wang AT, Elraiyah TA et al (2015) A systematic review for the screening for peripheral arterial disease in asymptomatic patients. J Vasc Surg 61(3 Suppl):42S–53S. https://doi.org/10.1016/j.jvs.2014.12.008
Potier L, Abi Khalil C, Mohammedi K, Roussel R (2011) Use and utility of ankle brachial index in patients with diabetes. Eur J Vasc Endovasc Surg 41:110–116. https://doi.org/10.1016/j.ejvs.2010.09.020
Aubert CE, Cluzel P, Kemel S et al (2014) Influence of peripheral vascular calcification on efficiency of screening tests for peripheral arterial occlusive disease in diabetes—a cross-sectional study. Diabet Med 31:192–199. https://doi.org/10.1111/dme.12309
Ogren M, Hedblad B, Engström G, Janzon L (2005) Prevalence and prognostic significance of asymptomatic peripheral arterial disease in 68-year-old men with diabetes. Results from the population study ‘Men born in 1914’ from Malmö, Sweden. Eur J Vasc Endovasc Surg 29:182–189. https://doi.org/10.1016/j.ejvs.2004.11.013
Mostaza JM, Manzano L, Suarez C et al (2011) Different prognostic value of silent peripheral artery disease in type 2 diabetic and non-diabetic subjects with stable cardiovascular disease. Atherosclerosis 214:191–195. https://doi.org/10.1016/j.atherosclerosis.2010.10.020
Potier L, Roussel R, Labreuche J, REACH Investigators et al (2015) Interaction between diabetes and a high ankle-brachial index on mortality risk. Eur J Prev Cardiol 22:615–621. https://doi.org/10.1177/2047487314533621
Vogt MT, McKenna M, Wolfson SK, Kuller LH (1993) The relationship between ankle brachial index, other atherosclerotic disease, diabetes, smoking and mortality in older men and women. Atherosclerosis 101:191–202. https://doi.org/10.1016/0021-9150(93)90116-C
Leibson CL, Ransom JE, Olson W, Zimmerman BR, O’Fallon WM, Palumbo PJ (2004) Peripheral arterial disease, diabetes, and mortality. Diabetes Care 27:2843–2849. https://doi.org/10.2337/diacare.27.12.2843
Hanssen NM, Huijberts MS, Schalkwijk CG, Nijpels G, Dekker JM, Stehouwer CD (2012) Associations between the ankle-brachial index and cardiovascular and all-cause mortality are similar in individuals without and with type 2 diabetes: nineteen-year follow-up of a population-based cohort study. Diabetes Care 35:1731–1735. https://doi.org/10.2337/dc12-0178
Hendriks EJ, Westerink J, de Jong PA, SMART Study Group et al (2016) Association of high ankle brachial index with incident cardiovascular disease and mortality in a high-risk population. Arterioscler Thromb Vasc Biol 36:412–417. https://doi.org/10.1161/ATVBAHA.115.306657
Li HY, Jiang YD, Chang TJ et al (2011) Serum vascular adhesion protein-1 predicts 10-year cardiovascular and cancer mortality in individuals with type 2 diabetes. Diabetes 60:993–999. https://doi.org/10.2337/db10-0607
Gazzaruso C, Coppola A, Falcone C et al (2013) Transcutaneous oxygen tension as a potential predictor of cardiovascular events in type 2 diabetes: comparison with ankle-brachial index. Diabetes Care 36:1720–1725. https://doi.org/10.2337/dc12-1401
Norman PE, Davis WA, Bruce DG, Davis TM (2006) Peripheral arterial disease and risk of cardiac death in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care 29:575–580. https://doi.org/10.2337/diacare.29.03.06.dc05-1567
Li J, Luo Y, Xu Y et al (2007) Risk factors of peripheral arterial disease and relationship between low ankle-brachial index and mortality from all-cause and cardiovascular disease in Chinese patients with type 2 diabetes. Circ J 71:377–381. https://doi.org/10.1253/circj.71.377
Bundó M, Muñoz L, Pérez C et al (2010) Asymptomatic peripheral arterial disease in type 2 diabetes patients: a 10-year follow-up study of the utility of the ankle brachial index as a prognostic marker of cardiovascular disease. Ann Vasc Surg 24:985–993. https://doi.org/10.1016/j.avsg.2010.06.001
Abbott JD, Lombardero MS, Barsness GW et al (2012) Ankle-brachial index and cardiovascular outcomes in the Bypass Angioplasty Revascularization Investigation 2 Diabetes trial. Am Heart J 164:585–590.e4. https://doi.org/10.1016/j.ahj.2012.06.017
