Abstract
Purpose
As the efficacy of all pediatric high-grade glioma (HGG) treatments is similar and still disappointing, it is essential to also investigate the toxicity of available treatments.
Methods
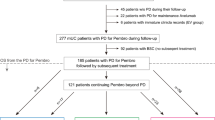
Prospectively recorded hematologic and nonhematologic toxicities of children treated with radiochemotherapy in the HIT GBM-C/D and HIT-HGG-2007 trials were compared. Children aged 3–18 years with histologically proven HGG (WHO grade III and IV tumors) or unequivocal radiologic diagnosis of diffuse intrinsic pontine glioma (DIPG) were included in these trials. The HIT-HGG-2007 protocol comprised concomitant radiochemotherapy with temozolomide, while cisplatinum/etoposide (PE) and PE plus ifosfamide (PEI) in combination with weekly vincristine injections were applied during radiochemotherapy in the HIT GBM-C/D protocol.
Results
Regular blood counts and information about cellular nadirs were available from 304 patients (leukocytes) and 306 patients (thrombocytes), respectively. Grade 3–4 leukopenia was much more frequent in the HIT GBM-C/D cohort (n = 88, 52%) vs. HIT-HGG-2007 (n = 13, 10%; P <0.001). Grade 3–4 thrombopenia was also more likely in the HIT GBM-C/D cohort (n = 21, 12% vs. n = 3,2%; P <0.001). Grade 3–4 leukopenia appeared more often in children aged 3–7 years (n = 38/85, 45%) than in children aged 8–12 years (n = 39/120, 33%) and 13–18 years (24/100, 24%; P =0.034). In addition, sickness was more frequent in the HIT GBM-C/D cohort (grade 1–2: 44%, grade 3–4: 6% vs. grade 1–2: 28%, grade 3–4: 1%; P <0.001).
Conclusion
Radiochemotherapy involving cisplatinum-based polychemotherapy is more toxic than radiotherapy in combination with temozolomide. Without evidence of differences in therapeutic efficacy, the treatment with lower toxicity, i. e., radiotherapy with temozolomide should be used.
Zusammenfassung
Zielsetzung
Die Wirksamkeit verschiedener Protokolle zur Radiochemotherapie bei Kindern mit hochmalignen Gliomen („high-grade glioma“, HGG) ist ähnlich und leider noch enttäuschend. Es erscheint vordringlich, auch die Toxizität verschiedener Therapieprotokolle zu untersuchen.
Methoden
Es wurden prospektiv erhobene hämatologische und nichthämatologische Toxizitäten von Kindern verglichen, die in der HIT-GBM-C/D- bzw. HIT-HGG-2007-Studie mit einer Radiochemotherapie behandelt wurden. In diesen Studien wurden Kinder im Alter von 3–18 Jahren mit histologisch gesichertem HGG (WHO-Grad-III-und -Grad-IV-Tumore) oder eindeutiger radiologischer Diagnose eines diffusen intrinsischen Ponsglioms (DIPG) eingeschlossen. Das HIT-HGG-2007-Protokoll umfasste eine konkomitante Radiochemotherapie mit Temozolomid; das HIT-GBM-C/D-Protokoll bestand aus Cisplatin/Etoposid (PE) und PE plus Ifosfamid (PEI) in Kombination mit wöchentlichen Vincristin-Injektionen während der Radiochemotherapie.
Ergebnisse
Regelmäßige Blutbilder waren von je 304 (Leukozyten) und 306 Patienten (Thrombozyten) verfügbar. Eine Grad-3/4-Leukopenie trat deutlich häufiger in der HIT-GBM-C/D- (n = 88, 52 %) als in der HIT-HGG-2007-Kohorte (n = 13, 10 %; P <0,001) auf. Ebenso war eine Grad-3/4-Thrombopenie in der HIT-GBM-C/D-Kohorte deutlich wahrscheinlicher (n = 21, 12 % vs. n = 3, 2 %; P <0,001). Eine Grad-3/4-Leukopenie trat bei Kindern zwischen 3–7 Jahren (38/85, 45 %) häufiger auf als bei Kindern zwischen 8–12 (39/120, 33 %) bzw. 13–18 Jahren (24/100, 24 %; P =0,034). Auch nichthämatologische Toxizität, z. B. Übelkeit, war in der HIT-GBM-C/D-Kohorte häufiger (Grad 1–2: 44 %, Grad 3–4: 6 % vs. Grad 1–2: 28 %, Grad 3–4: 1 %; P <0,001).
Schlussfolgerung
Eine Cisplatin-basierte Polychemotherapie ist toxischer als die Radiochemotherapie mit Temozolomid. Bei fehlender Evidenz für therapeutische Überlegenheit sollte die Behandlung mit geringerer Toxizität, d. h. Radiochemotherapie mit Temozolomid, verwendet werden.



