Abstract
Aims/hypothesis
Pancreatic fat accumulation may contribute to the development of beta cell dysfunction. Exercise training improves whole-body insulin sensitivity, but its effects on pancreatic fat content and beta cell dysfunction are unclear. The aim of this parallel-group randomised controlled trial was to evaluate the effects of exercise training on pancreatic fat and beta cell function in healthy and prediabetic or type 2 diabetic participants and to test whether the responses were similar regardless of baseline glucose tolerance.
Methods
Using newspaper announcements, a total of 97 sedentary 40–55-year-old individuals were assessed for eligibility. Prediabetes (impaired fasting glucose and/or impaired glucose tolerance) and type 2 diabetes were defined by ADA criteria. Of the screened candidates, 28 healthy men and 26 prediabetic or type 2 diabetic men and women met the inclusion criteria and were randomised into 2-week-long sprint interval or moderate-intensity continuous training programmes in a 1:1 allocation ratio using random permuted blocks. The primary outcome was pancreatic fat, which was measured by magnetic resonance spectroscopy. As secondary outcomes, beta cell function was studied using variables derived from OGTT, and whole-body insulin sensitivity and pancreatic fatty acid and glucose uptake were measured using positron emission tomography. The measurements were carried out at the Turku PET Centre, Finland. The analyses were based on an intention-to-treat principle. Given the nature of the intervention, blinding was not applicable.
Results
At baseline, the group of prediabetic or type 2 diabetic men had a higher pancreatic fat content and impaired beta cell function compared with the healthy men, while glucose and fatty acid uptake into the pancreas was similar. Exercise training decreased pancreatic fat similarly in healthy (from 4.4% [3.0%, 6.1%] to 3.6% [2.4%, 5.2%] [mean, 95% CI]) and prediabetic or type 2 diabetic men (from 8.7% [6.0%, 11.9%] to 6.7% [4.4%, 9.6%]; p = 0.036 for time effect) without any changes in pancreatic substrate uptake (p ≥ 0.31 for time effect in both insulin-stimulated glucose and fasting state fatty acid uptake). In prediabetic or type 2 diabetic men and women, both exercise modes similarly improved variables describing beta cell function.
Conclusions/interpretation
Two weeks of exercise training improves beta cell function in prediabetic or type 2 diabetic individuals and decreases pancreatic fat regardless of baseline glucose tolerance. This study shows that short-term training efficiently reduces ectopic fat within the pancreas, and exercise training may therefore reduce the risk of type 2 diabetes.
Trial registration
ClinicalTrials.gov NCT01344928
Funding
This study was funded by the Emil Aaltonen Foundation, the European Foundation for the Study of Diabetes, the Finnish Diabetes Foundation, the Orion Research Foundation, the Academy of Finland (grants 251399, 256470, 281440, and 283319), the Ministry of Education of the State of Finland, the Paavo Nurmi Foundation, the Novo Nordisk Foundation, the Finnish Cultural Foundation, the Hospital District of Southwest Finland, the Turku University Foundation, and the Finnish Medical Foundation.
Similar content being viewed by others

Introduction
Obesity and physical inactivity are major risk factors for type 2 diabetes mellitus. Obesity has been linked to the accumulation of ectopic fat in different organs, such as the heart, muscle, liver and pancreas [1]. Although ectopic fat in the liver and its association with metabolic disorders has been extensively studied [2], less is known about the role of fatty pancreas despite its clinical significance [3, 4]. A growing amount of evidence suggests that fatty pancreas is more frequently observed in individuals with impaired glucose tolerance [5,6,7,8,9]. Therefore, approaches to maintain a normal pancreatic fat content could reduce the risk of metabolic diseases and type 2 diabetes.
Insulin resistance and dysfunction of the pancreatic beta cells characterise type 2 diabetes and are already present before hyperglycaemia develops [10, 11]. A relationship between pancreatic fat and impaired beta cell function has been shown in some [6, 12] but not all [13,14,15] studies. A recent study showed that pancreatic fat content decreased after bariatric surgery, with normalisation of the first-phase insulin response, only in individuals with type 2 diabetes despite similar weight losses in type 2 diabetic participants and individuals with normal glucose tolerance, suggesting that fatty pancreas associates with type 2 diabetes [9]. It currently remains unclear whether pancreatic fat accumulation causes beta cell dysfunction and consequently type 2 diabetes, or whether fatty pancreas and type 2 diabetes are independent consequences of obesity [4].
Regular exercise training has a major role in the prevention of type 2 diabetes [16]. It has recently been shown that both moderate-intensity continuous training (MICT) as well as different high-intensity interval training (HIIT) regimes can improve beta cell function in insulin resistance [17,18,19,20,21]. However, the effects of exercise training on pancreatic fat content are unknown, although it has been speculated that lifestyle modifications targeted at decreasing pancreatic fat could improve glycaemic control [22].
