Abstract
Purpose
The present study aims to evaluate both early and late toxicity profiles of patients receiving immediate postoperative radiotherapy (RT; adjuvant RT or additive RT) compared to salvage RT.
Methods
We evaluated 253 patients with prostate cancer treated with either immediate postoperative (adjuvant RT, n = 42; additive RT, n = 39) or salvage RT (n = 137). Thirty-five patients received salvage treatment but did not achieve a postoperative prostate specific antigen (PSA) level <0.1 ng/ml and thus were excluded from analysis.
Results
A significantly higher rate of early grade 1/2 proctitis in the immediate postoperative RT group without additional pelvic RT was observed (p = 0.02). Patients in the immediate postoperative RT group without additional pelvic RT showed significantly more early urinary tract obstructions (p = 0.003). Toxicity rates of early (<3 months) and late (3–6 months) postoperative RT were similar (p > 0.05). Baseline recovery rate of erectile dysfunction was better in patients with immediate postoperative RT without additional pelvic RT (p = 0.02; hazard ratio (HR) = 2.22, 95%-confidence interval, 95%-CI: 1.12–4.37). Recovery rate of urinary incontinence showed no significant difference in all groups (p > 0.05).
Conclusion
Patients receiving immediate postoperative RT (adjuvant or additive RT) without additional pelvic RT experience early gastrointestinal (GI) side effect proctitis and, as well as early genitourinary (GU) toxicity urinary tract obstruction more frequently than patients treated with salvage RT. Therefore, complete recovery after surgery is essential. However, we suggest basing the treatment decision on the patient’s postoperative clinical condition and evaluation of any adverse risk factors, since many studies demonstrate a clear benefit for immediate postoperative RT (adjuvant or additive RT) in terms of oncological outcome.
Zusammenfassung
Hintergrund
In der vorliegenden Auswertung werden die frühen und späten Nebenwirkungen der sofortigen postoperativen Radiotherapie (RT; adjuvante oder additive RT) mit der Salvage-RT verglichen.
Methoden
Die Autoren werteten die Daten von 253 Patienten mit Prostatakarzinom aus, welche mit sofortiger postoperativer RT behandelt wurden: n = 42 für adjuvante RT, n = 39 für additive RT, n = 137 für Salvage-RT. Die 35 mit einer Salvage-Therapie behandelten Patienten, die keinen postoperativen Nadir für das prostataspezifische Antigen (PSA) <0,1 ng/ml erreichten, wurden aus der Analyse ausgeschlossen.
Ergebnisse
Patienten mit sofortiger postoperativer RT ohne zusätzliche RT des Beckens zeigten eine signifikant höhere Rate an frühen Grad-1/2-Proktitiden (p = 0,02). Außerdem wies diese Gruppe signifikant mehr frühe obstruktive Uropathien auf (p = 0,003). Es gab keinen signifikanten Unterschied (p > 0,05) bezüglich der Nebenwirkungsprofile zwischen Patienten mit früher postoperativer RT (innerhalb <3 Monate) vs. späte postoperative RT (innerhalb von 3–6 Monaten). Die Post-RT-Rückbildungsrate der erektilen Dysfunktion war signifikant besser bei Patienten mit sofortiger postoperativer RT ohne zusätzliche RT des Beckens (p = 0,02; Hazard Ratio, HR = 2,22; 95%-Konfidenzintervall, 95%-KI: 1.12–4,37). Dagegen wies die Rückbildungsrate einer Harninkontinenz keine signifikanten Unterschiede in allen Gruppen auf (p > 0,05).
Schlussfolgerung
Bei Patienten mit sofortiger postoperativer RT (adjuvante oder additive RT) ohne zusätzliche RT des Beckens treten häufiger frühe gastrointestinale Nebenwirkungen wie Proktitis auf. Ebenso leiden sie häufiger an obstruktiven Uropathien. Eine komplette postoperative Erholung von Nebenwirkungen ist deswegen wichtig. Die Autoren empfehlen daher, die Therapieentscheidung mit Blick auf den postoperativen Zustand des Patienten und vorhandene Risikofaktoren für ein Rezidiv zu treffen, denn manche Tumorfaktoren machen eine aggressive Vorgehensweise notwendig.