Lau KK, Wong YK, Chan YH et al (2012) Prognostic implications of surrogate markers of atherosclerosis in low to intermediate risk patients with type 2 diabetes. Cardiovasc Diabetol 11:101. https://doi.org/10.1186/1475-2840-11-101
Mukamal KJ, Kizer JR, Djoussé L et al (2013) Prediction and classification of cardiovascular disease risk in older adults with diabetes. Diabetologia 56:275–283. https://doi.org/10.1007/s00125-012-2772-1
Natsuaki C, Inoguchi T, Maeda Y et al (2014) Association of borderline ankle-brachial index with mortality and the incidence of peripheral artery disease in diabetic patients. Atherosclerosis 234:360–365. https://doi.org/10.1016/j.atherosclerosis.2014.03.018
Yeboah J, Erbel R, Delaney JC et al (2014) Development of a new diabetes risk prediction tool for incident coronary heart disease events: the Multi-Ethnic Study of Atherosclerosis and the Heinz Nixdorf Recall Study. Atherosclerosis 236:411–417. https://doi.org/10.1016/j.atherosclerosis.2014.07.035
Zobel EH, von Scholten BJ, Reinhard H et al (2017) Toe-brachial index as a predictor of cardiovascular disease and all-cause mortality in people with type 2 diabetes and microalbuminuria. Diabetologia 60:1883–1891. https://doi.org/10.1007/s00125-017-4344-x
American Diabetes Association (2018) 10. Microvascular complications and foot care: standards of medical care in diabetes-2018. Diabetes Care 41(Suppl 1):S105–S118. https://doi.org/10.2337/dc18-S010
Hsieh MC, Tien KJ, Perng DS et al (2009) Diabetic nephropathy and risk factors for peripheral artery disease in Chinese with type 2 diabetes mellitus. Metabolism 58:504–509. https://doi.org/10.1016/j.metabol.2008.11.008
Chen SC, Hsiao PJ, Huang JC et al (2015) Abnormally low or high ankle-brachial index is associated with proliferative diabetic retinopathy in type 2 diabetic mellitus patients. PLoS One 10:e0134718. https://doi.org/10.1371/journal.pone.0134718
Yan BP, Zhang Y, Kong AP, Hong Kong JADE Study Group et al (2015) Borderline ankle-brachial index is associated with increased prevalence of micro- and macrovascular complications in type 2 diabetes: a cross-sectional analysis of 12,772 patients from the Joint Asia Diabetes Evaluation Program. Diab Vasc Dis Res 12:334–341. https://doi.org/10.1177/1479164115590559
Salvotelli L, Stoico V, Perrone F et al (2015) Prevalence of neuropathy in type 2 diabetic patients and its association with other diabetes complications: the Verona Diabetic Foot Screening Program. J Diabetes Complicat 29:1066–1070. https://doi.org/10.1016/j.jdiacomp.2015.06.014
Cardoso CR, Leite NC, Ferreira MT, Salles GF (2015) Prognostic importance of baseline and serial glycated hemoglobin levels in high-risk patients with type 2 diabetes: the Rio de Janeiro Type 2 Diabetes Cohort Study. Acta Diabetol 52:21–29. https://doi.org/10.1007/s00592-014-0592-0
Cardoso CR, Moran CB, Marinho FS, Ferreira MT, Salles GF (2015) Increased aortic stiffness predicts future development and progression of peripheral neuropathy in patients with type 2 diabetes: the Rio de Janeiro Type 2 Diabetes Cohort Study. Diabetologia 58:2161–2168. https://doi.org/10.1007/s00125-015-3658-9
Cardoso CRL, Leite NC, Dib E, Salles GF (2017) Predictors of development and progression of retinopathy in patients with type 2 diabetes: importance of blood pressure parameters. Sci Rep 7:4867. https://doi.org/10.1038/s41598-017-05159-6
Cardoso CRL, Leite NC, Salles GC, Ferreira MT, Salles GF (2018) Aortic stiffness and ambulatory blood pressure as predictors of diabetic kidney disease: a competing risks analysis from the Rio de Janeiro Type 2 Diabetes Cohort Study. Diabetologia 61:455–465. https://doi.org/10.1007/s00125-017-4484-z
Verberk WJ, Kollias A, Stergiou GS (2012) Automated oscillometric determination of the ankle-brachial index: a systematic review and meta-analysis. Hypertens Res 35:883–891. https://doi.org/10.1038/hr.2012.83
Herráiz-Adillo Á, Cavero-Redondo I, Álvarez-Bueno C, Martínez-Vizcaíno V, Pozuelo-Carrascosa DP, Notario-Pacheco B (2017) The accuracy of an oscillometric ankle-brachial index in the diagnosis of lower limb peripheral arterial disease: a systematic review and meta-analysis. Int J Clin Pract 71:e12994. https://doi.org/10.1111/ijcp.12994