To study the effects of short-term exercise training on the pancreas, we recruited healthy middle-aged men as well as men and women with prediabetes or type 2 diabetes. The aims of the present study were to investigate (1) whether 2 weeks of exercise training would have similar effects on pancreatic fat content and beta cell function in healthy and prediabetic or type 2 diabetic men, and (2) whether the effects of sprint interval training (SIT) and MICT would differ in prediabetic or type 2 diabetic men and women. We previously showed that 2 weeks of either SIT or MICT decreased intrathoracic fat in both healthy and prediabetic or type 2 diabetic men [23]. We therefore hypothesised that pancreatic fat would decrease by exercise training similarly in healthy and prediabetic or type 2 diabetic participants.
Methods
Study design
This study was a parallel-group randomised controlled trial conducted at Turku PET Centre (Turku, Finland) as a part of a larger study entitled The Effects of Short-time High-intensity Interval Training on Tissue Glucose and Fat Metabolism in Healthy Subjects and Patients With Type 2 Diabetes (NCT01344928). We have previously published several reports of the study focusing on different tissues [23,24,25,26,27,28,29,30,31]. The first phase of the study investigated healthy men (with measurements between March 2011 and February 2013), and the second phase involved men and women with type 2 diabetes or prediabetes (with measurements between February 2013 and October 2015). The study was conducted according to the Declaration of Helsinki, and the study protocol was approved by the ethical committee of the Hospital District of Southwest Finland, Turku (decision 95/180/2010 §228). The participants’ health status was determined by a thorough physical examination during the screening. The purpose, nature and potential risks of the study were explained verbally and in writing before individuals gave their informed consent to participate in the study.
Participants
The study was designed to investigate 40–55-year-old participants as type 2 diabetes is often diagnosed within this age range. Individuals with relatively newly diagnosed type 2 diabetes or with prediabetes (impaired fasting glucose and/or impaired glucose tolerance, based on the criteria by ADA) who could benefit from an exercise training intervention were recruited via newspaper announcements. The inclusion criteria for the healthy candidates were: male sex, age 40–55 years, BMI 18.5–30 kg/m2, normal glycaemic control verified by OGTT, and no exercise on regular basis (\( \overset{\cdot }{V}{\mathrm{O}}_{2\mathrm{peak}} \) ≤ 40 ml kg−1 min−1). For prediabetic or type 2 diabetic candidates, the inclusion criteria were the same, except: male or female sex, BMI 18.5–35 kg/m2, and impaired glucose tolerance or type 2 diabetes according to ADA criteria [32]. A candidate was excluded if he or she had a condition which could potentially endanger their health during the study or interfere with the interpretation of the results as explained in detail previously [26, 31]. Of 97 screened individuals, 28 healthy men and 26 prediabetic or type 2 diabetic individuals (16 men, ten women) fulfilled the inclusion criteria and were admitted into the study (Fig. 1). Of 26 prediabetic or type 2 diabetic individuals, the ADA criteria for type 2 diabetes [32] were met in 17 (11 men); 13 (ten men) of these were being treated with at least one type of oral hypoglycaemic agent (median duration of type 2 diabetes 4 years), whereas four individuals with type 2 diabetes (one man) had taken no previous medication for type 2 diabetes. The remaining nine prediabetic or type 2 diabetic participants (five men) met the ADA criteria for prediabetes, having impaired fasting glucose and/or impaired glucose tolerance [32].
Randomisation to the SIT and MICT groups using a 1:1 allocation ratio was performed separately for the healthy and prediabetic or type 2 diabetic participants with random permuted blocks, as previously described in detail [23, 27, 28]. Given the nature of the intervention, no blinding was used. Two healthy and five prediabetic or type 2 diabetic participants discontinued the trial (see Fig. 1 for details).
Training interventions
Training interventions consisted of six exercise sessions over 2 weeks [25, 31]. SIT consisted of 4–6 episodes of all-out cycling effort (Monark Ergomedic 894E; Monark, Vansbro, Sweden) lasting 30 s each, with a supramaximal workload, separated by 4 min of recovery. The MICT group cycled (Tunturi E85; Tunturi Fitness, Almere, the Netherlands) for 40–60 min at an intensity equalling 60% of peak workload. Training interventions are described in detail in electronic supplementary material (ESM Methods).
Outcome measures
The number of completed experiments in terms of outcome measures is summarised in Table 1. The reasons for not completing the experiments have previously been explained in detail [27, 28].
Pancreatic fat content
The primary outcome measure of the study was pancreatic fat content, which was determined by proton magnetic resonance spectroscopy (1H MRS) using a Philips Gyroscan Intera 1.5 T CV Nova Dual Scanner (Philips Medical Systems, Best, the Netherlands) with a SENSE body coil (Philips Medical Systems, Best, the Netherlands). Details of the protocol are described in ESM Methods.
Pancreatic metabolism
As secondary outcomes, pancreatic glucose and fatty acid uptake were studied by positron emission tomography (PET) after an overnight fast. Fatty acid uptake was studied in the fasted state using 14(R,S)-[18F]fluoro-6-thia-heptadecanoic acid ([18F]FTHA; 155 (SD 9) MBq) as a tracer. On a different day, glucose uptake was measured using 2-deoxy-2-[18F]fluoro-d-glucose ([18F]FDG; 157 (SD 10) MBq) during a hyperinsulinaemic–euglycaemic clamp when participants had reached a stable glucose concentration of 5.0 (±0.5) mmol/l [23, 26]. Details of PET image processing and analysis are described in ESM Methods.