Similar content being viewed by others
References
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Nachbichler SB, Schupp G, Ballhausen H et al (2017) Temozolomide during radiotherapy of glioblastoma multiforme daily administration improves survival. Strahlenther Onkol. https://doi.org/10.1007/s00066-017-1110-4
Mayer A, Schwanbeck C, Sommer C et al (2015) Adjuvant temozolomide-based chemoradiotherapy versus radiotherapy alone in patients with WHO III astrocytoma: The Mainz experience. Strahlenther Onkol 191(8):665–671
Sposto R, Ertel IJ, Jenkin RD et al (1989) The effectiveness of chemotherapy for treatment of high grade astrocytoma in children: Results of a randomized trial. A report from the Childrens Cancer Study Group. J Neurooncol 7:165–177
Broniscer A, Chintagumpala M, Fouladi M et al (2006) Temozolomide after radiotherapy for newly diagnosed high-grade glioma and unfavorable low-grade glioma in children. J Neurooncol 76:313–319
Nicholson HS, Kretschmar CS, Krailo M et al (2007) Phase 2 study of temozolomide in children and adolescents with recurrent central nervous system tumors: A report from the Children’s Oncology Group. Cancer 110:1542–1550
Cohen KJ, Pollack IF, Zhou T et al (2011) Temozolomide in the treatment of high-grade gliomas in children: a report from the Children’s Oncology Group. Neuro-Oncology 13:317–323
Cohen KJ, Heideman RL, Zhou T et al (2011) Temozolomide in the treatment of children with newly diagnosed diffuse intrinsic pontine gliomas: A report from the Children’s Oncology Group. Neuro-Oncol 13:410–416
Wolff JEA, Driever PH, Erdlenbruch B et al (2010) Intensive chemotherapy improves survival in pediatric high-grade glioma after gross total resection: Results of the HIT-GBM-C protocol. Cancer 116:705–712
Wolff JE, Kortmann R‑D, Wolff B et al (2011) High dose methotrexate for pediatric high grade glioma: Results of the HIT-GBM-D pilot study. J Neurooncol 102:433–442
Louis et al (2007) WHO classification of tumors of the central nervous sytem. IARC Press, Lyon
Warmuth-Metz M, Bison B, Leykamm S (2009) Neuroradiologic review in pediatric brain tumor studies. Klin Neuroradiol 19:263–273
Fangusaro J, Warren KE (2013) Unclear standard of care for pediatric high grade glioma patients. J Neurooncol 113(2):341–342
Stupp R, Hegi ME, Gorlia T et al (2014) Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071-22072 study): A multicentre, randomised, open-label, phase 3 trial. Lancet Oncol 15:1100–1108
Gilbert MR, Dignam JJ, Armstrong TS et al (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370:699–708
Chinot OL, Wick W, Mason W et al (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 370:709–722
Finlay JL, Boyett JM, Yates AJ et al (1995) Randomized phase III trial in childhood high-grade astrocytoma comparing vincristine, lomustine, and prednisone with the eight-drugs-in-1-day regimen. Childrens Cancer Group. J Clin Oncol 13:112–123
Pixberg C, Koch R, Eich HT et al (2016) Acute toxicity grade 3 and 4 after irradiation in children and adolescents: Results from the IPPARCA collaboration. Int J Radiat Oncol Biol Phys 94(4):792–799
Minniti G, De Sanctis V, Muni R et al (2008) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma in elderly patients. J Neurooncol 88:97–103
Sijben AE, McIntyre JB, Roldán GB et al (2008) Toxicity from chemoradiotherapy in older patients with glioblastoma multiforme. J Neurooncol 89:97–103
Brandes AA, Franceschi E, Tosoni A et al (2009) Temozolomide concomitant and adjuvant to radiotherapy in elderly patients with glioblastoma: Correlation with MGMT promoter methylation status. Cancer 115:3512–3518
Wick W, Platten M, Meisner C et al (2012) Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: The NOA-08 randomised, phase 3 trial. Lancet Oncol 13:707–715
Balducci L, Colloca G, Cesari M et al (2010) Assessment and treatment of elderly patients with cancer. Surg Oncol 19:117–123
Gupta AA, Anderson JR, Pappo AS et al (2012) Patterns of chemotherapy-induced toxicities in younger children and adolescents with Rhabdomyosarcoma: A report from the Children’s Oncology Group Soft Tissue Sarcoma Committee. Cancer 118(4):1130–1137
Elias GP, Antoniali C, Mariano RC et al (2005) Comparative study of rules employed for calculation of pediatric drug dosage. J Appl Oral Sci 13(2):114–119
Jackacki RI, Cohen KJ, Buxton A et al (2016) Phase 2 study of concurrent radiotherapy and temozolomide followed by temozolomide and lomustine in the treatment of children with high-grade glioma: A report of the Children’s Oncology Group ACNS0423 study. Neuro Oncol 18(10):1442–1450
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C. M. Kramm reports grants from Deutsche Kinderkrebsstiftung, Bonn, Germany, during the conduct of the study; grants from Merck, KGaA Darmstadt, Germany, outside the submitted work. B. Bison reports personal fees and nonfinancial support from Deutsche Kinderkrebsstiftung, during the conduct of the study; personal fees and nonfinancial support from Deutsche Kinderkrebsstiftung, outside the submitted work. C. Seidel, A.O. von Bueren, S. Bojko, M. Hoffmann, T. Pietsch, G.H. Gielen, M. Warmuth-Metz and R.‑D. Kortmann declare that they have no competing interests.
Additional information
Clemens Seidel and André O. von Bueren contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Seidel, C., von Bueren, A.O., Bojko, S. et al. Concurrent radiotherapy with temozolomide vs. concurrent radiotherapy with a cisplatinum-based polychemotherapy regimen. Strahlenther Onkol 194, 215–224 (2018). https://doi.org/10.1007/s00066-017-1218-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-017-1218-6