Espinola-Klein C, Rupprecht HJ, Bickel C, AtheroGene Investigators et al (2008) Different calculations of ankle-brachial index and their impact on cardiovascular risk prediction. Circulation 118:961–967. https://doi.org/10.1161/CIRCULATIONAHA.107.763227
Wilkinson CP, Ferris FL 3rd, Klein RE, Global Diabetic Retinopathy Project Group et al (2003) Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 110:1677–1682. https://doi.org/10.1016/S0161-6420(03)00475-5
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845. https://doi.org/10.2307/2531595
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27:157–172. https://doi.org/10.1002/sim.2929
Pencina MJ, D’Agostino RB Sr, Demler OV (2012) Novel metrics for evaluating improvement in discrimination: net reclassification and integrated discrimination improvement for normal variables and nested models. Stat Med 31:101–113. https://doi.org/10.1002/sim.4348
Pang CL, Pilkington N, Wei Y, Peters J, Roobottom C, Hyde C (2018) A methodology review on the incremental prognostic value of computed tomography biomarkers in addition to Framingham risk score in predicting cardiovascular disease: the use of association, discrimination and reclassification. BMC Cardiovasc Disord 18:39. https://doi.org/10.1186/s12872-018-0777-5
Barrett EJ, Liu Z, Khamaisi M et al (2017) Diabetic microvascular disease: an Endocrine Society scientific statement. J Clin Endocrinol Metab 102:4343–4410. https://doi.org/10.1210/jc.2017-01922
Davis WA, Norman PE, Bruce DG, Davis TM (2006) Predictors, consequences and costs of diabetes-related lower extremity amputation complicating type 2 diabetes: the Fremantle Diabetes Study. Diabetologia 49:2634–2641. https://doi.org/10.1007/s00125-006-0431-0
González-Clemente JM, Piniés JA, Calle-Pascual A, PADiD Study Group et al (2008) Cardiovascular risk factor management is poorer in diabetic patients with undiagnosed peripheral arterial disease than in those with known coronary heart disease or cerebrovascular disease. Results of a nationwide study in tertiary diabetes centres. Diabet Med 25:427–434. https://doi.org/10.1111/j.1464-5491.2008.02402.x
Mehler PS, Coll JR, Estacio R, Esler A, Schrier RW, Hiatt WR (2003) Intensive blood pressure control reduces the risk of cardiovascular events in patients with peripheral arterial disease and type 2 diabetes. Circulation 107:753–756. https://doi.org/10.1161/01.CIR.0000049640.46039.52
Barone Gibbs B, Dobrosielski DA, Althouse AD, Stewart KJ (2013) The effect of exercise training on ankle-brachial index in type 2 diabetes. Atherosclerosis 230:125–130. https://doi.org/10.1016/j.atherosclerosis.2013.07.002
Funding
This study was supported by grants from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, Brazil) and from the Fundação Carlos Chagas Filho de Amparo a Pesquisa do Estado do Rio de Janeiro (FAPERJ, Brazil). The sponsors had no role in the study design, data collection or analysis, or interpretation of the results, or in the preparation, review and approval of the manuscript.
Author information
Authors and Affiliations
Contributions
CRLC, NCL and GFS conceived and designed the study, followed-up the participants and obtained the data. JVM performed the ABI measurements. CRLC drafted the manuscript. GCS and GFS analysed the data and GFS is the guarantor. All authors helped interpret the results, reviewed the manuscript and approved this version to be published. GFS had full access to all of the data and takes responsibility for the integrity of the data and the accuracy of data analysis.
Corresponding author
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Electronic supplementary material
ESM
(PDF 71 kb)
Rights and permissions
About this article
Cite this article
Cardoso, C.R.L., Melo, J.V., Salles, G.C. et al. Prognostic impact of the ankle–brachial index on the development of micro- and macrovascular complications in individuals with type 2 diabetes: the Rio de Janeiro Type 2 Diabetes Cohort Study. Diabetologia 61, 2266–2276 (2018). https://doi.org/10.1007/s00125-018-4709-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4709-9