Beta cell function variables, glycaemic control, and anthropometrics
Measurement of whole-body insulin-stimulated glucose uptake (M value), details of OGTT, and determination of body composition and peak exercise capacity (\( \overset{\cdot }{V}{\mathrm{O}}_{2\mathrm{peak}} \)) are described in ESM Methods. Insulin secretion rates (ISRs) were calculated from C-peptide deconvolution for every 5 min for the whole 2 h period of the OGTT [33]. Early- and late-phase ISR (ISRearly and ISRlate) were calculated as the AUC of ISR from 0 to 30 min and from 30 to 120 min, respectively. Total ISR (ISRtotal) denotes the AUC for the whole 2 h period. An index of early ISR normalised to glucose concentration (ΔISR0-30/ΔG0-30) was calculated as (ISR30-ISR0)/(glucose30-glucose0). Other beta cell function variables were derived by modelling as described by Mari et al [34] and described in detail in ESM Methods.
Statistical analysis
Sample size was calculated for the whole study (NCT01344928) based on its primary outcome, skeletal muscle glucose uptake [25, 29]. No sample size calculation was performed specifically on the outcome measures of the present study.
The normal distribution of the variables was tested using the Shapiro–Wilk test and evaluated visually. Logarithmic (log10) or square root transformations were performed when appropriate to achieve a normal distribution. Statistical analyses were performed using hierarchical mixed linear models with compound symmetry covariance structure. First, the differences between healthy and prediabetic or type 2 diabetic men were studied with the model, which included one within-factor term (time; indicating the overall mean change between baseline and measurement after the intervention), one between-factor term (diabetes mellitus; healthy and prediabetic or type 2 diabetic men) and one interaction term (time × diabetes mellitus; indicating whether mean change during the study was different between healthy and prediabetic or type 2 diabetic men). Prediabetic and type 2 diabetic women were completely excluded when comparing the effects of exercise in healthy and prediabetic or type 2 diabetic participants to avoid mixing the effects of sex and glucose intolerance. Second, differences between SIT and MICT in prediabetic or type 2 diabetic participants, including both men and women (reported in ESM Methods), were studied using a model that included within-factor time, between-factor group (SIT and MICT) and interaction terms (time × group; whether the mean change was different in the SIT and MICT groups). The analyses were carried out using the intention-to-treat principle and included all the randomised participants. Missing data points were accounted for by restricted maximum likelihood estimation within the linear mixed models. Correlations were calculated using Pearson’s correlation (Spearman’s rank correlation for non-normally distributed data). The statistical tests were performed as two-sided and the level of statistical significance was set at 0.05. The analyses were performed using SAS System, version 9.4 for Windows (SAS Institute, Cary, NC, USA).
Results
Healthy vs prediabetic or type 2 diabetic men
The effects of exercise training were first studied separately in prediabetic and type 2 diabetic men (ESM Table 1). As most of the variables changed similarly in these groups, prediabetic and type 2 diabetic men were combined into one group. Therefore, the effects of exercise training are compared between healthy and prediabetic or type 2 diabetic men.
Prediabetic or type 2 diabetic men were heavier, had more fat and had a lower exercise capacity than healthy men at baseline (Table 2). Exercise training improved \( \overset{\cdot }{V}{\mathrm{O}}_{2\mathrm{peak}} \) and M value similarly in the healthy and prediabetic or type 2 diabetic men, and gave rise to a small but statistically significant decrease in waist circumference, fat percentage, subcutaneous and visceral fat, and HbA1c in both groups (Table 2).
Pancreatic fat content was lower in healthy men than prediabetic or type 2 diabetic men at baseline (p = 0.032; Fig. 2a,b). Two weeks of exercise training decreased pancreatic fat similarly in the healthy (from 4.4% [3.0%, 6.1%] to 3.6% [2.4%, 5.2%]) and prediabetic or type 2 diabetic men (from 8.7% [6.0%, 11.9%] to 6.7% [4.4%, 9.6%], p = 0.036 for time, p = 0.52 for the interaction time × diabetes mellitus; Fig. 2b). Five healthy men had pancreatic fat content greater than 6.2%, which has been recommended as the cut-off value for normal pancreatic fat [22], whereas three prediabetic or type 2 diabetic men had pancreatic fat below 6.2% (Fig. 2a). When the men were divided into groups with low (below 6.2%) and high (above 6.2%) pancreatic fat content, exercise training decreased pancreatic fat by 31% only in those men who had fatty pancreas at baseline (p = 0.001 for the interaction time × pancreatic fat content; p < 0.001 for the time effect in men with high pancreatic fat) (Fig. 2c). In the men’s pooled baseline data, pancreatic fat correlated positively with BMI, fat percentage, visceral fat and fasting glucose concentration (Table 3).