Similar content being viewed by others
References
International Agency for Research on Cancer (2014) World Cancer Report 2014. International Agency for Research on Cancer, Lyon
Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, Davis M, Peters TJ, Turner EL, Martin RM, Oxley J, Robinson M, Staffurth J, Walsh E, Bollina P, Catto J, Doble A, Doherty A, Gillatt D, Kockelbergh R, Kynaston H, Paul A, Powell P, Prescott S, Rosario DJ, Rowe E, Neal DE, Protec TSG (2016) 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 375(15):1415–1424. https://doi.org/10.1056/NEJMoa1606220
Fichtner J (2000) The management of prostate cancer in patients with a rising prostate-specific antigen level. BJU Int 86(2):181–190. https://doi.org/10.1046/j.1464-410x.2000.00701.x
Bolla M, van Poppel H, Collette L, van Cangh P, Vekemans K, Da Pozzo L, de Reijke TM, Verbaeys A, Bosset J‑F, van Velthoven R, Maréchal J‑M, Scalliet P, Haustermans K, Piérart M (2005) Postoperative radiotherapy after radical prostatectomy: a randomised controlled trial (EORTC trial 22911). Lancet 366(9485):572–578. https://doi.org/10.1016/S0140-6736(05)67101-2
Bolla M, van Poppel H, Tombal B, Vekemans K, Da Pozzo L, de Reijke TM, Verbaeys A, Bosset JF, van Velthoven R, Colombel M, van de Beek C, Verhagen P, van den Bergh A, Sternberg C, Gasser T, van Tienhoven G, Scalliet P, Haustermans K, Collette L (2012) Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer: long-term results of a randomised controlled trial (EORTC trial 22911). Lancet 380(9858):2018–2027. https://doi.org/10.1016/s0140-6736(12)61253-7
Thompson IM, Tangen CM, Paradelo J et al (2006) Adjuvant radiotherapy for pathologically advanced prostate cancer: a randomized clinical trial. JAMA 296(19):2329–2335. https://doi.org/10.1001/jama.296.19.2329
Thompson IM, Tangen CM, Paradelo J, Lucia MS, Miller G, Troyer D, Messing E, Forman J, Chin J, Swanson G, Canby-Hagino E, Crawford ED (2009) Adjuvant radiotherapy for pathologic T3N0M0 prostate cancer significantly reduces risk of metastases and improves survival: long-term followup of a randomized clinical trial. J Urol 181(3):956–962. https://doi.org/10.1016/j.juro.2008.11.032
Wiegel T, Bottke D, Steiner U, Siegmann A, Golz R, Storkel S, Willich N, Semjonow A, Souchon R, Stockle M, Rube C, Weissbach L, Althaus P, Rebmann U, Kalble T, Feldmann HJ, Wirth M, Hinke A, Hinkelbein W, Miller K (2009) Phase III postoperative adjuvant radiotherapy after radical prostatectomy compared with radical prostatectomy alone in pT3 prostate cancer with postoperative undetectable prostate-specific antigen: ARO 96-02/AUO AP 09/95. J Clin Oncol 27(18):2924–2930. https://doi.org/10.1200/jco.2008.18.9563
Wiegel T, Bartkowiak D, Bottke D, Thamm R, Hinke A, Stöckle M, Rübe C, Semjonow A, Wirth M, Störkel S, Golz R, Engenhart-Cabillic R, Hofmann R, Feldmann H‑J, Kälble T, Siegmann A, Hinkelbein W, Steiner U, Miller K (2015) Prostate-specific antigen persistence after radical prostatectomy as a predictive factor of clinical relapse-free survival and overall survival: 10-year data of the ARO 96-02 trial. Int J Radiat Oncol Biol Phys 91(2):288–294. https://doi.org/10.1016/j.ijrobp.2014.09.039
Wiegel T, Bartkowiak D, Bottke D, Bronner C, Steiner U, Siegmann A, Golz R, Storkel S, Willich N, Semjonow A, Stockle M, Rube C, Rebmann U, Kalble T, Feldmann HJ, Wirth M, Hofmann R, Engenhart-Cabillic R, Hinke A, Hinkelbein W, Miller K (2014) Adjuvant radiotherapy versus wait-and-see after radical prostatectomy: 10-year follow-up of the ARO 96-02/AUO AP 09/95 trial. Eur Urol 66(2):243–250. https://doi.org/10.1016/j.eururo.2014.03.011
Cozzarini C, Fiorino C, Da Pozzo LF, Alongi F, Berardi G, Bolognesi A, Briganti A, Broggi S, Deli A, Guazzoni G, Perna L, Pasetti M, Salvadori G, Montorsi F, Rigatti P, Di Muzio N (2012) Clinical factors predicting late severe urinary toxicity after postoperative radiotherapy for prostate carcinoma: a single-institute analysis of 742 patients. Int J Radiat Oncol Biol Phys 82(1):191–199. https://doi.org/10.1016/j.ijrobp.2010.09.027