Pancreatic fat content in healthy and prediabetic or type 2 diabetic men at baseline (a), before and after the training intervention when participants were grouped into healthy and prediabetic or type 2 diabetic men (b), and before and after the training intervention when men were grouped according to low (≤6.2%) and high (>6.2%) pancreatic fat at baseline (c). The shaded area in (a) denotes normal pancreatic fat content (≤6.2%). (b, c) Square root transformation was performed to calculate model-based means and 95% CI. Circles, healthy men; squares, prediabetic men; triangles, type 2 diabetic men; white symbols, before exercise intervention; black symbols, after exercise intervention. T2DM, type 2 diabetes mellitus. *p ≤ 0.05, ***p ≤ 0.001 for baseline difference between the groups; †p ≤ 0.05 for time effect; ‡‡‡p ≤ 0.001 time effect for men with high pancreatic fat content
Pancreatic fatty acid uptake and insulin-stimulated glucose uptake determined by PET were similar in the healthy and prediabetic or type 2 diabetic men at baseline, and remained unchanged after 2 weeks of exercise training (Table 4).
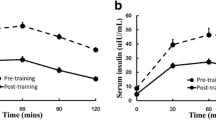
ISRbasal, ISRlate and ISRtotal were higher in prediabetic or type 2 diabetic men than healthy men at baseline, while ISRearly did not differ between the groups (Table 4, Fig. 3a). Exercise training decreased ISRbasal in prediabetic or type 2 diabetic men (p = 0.034 for the time effect in prediabetic or type 2 diabetic men), and increased ISRearly only in the healthy men (p = 0.006 for the time effect in healthy men; Fig. 3a). However, the index of early ISR normalised for glucose concentration (ΔISR0-30/ΔG0-30) decreased similarly in both groups (p = 0.010 for time). Before the intervention, ISRbasal and ISRtotal correlated positively with pancreatic fat content in the whole study population, but no correlations were found between changes in pancreatic fat and beta cell function (Table 3).
ISR (a) and potentiation (b) during 2 h OGTTs in healthy and prediabetic or type 2 diabetic men before and after the training intervention. The shaded area in (a) denotes ISRearly (0–30 min), which increased only in healthy men (p = 0.006 for the time effect in healthy men). There were non-significant differences in the potentiation of insulin secretion between prediabetic or type 2 diabetic men and healthy men (p = 0.083 for time effect for the potentiation factor ratio in prediabetic or type 2 diabetic men). White circles, healthy men before the exercise intervention; black circles, healthy men after the exercise intervention; white squares, prediabetic or type 2 diabetic men before the exercise intervention; black squares, prediabetic or type 2 diabetic men after the exercise intervention
At baseline, the potentiation factor ratio was lower in prediabetic or type 2 diabetic men than healthy men (p = 0.010). Two weeks of exercise training had a non-significantly different effect on potentiation in healthy and prediabetic or type 2 diabetic men (p = 0.086 for the interaction time × diabetes mellitus; Fig. 3b).
Pancreatic glucose sensitivity was lower in prediabetic or type 2 diabetic men than healthy men at baseline, and remained unchanged by training (Table 4). Rate sensitivity was not statistically significantly different at baseline, and it decreased similarly after training in both healthy and prediabetic or type 2 diabetic men (Table 4).
SIT vs MICT in prediabetic or type 2 diabetic men and women
The effects of exercise training did not differ between men and women (ESM Table 2), and therefore the effects of SIT and MICT were studied in the combined group of men and women with prediabetes or type 2 diabetes. As previously reported [25], SIT and MICT decreased fat percentage, abdominal fat and HbA1c to a similar extent, and increased M value, in prediabetic or type 2 diabetic participants (ESM Table 3). However, \( \overset{\cdot }{V}{\mathrm{O}}_{2\mathrm{peak}} \) improved only after SIT (ESM Table 3) [25]. Both training modes decreased pancreatic fat content in those individuals with fatty pancreas at baseline (p = 0.035 for time, p = 0.47 for the interaction time × group). The decrease in ISRbasal and ISRearly was not significant (p = 0.082 and p = 0.056 for time, respectively), and ΔISR0-30/ΔG0-30 decreased (p = 0.005 for time; ESM Table 4), after training. ISRlate and ISRtotal remained unchanged. The potentiation factor ratio increased (p = 0.030 for time) and rate sensitivity decreased (p = 0.007 for time). Except for \( \overset{\cdot }{V}{\mathrm{O}}_{2\mathrm{peak}} \), there was no difference between SIT and MICT in prediabetic or type 2 diabetic participants (ESM Tables 3 and 4). Baseline pancreatic fat content did not correlate with any of the whole-body or beta cell function variables in prediabetic or type 2 diabetic men and women (ESM Table 5).
Discussion
The present study shows for the first time that exercise training decreases pancreatic fat content regardless of baseline glucose tolerance. Both SIT and MICT reduced pancreatic fat, especially in individuals with fatty pancreas, underlining the beneficial effect of exercise training for those at risk of type 2 diabetes. Decreased pancreatic fat was not associated with changes in pancreatic metabolism or beta cell function.
At baseline, pancreatic fat content was higher in prediabetic or type 2 diabetic men than healthy men, which is consistent with previous studies [5,6,7,8], although a conflicting report also exists [35]. Whereas pancreatic fat was positively associated with BMI, body fat and visceral fat in all male participants, these associations were lost when considering only those who had prediabetes or type 2 diabetes. Furthermore, pancreatic fat correlated positively with fasting glucose, ISRbasal and ISRtotal in all men, but not in prediabetic or type 2 diabetic participants. Previous studies have reported conflicting results with regards to the association between pancreatic fat and BMI, some reporting a positive correlation [5, 7, 12, 35] and others reporting no significant correlation [6, 22]. The association between pancreatic fat and beta cell function is equally unclear. Studies addressing mainly non-diabetic individuals have reported no association between these variables [13,14,15], whereas other studies have shown that the association is different in normoglycaemic and prediabetic or type 2 diabetic individuals [6, 12]. Beta cell functional variables have been shown to have distinct patterns of decrease when spanning the range from normoglycaemic obese individuals to those with overt type 2 diabetes [36], and even beta cell defects in impaired fasting glucose and impaired glucose tolerance are different [37]. Therefore, it may be that different factors affect pancreatic fat accumulation during normoglycaemia, impaired glucose tolerance and full-blown type 2 diabetes [6, 9, 22]. These discrepancies highlight the fact that more research is needed to better understand the causes and consequences of fatty pancreas.
Just 2 weeks of exercise training decreased pancreatic fat similarly in healthy and prediabetic or type 2 diabetic men. A cross-sectional study investigating eight monozygotic young adult male twin pairs with different fitness levels reported no difference in pancreatic fat between more and less active twins [38]. However, even the healthy participants in the present study had relatively low physical fitness and high BMI, which may explain why such a short training intervention decreased pancreatic fat in the present study. Pancreatic fatty acid uptake and insulin-stimulated glucose uptake as well as fasting serum NEFA concentration were similar in healthy and prediabetic or type 2 diabetic men at baseline and remained unchanged by training. Hence, substrate uptake does not seem to explain the baseline difference between the groups or the observed decrease in pancreatic fat after exercise training. However, we measured fatty acid uptake in the fasting state, and it is possible that fat accumulation may occur during the postprandial period. A subgroup comparison between prediabetic and type 2 diabetic men (ESM Table 1) suggests that glucose uptake may be different during the progression of type 2 diabetes. Moreover, sex may also affect pancreatic metabolism (ESM Table 2). However, the small number of participants in the subgroup comparisons limits the interpretation of the findings. Further studies spanning the range from obesity to overt type 2 diabetes could shed more light on the question of whether there is a distinct pattern in pancreatic metabolism when type 2 diabetes progresses, and whether it is related to the accumulation of pancreatic fat.
When dividing the men according to low (≤6.2%) and high (>6.2%) baseline pancreatic fat content [22], exercise training decreased pancreatic fat by 31% in those men who had fatty pancreas to start with. The result that as little as 2 weeks of exercise has a marked impact on those individuals with fatty pancreas is clinically significant, as ectopic fat accumulation is recognised as a major factor in the development of type 2 diabetes [3, 4, 22].
The effects of exercise training on beta cell function have been previously studied in obese, prediabetic or type 2 diabetic individuals using a disposition index as the measure of beta cell function. Regardless of the different exercise modes (HIIT, MICT or functional high intensity training [CrossFit]) used in different studies, all have reported an increased disposition index after the training intervention, and hence inferred that training improves beta cell function [17,18,19,20,21]. However, as the disposition index may be biased [39], we studied beta cell function using several model-based variables. At baseline, ISRtotal was higher in prediabetic or type 2 diabetic men than healthy men. This reflects higher glucose levels and the reciprocal relationship between insulin sensitivity and insulin secretion, implying that reduced insulin sensitivity is compensated by increased ISR [40] until glucotoxicity becomes too great for beta cells to compensate sufficiently [41]. After exercise training, ISRbasal decreased in prediabetic or type 2 diabetic men, while ISRearly increased only in healthy men. When considering all prediabetic or type 2 diabetic participants (men and women), differences in these variables after SIT and MICT were not significant (p = 0.082 and p = 0.056 for time, respectively). On the other hand, whole-body insulin sensitivity increased similarly in both groups. The increase in ISRearly in healthy men may be a response to improved glucose sensitivity in the muscles, whereas prediabetic or type 2 diabetic individuals may compensate improved whole-body insulin sensitivity by maintaining or decreasing insulin secretion, which was already increased at baseline. A similar compensatory decrease in insulin secretion in overweight adults after training has previously been reported [21]. When normalising early ISR for glucose concentration, it decreased similarly in healthy and prediabetic or type 2 diabetic men. A corresponding decrease was observed in rate sensitivity, probably due to improved whole-body insulin sensitivity.