Sowerby RJ, Gani J, Yim H, Radomski SB, Catton C (2014) Long-term complications in men who have early or late radiotherapy after radical prostatectomy. Can Urol Assoc J 8(7–8):253–258. https://doi.org/10.5489/cuaj.1764
Hegarty SE, Hyslop T, Dicker AP, Showalter TN (2015) Radiation therapy after radical prostatectomy for prostate cancer: evaluation of complications and influence of radiation timing on outcomes in a large, population-based cohort. PLoS ONE 10(2):e118430. https://doi.org/10.1371/journal.pone.0118430
Zaffuto E, Gandaglia G, Fossati N, Dell’Oglio P, Moschini M, Cucchiara V, Suardi N, Mirone V, Bandini M, Shariat SF, Karakiewicz PI, Montorsi F, Briganti A (2017) Early postoperative radiotherapy is associated with worse functional outcomes in patients with prostate cancer. J Urol 197(3):669–675. https://doi.org/10.1016/j.juro.2016.09.079
Pearse M, Fraser-Browne C, Davis ID, Duchesne GM, Fisher R, Frydenberg M, Haworth A, Jose C, Joseph DJ, Lim TS, Matthews J, Millar J, Sidhom M, Spry NA, Tang CI, Turner S, Williams SG, Wiltshire K, Woo HH, Kneebone A (2014) A Phase III trial to investigate the timing of radiotherapy for prostate cancer with high-risk features: background and rationale of the Radiotherapy—Adjuvant Versus Early Salvage (RAVES) trial. BJU Int 113(Suppl 2):7–12. https://doi.org/10.1111/bju.12623
National Cancer Institute (2010) Common terminology criteria for adverse events version 4.03. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed 2016-01-28 (Archived by WebCite® at http://www.webcitation.org/6nbc063zm)
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA (2016) The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 40(2):244–252. https://doi.org/10.1097/pas.0000000000000530
Mallick S, Madan R, Julka PK, Rath GK (2015) Radiation induced cystitis and proctitis—prediction, assessment and management. Asian Pac J Cancer Prev 16(14):5589–5594
Pinkawa M, Berneking V, König L, Frank D, Bretgeld M, Eble MJ (2017) Hydrogel injection reduces rectal toxicity after radiotherapy for localized prostate cancer. Strahlenther Onkol 193(1):22–28. https://doi.org/10.1007/s00066-016-1040-6
Pinkawa M, Schubert C, Escobar-Corral N, Holy R, Eble MJ (2015) Application of a hydrogel spacer for postoperative salvage radiotherapy of prostate cancer. Strahlenther Onkol 191(4):375–379. https://doi.org/10.1007/s00066-014-0769-z
Elliott SP, Meng MV, Elkin EP, McAninch JW, Duchane J, Carroll PR (2007) Incidence of urethral stricture after primary treatment for prostate cancer: data from CaPSURE. J Urol 178(2):529–534. https://doi.org/10.1016/j.juro.2007.03.126
Valicenti RK, Thompson I Jr., Albertsen P, Davis BJ, Goldenberg SL, Wolf JS, Sartor O, Klein E, Hahn C, Michalski J, Roach M III, Faraday MM (2013) Adjuvant and salvage radiation therapy after prostatectomy: American Society for Radiation Oncology/American Urological Association guidelines. Int J Radiat Oncol Biol Phys 86(5):822–828. https://doi.org/10.1016/j.ijrobp.2013.05.029
Pfister D, Bolla M, Briganti A, Carroll P, Cozzarini C, Joniau S, van Poppel H, Roach M, Stephenson A, Wiegel T, Zelefsky MJ (2014) Early salvage radiotherapy following radical prostatectomy. Eur Urol 65(6):1034–1043. https://doi.org/10.1016/j.eururo.2013.08.013
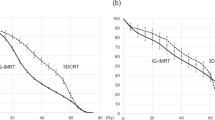
Michalski JM, Yan Y, Watkins-Bruner D, Walter B, Winter K, Galvin JM, Bahary J, Morton GC, Parliament MB, Sandler H (2011) Preliminary analysis of 3D-CRT vs. IMRT on the high dose arm of the RTOG 0126 prostate cancer trial: toxicity report. Int J Radiat Oncol Biol Phys 81(2):1–S2. https://doi.org/10.1016/j.ijrobp.2011.06.004
Waldstein C, Dörr W, Pötter R, Widder J, Goldner G (2018) Postoperative radiotherapy for prostate cancer. Strahlenther Onkol 194(1):23–30. https://doi.org/10.1007/s00066-017-1215-9
Cambria R, Cattani F, Jereczek-Fossa BA, Pansini F, Ciardo D, Vigorito S, Russo S, Zerini D, Cozzi L, Orecchia R (2014) Planning study to compare dynamic and rapid arc techniques for postprostatectomy radiotherapy of prostate cancer. Strahlenther Onkol 190(6):569–574. https://doi.org/10.1007/s00066-014-0601-9
Lee SH, Seo HJ, Lee NR, Son SK, Kim DK, Rha KH (2017) Robot-assisted radical prostatectomy has lower biochemical recurrence than laparoscopic radical prostatectomy: systematic review and meta-analysis. Investig Clin Urol 58(3):152–163. https://doi.org/10.4111/icu.2017.58.3.152