The potentiation of insulin secretion was impaired in prediabetic or type 2 diabetic men compared with healthy men at baseline. Our finding is in line with previous studies, which have reported blunted and delayed potentiation in diabetic individuals using a multiple meal test [42] as well as a decreased potentiation factor ratio in diabetic individuals compared with non-diabetic control participants [6]. Exercise training might normalise potentiation in prediabetic or type 2 diabetic men towards that of the healthy men (Fig. 3b; p = 0.083), suggesting that exercise training may improve the ability of beta cells to read potentiating signals, such as incretins and neural signals. However, further work is necessary to explore this.
Over the past few years, numerous studies have elucidated the effects of HIIT, or its special case SIT, in both healthy and type 2 diabetic participants, and have concluded that HIIT is at least as beneficial as the more traditional MICT in improving glycaemic control and maximal exercise capacity [43,44,45]. With regards to prediabetic or type 2 diabetic men and women in the present study, SIT and MICT had a different effect only on \( \overset{\cdot }{V}{\mathrm{O}}_{2\mathrm{peak}} \), which increased only after SIT, as discussed in our previous report [25]. The changes observed in all the other variables investigated in the present study, including increased whole-body insulin sensitivity, decreased pancreatic fat content, improved potentiation and decreased ΔISR0-30/ΔG0-30, were similar for both training modes. To conclude, both SIT and MICT can be used to improve the metabolic health of prediabetic or type 2 diabetic individuals.
The present study is not, however, without limitations. The number of participants was relatively small, although similar sample sizes have previously been used in exercise training studies with a technically demanding study design. In addition, the dropout rate was relatively high. The prediabetic or type 2 diabetic participants comprised a rather heterogeneous group containing both men and women, some with prediabetes and others with type 2 diabetes, but the number of each was too small to fully address the differences between the subgroups. It has been shown that pancreatic function differs during prediabetes and overt type 2 diabetes [36]. However, in the prediabetic and type 2 diabetic men in the present study, pancreatic function and responses to exercise were quite similar, probably because the individuals with type 2 diabetes had been relatively recently diagnosed (median duration of type 2 diabetes 4 years). Also, the oral hypoglycaemic medication taken by the participants with type 2 diabetes was interrupted for 2 days before the pre- and post-measurement PET scans. However, measuring glucose and fatty acid uptake as well as pancreatic fat content were unsuccessful in some participants (Table 1), and the heterogeneity of the prediabetic or type 2 diabetic individuals may have affected the results relating to pancreatic metabolism.
Using 1H MRS to measure pancreatic fat content cannot distinguish intracellular fat accumulation in beta cells from adipose tissue infiltration. Since pancreatic islets containing beta cells cover only around 2% of the pancreatic mass, most of the fat detected by MRS probably lies outside the islets. While the main deposition of fat in the human pancreas remains unclear, it has been suggested that 1H MRS measurement of triacylglycerols in the whole pancreas represents a surrogate marker for islet lipids [3]. In addition, individuals with type 2 diabetes have been shown to have a lower pancreatic volume than healthy individuals [46], making voxel placement more challenging. In the present study, the voxel placement within the body of pancreas was carefully ensured by axial, sagittal and coronal directions of investigation.
Finally, this study was designed to investigate the early-phase responses to exercise training. Lim et al studied the effects of dietary energy restriction in type 2 diabetes at different time points over 8 weeks, showing that although liver fat content decreased rapidly, the decrease in pancreatic fat content and improvement in beta cell function took longer to occur [47]. Therefore, the lack of association between changes in pancreatic fat content and beta cell function in the present study may be due to the short time course of the exercise intervention, and longer exercise interventions will be needed to investigate the functional effect of decreased pancreatic fat.
Conclusion
This study shows for the first time that exercise training decreases pancreatic fat content regardless of baseline glucose tolerance. In particular, individuals with fatty pancreas benefited from exercise training, with a similar decrease obtained with both SIT and MICT. As an accumulation of ectopic fat in the internal organs, including the pancreas, is a key factor in obesity and the development of type 2 diabetes, this study shows that exercise training is an effective way to decrease ectopic fat accumulation and hence reduce the risk of type 2 diabetes.
Data availability
The data are available on reasonable request from the corresponding author.
Abbreviations
- HIIT:
-
High-intensity interval training
- ISR:
-
Insulin secretion rate
- MICT:
-
Moderate-intensity continuous training
- MRS:
-
Magnetic resonance spectroscopy
- M value:
-
Whole-body insulin-stimulated glucose uptake
- PET:
-
Positron emission tomography
- SIT:
-
Sprint interval training
References
van Herpen NA, Schrauwen-Hinderling VB (2008) Lipid accumulation in non-adipose tissue and lipotoxicity. Physiol Behav 94:231–241
Yki-Järvinen H (2014) Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol 2:901–910
Guglielmi V, Sbraccia P (2017) Type 2 diabetes: does pancreatic fat really matter? Diabetes Metab Res Rev. https://doi.org/10.1002/dmrr.2955
Catanzaro R, Cuffari B, Italia A, Marotta F (2016) Exploring the metabolic syndrome: nonalcoholic fatty pancreas disease. World J Gastroenterol 22:7660–7675
Heber SD, Hetterich H, Lorbeer R et al (2017) Pancreatic fat content by magnetic resonance imaging in subjects with prediabetes, diabetes, and controls from a general population without cardiovascular disease. PLoS One 12:1–13
Tushuizen ME, Bunck MC, Pouwels PJ et al (2007) Pancreatic fat content and beta-cell function in men with and without type 2 diabetes. Diabetes 30:2916–2921
Gaborit B, Abdesselam I, Kober F et al (2015) Ectopic fat storage in the pancreas using 1H-MRS: importance of diabetic status and modulation with bariatric surgery-induced weight loss. Int J Obes 39:480–487
Dong Z, Luo Y, Cai H et al (2016) Noninvasive fat quantification of the liver and pancreas may provide potential biomarkers of impaired glucose tolerance and type 2 diabetes. Med 95:e3858
Steven S, Hollingsworth KG, Small PK et al (2016) Weight Loss Decreases Excess Pancreatic Triacylglycerol Specifically in Type 2 Diabetes. Diabetes Care 39:158–165
Kahn SE, Hull RL, Utzschneider KM (2006) Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444:840–846
Kahn SE (2003) The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of Type 2 diabetes. Diabetologia 46:3–19
Heni M, Machann J, Staiger H et al (2010) Pancreatic fat is negatively associated with insulin secretion in individuals with impaired fasting glucose and/or impaired glucose tolerance: a nuclearmagnetic resonance study. Diabetes Metab Res Rev 26:200–205
Wong VW-S, Wong GL, Yeung DK et al (2014) Fatty pancreas,Insulin resistance, and β-cell function: a population study using fat-water magnetic resonance imaging. Am J Gastroenterol 109:589–597
Staaf J, Labmayr V, Paulmichl K et al (2017) Pancreatic fat is associated with metabolic syndrome and visceral fat but not beta-cell function or body mass index in pediatric obesity. Pancreas 46:358–365
Begovatz P, Koliaki C, Weber K et al (2015) Pancreatic adipose tissue infiltration, parenchymal steatosis and beta cell function in humans. Diabetologia 58:1646–1655
Colberg S, Albright A, Blissmer B et al (2010) Exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association: joint position statement. Med Sci Sports Exerc 42:2282–2303
Madsen SM, Thorup AC, Overgaard K, Jeppesen PB (2015) High intensity interval training improves glycaemic control and pancreatic β cell function of type 2 diabetes patients. PLoS One 10:1–24
Malin SK, Solomon TPJ, Blaszczak A et al (2013) Pancreatic β-cell function increases in a linear dose-response manner following exercise training in adults with prediabetes. AJP Endocrinol Metab 305:E1248–E1254
Nieuwoudt S, Fealy CE, Foucher JA et al (2017) Functional high intensity training improves pancreatic β-cell function in adults with type 2 diabetes. Am J Physiol - Endocrinol Metab 313:E314–E320
Solomon TPJ, Malin SK, Karstoft K et al (2013) Pancreatic β-cell function is a stronger predictor of changes in glycemic control after an aerobic exercise intervention than insulin sensitivity. J Clin Endocrinol Metab 98:4176–4186
Slentz CA, Tanner CJ, Bateman LA et al (2009) Effects of exercise training intensity on pancreatic β-cell function. Diabetes Care 32:1807–1811
Singh RG, Yoon HD, Poppitt SD et al (2017) Ectopic fat accumulation in the pancreas and its clinical relevance: a systematic review, meta- analysis, and meta-regression. Metabolism 69:1–13
Honkala SM, Motiani KK, Eskelinen J-J et al (2017) Exercise training reduces intrathoracic fat regardless of defective glucose tolerance. Med Sci Sport Exerc 49:1313–1322
Eskelinen J-J, Heinonen I, Löyttyniemi E et al (2015) Muscle-specific glucose and free fatty acid uptake after sprint interval and moderate-intensity training in healthy middle-aged men. J Appl Physiol 118:1172–1180
Sjöros T, Heiskanen MA, Motiani KK et al (2018) Increased insulin-stimulated glucose uptake in both leg and arm muscles after sprint interval and moderate intensity training in subjects with Type 2 Diabetes or Prediabetes. Scand J Med Sci Sport 28:77–87
Heiskanen MA, Leskinen T, Eskelinen J-J et al (2015) Different predictors of right and left ventricular metabolism in healthy middle-aged men. Front Physiol 6:389
Heiskanen MA, Leskinen T, Heinonen IH et al (2016) Right ventricular metabolic adaptations to high-intensity interval and moderate-intensity continuous training in healthy middle-aged men. Am J Physiol Heart Circ Physiol 311:H667–H675
Heiskanen MA, Sjöros TJ, Heinonen IHA et al (2017) Sprint interval training decreases left-ventricular glucose uptake compared to moderate-intensity continuous training in subjects with type 2 diabetes or prediabetes. Sci Rep 7:10531