Fossati N, Karnes RJ, Boorjian SA, Moschini M, Morlacco A, Bossi A, Seisen T, Cozzarini C, Fiorino C, Noris Chiorda B, Gandaglia G, Dell’Oglio P, Joniau S, Tosco L, Shariat S, Goldner G, Hinkelbein W, Bartkowiak D, Haustermans K, Tombal B, Montorsi F, Van Poppel H, Wiegel T, Briganti A (2017) Long-term impact of adjuvant versus early salvage radiation therapy in pT3N0 prostate cancer patients treated with radical prostatectomy: results from a multi-institutional series. Eur Urol 71(6):886–893. https://doi.org/10.1016/j.eururo.2016.07.028
Budiharto T, Perneel C, Haustermans K, Junius S, Tombal B, Scalliet P, Renard L, Lerut E, Vekemans K, Joniau S, Van Poppel H (2010) A multi-institutional analysis comparing adjuvant and salvage radiation therapy for high-risk prostate cancer patients with undetectable PSA after prostatectomy. Radiother Oncol 97(3):474–479. https://doi.org/10.1016/j.radonc.2010.07.008
Detti B, Scoccianti S, Cassani S, Cipressi S, Villari D, Lapini A, Saieva C, Cai T, Pertici M, Giacomelli I, Livi L, Ceroti M, Nicita G, Carini M, Biti G (2013) Adjuvant and salvage radiotherapy after prostatectomy: outcome analysis of 307 patients with prostate cancer. J Cancer Res Clin Oncol 139(1):147–157. https://doi.org/10.1007/s00432-012-1309-9
Jereczek-Fossa BA, Zerini D, Vavassori A, Fodor C, Santoro L, Minissale A, Cambria R, Cattani F, Garibaldi C, Serafini F, Matei VD, de Cobelli O, Orecchia R (2009) Sooner or later? Outcome analysis of 431 prostate cancer patients treated with postoperative or salvage radiotherapy. Int J Radiat Oncol Biol Phys 74(1):115–125. https://doi.org/10.1016/j.ijrobp.2008.07.057
Mishra MV, Scher ED, Andrel J, Margules AC, Hegarty SE, Trabulsi EJ, Hyslop T, Den RB, Lallas CD, Gomella LG, Dicker AP, Showalter TN (2015) Adjuvant versus salvage radiation therapy for prostate cancer patients with adverse pathologic features: comparative analysis of long-term outcomes. Am J Clin Oncol 38(1):55–60. https://doi.org/10.1097/COC.0b013e318287bb6b
Ost P, De Troyer B, Fonteyne V, Oosterlinck W, De Meerleer G (2011) A matched control analysis of adjuvant and salvage high-dose postoperative intensity-modulated radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys 80(5):1316–1322. https://doi.org/10.1016/j.ijrobp.2010.04.039
D’Amico AV, Chen MH, Sun L, Lee WR, Mouraviev V, Robertson CN, Walther PJ, Polascik TJ, Albala DM, Moul JW (2010) Adjuvant versus salvage radiation therapy for prostate cancer and the risk of death. BJU Int 106(11):1618–1622. https://doi.org/10.1111/j.1464-410X.2010.09447.x
Hervas A, Gomez-Caamano A, Casana M, Gomez-Iturriaga A, Pastor J, Jove J, Mengual JL, Gonzalez-San Segundo C, Munoz J (2018) Adjuvant versus salvage radiotherapy in prostate cancer: multi-institutional retrospective analysis of the Spanish RECAP database. Clin Transl Oncol 20(2):193–200. https://doi.org/10.1007/s12094-017-1709-z
Buscariollo DL, Drumm M, Niemierko A, Clayman RH, Galland-Girodet S, Rodin D, Feldman AS, M Dahl M, McGovern FJ, F Olumi A, Eidelman A, Shipley WU, Zietman AL, Efstathiou JA (2017) Long-term results of adjuvant versus early salvage postprostatectomy radiation: a large single-institutional experience. Pract Radiat Oncol 7(2):e125–e133. https://doi.org/10.1016/j.prro.2016.10.010
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.M.E. Vogel, K.A. Kessel, J.E. Gschwend, W. Weichert, J.J. Wilkens and S.E. Combs declare that they have no competing interests.
Ethical standards
The present work is approved by the Ethics Commission of the Technical University of Munich (TUM) and is registered with the project number 320/14.
Rights and permissions
About this article
Cite this article
Vogel, M.M.E., Kessel, K.A., Gschwend, J.E. et al. Early and late toxicity profiles of patients receiving immediate postoperative radiotherapy versus salvage radiotherapy for prostate cancer after prostatectomy. Strahlenther Onkol 195, 131–144 (2019). https://doi.org/10.1007/s00066-018-1359-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1359-2