Eskelinen J-J, Heinonen I, Löyttyniemi E et al (2016) Left-ventricular vascular and metabolic adaptations to high-intensity interval and moderate intensity continuous training: a randomized trial in healthy middle-aged men. J Physiol 594:7127–7140
Honkala SM, Johansson J, Motiani KK et al (2017) Short-term interval training alters brain glucose metabolism in subjects with insulin resistance. J Cereb Blood Flow Metab. https://doi.org/10.1177/0271678X17734998
Kiviniemi AM, Tulppo MP, Eskelinen JJ et al (2014) Cardiac autonomic function and high-intensity interval training in middle-age men. Med Sci Sports Exerc 46:1960–1967
American Diabetes Association (2015) 2. Classification and diagnosis of diabetes. Diabetes Care 38:S8–S16
Van Cauter E, Mestrez F, Sturis J, Polonsky KS (1992) Estimation of insulin secretion rates from C-peptide levels: comparison of individual and standard kinetic parameters for C-peptide clearance. Diabetes 41:368–377
Mari A, Schmitz O, Gastaldelli A et al (2002) Meal and oral glucose tests for assessment of beta-cell function: modeling analysis in normal subjects. Am J Physiol Endocrinol Metab 283:E1159–E1166
Saisho Y, Butler AE, Meier JJ et al (2007) Pancreas volumes in humans from birth to age one hundred taking into account sex, obesity, and presence of type-2 diabetes. Clin Anat 20:933–942
Ferrannini E, Gastaldelli A, Miyazaki Y et al (2005) β-cell function in subjects spanning the range from normal glucose tolerance to overt diabetes: a new analysis. J Clin Endocrinol Metab 90:493–500
Kanat M, Mari A, Norton L et al (2012) Distinct β-cell defects in impaired fasting glucose and impaired glucose tolerance. Diabetes 61:447–453
Hannukainen JC, Borra R, Linderborg K et al (2011) Liver and pancreatic fat content and metabolism in healthy monozygotic twins with discordant physical activity. J Hepatol 54:545–552
Pacini G, Mari A (2003) Methods for clinical assessment of insulin sensitivity and β-cell function. Best Pract Res Clin Endocrinol Metab 17:305–322
Kahn SE, Prigeon RL, McCulloch DK et al (1993) Quantification of the relationship between insulin sensitivity and beta-cell function in human subjects. Evidence for a hyperbolic function. Diabetes 42:1663–1672
Boland BB, Rhodes CJ, Grimsby JS (2017) The dynamic plasticity of insulin production in β-cells. Mol Metab 6:958–973
Mari A, Tura A, Gastaldelli A, Ferrannini E (2002) Assessing insulin secretion by modeling in multiple-meal tests: role of potentiation. Diabetes 51(Suppl 1):S221–S226
Milanović Z, Sporiš G, Weston M (2015) Effectiveness of High-Intensity Interval Training (HIT) and Continuous Endurance Training for VO2max Improvements: A Systematic Review and Meta-Analysis of Controlled Trials. Sport Med 45:1469–1481
Jelleyman C, Yates T, O’Donovan G et al (2015) The effects of high-intensity interval training on glucose regulation and insulin resistance: A meta-analysis. Obes Rev 16:942–961
Cassidy S, Thoma C, Houghton D, Trenell MI (2017) High-intensity interval training: a review of its impact on glucose control and cardiometabolic health. Diabetologia 60:7–23
Macauley M, Percival K, Thelwall PE et al (2015) Altered volume, morphology and composition of the pancreas in type 2 diabetes. PLoS One 10:1–14
Lim EL, Hollingsworth KG, Aribisala BS et al (2011) Reversal of type 2 diabetes: Normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54:2506–2514
Acknowledgements
The authors thank the staff of Turku PET Centre and Paavo Nurmi Centre, University of Turku, for their excellent assistance in the study.
Funding
This study was conducted within the Centre of Excellence in Cardiovascular and Metabolic Diseases, supported by the Academy of Finland, University of Turku, Turku University Hospital and Åbo Akademi University. The study was financially supported by the Emil Aaltonen Foundation, the European Foundation for the Study of Diabetes, the Finnish Diabetes Foundation, the Orion Research Foundation, the Academy of Finland (grants 251399, 256470, 281440 and 283319), the Ministry of Education of the State of Finland, the Paavo Nurmi Foundation, the Novo Nordisk Foundation, the Finnish Cultural Foundation, the Hospital District of Southwest Finland, the Turku University Foundation and the Finnish Medical Foundation.
Author information
Authors and Affiliations
Contributions
KKK and JCH designed the study. JJE, KAV, MK, KKK and JCH collected the data. KKM analysed the PET images, AM performed the beta cell modelling, and VS performed the MRS analysis. MAH, KKM and EL analysed the data, and MAH, KKM, PN and JCH interpreted data. MAH wrote the manuscript and prepared the figures. All authors critically reviewed the manuscript and approved the final version. JCH is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Electronic supplementary material
ESM
(PDF 145 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Heiskanen, M.A., Motiani, K.K., Mari, A. et al. Exercise training decreases pancreatic fat content and improves beta cell function regardless of baseline glucose tolerance: a randomised controlled trial. Diabetologia 61, 1817–1828 (2018). https://doi.org/10.1007/s00125-018-4627-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4627-x