Background and Purpose:
To assess the late effect of a prostaglandin, given rectally during irradiation, on late rectal toxicity. In the acute treatment setting no significant differences in reducing the incidence of acute proctitis symptoms in patients receiving misoprostol, however, significantly more rectal bleeding had been reported.
Patients and Methods:
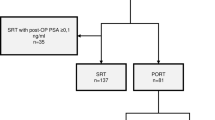
A total of 100 patients who had undergone radiotherapy for prostate cancer had been entered into this phase III randomized, placebo-controlled, double-blind study with misoprostol or placebo suppositories. The toxicity was evaluated yearly after cessation of irradiation by the RTOG/LENT-SOMA scale.
Results:
The median follow-up was 50 months. 20 patients suffered from grade 1, four patients from grade 2 as well, and three patients only from grade 2 toxicity. Frequency, bleeding and urgency were the most commonly reported symptoms. In keeping with other studies and clinical experience, the symptoms peaked within the first 2 years with a median for grade 1 of 13 months and for grade 2 of 15 months. The presence of acute toxicity grade 2 showed a correlation with the development of any late toxicity (p = 0.03). Any acute rectal bleeding was significant correlated with any late rectal bleeding (p = 0.017).
Conclusion:
Misoprostol given as once-daily suppository for prevention of acute radiation-induced proctitis does neither influence the incidence and severity of radiation-induced acute nor late rectal toxicity. Misoprostol has no negative impact on the incidence and severity of late rectal bleeding, in contrast to acute rectal bleeding. The routine clinical use of misoprostol suppositories cannot be recommended.
Hintergrund und Ziel:
Diese Untersuchung wurde durchgeführt, um einen potentiellen Einfluss von zur Prophylaxe der akuten Proktitis rektal gegebenem Misoprostol auf radiogene rektale Spätreaktionen zu evaluieren.
Patienten und Methodik:
100 Patienten, die mit Radiotherapie bei Prostatakarzinom behandelt wurden, wurden in diese randomisierte, plazebokontrollierte, doppelblinde Phase-III-Studie mit Misoprostol- bzw. Plazebozäpfchen eingeschlossen. Die Toxizität wurde jährlich anhand der RTOG- und LENT-SOMA-Skalen erhoben.
Ergebnisse:
Der mediane Nachbeobachtungszeitraum betrug 50 Monate. Bei 20 Patienten trat eine Grad-1-, bei vier ebenfalls eine Grad-2- und bei drei Patienten nur eine Grad-2-Toxizität auf. Frequenz, Blutung und Stuhldrang waren die häufigsten Symptome. Vergleichbar mit anderen Studien und klinischer Erfahrung, traten die Symptome am häufigsten innerhalb der ersten 2 Jahre mit einer medianen Zeit von 13 Monaten für Grad-1- und 15 Monaten für Grad-2-Proktitis auf. Das Vorhandensein akuter Grad-2-Toxizität zeigte eine Korrelation mit der Entwicklung von später Toxizität (p = 0,03). Akute Blutung war signifikant korreliert mit später Blutung (p = 0,017).
Schlussfolgerung:
Misoprostol, einmal täglich als Zäpfchen zur Prävention der akuten radiotherapieinduzierten Proktitis gegeben, beeinflusst weder die Inzidenz und Schwere der radiotherapieinduzierten akuten noch der späten rektalen Toxizität. Misoprostol hat keinen negativen Einfluss auf die Häufigkeit und Schwere von später rektaler Blutung im Gegensatz zu akuter Blutung. Der Routineeinsatz von Misoprostolzäpfchen kann nicht empfohlen werden.
Similar content being viewed by others
References
Arcangeli S, Saracino B, Petrongari MG, et al. Analysis of toxicity in patients with high risk prostate cancer treated with intensity-modulated pelvic radiation therapy and simultaneous integrated dose escalation to prostate area. Radiother Oncol 2007;84:148–55.
Ben-Josef E, Han S, Tobi M, et al. A pilot study of topical intrarectal application of amifostine for prevention of late radiation rectal injury. Int J Radiat Oncol Biol Phys 2002;53:1160–4.
Ben-Josef E, Han S, Tobi M, et al. Intrarectal application of amifostine for the prevention of radiation-induced rectal injury. Semin Radiat Oncol 2002;12:Suppl 1:81–5.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341–6.
Delaney JP, Bonsack ME, Felemovicius I. Misoprostol in the intestinal lumen protects against radiation injury of the mucosa of the small bowel. Radiat Res 1994;137:405–9.
El-Bassiouni M, Davis JB, El-Attar I, et al. Target motion variability and on-line positioning accuracy during external-beam radiation therapy of prostate cancer with an endorectal balloon device. Strahlenther Onkol 2006;182:531–6.
Elsayed H, Bölling T, Moustakis C, et al. Organ movements and dose exposures in teletherapy of prostate cancer using a rectal balloon. Strahlenther Onkol 2007;183:617–24.
Empey LR, Papp JD, Jewell LD, et al. Mucosal protective effects of vitamin E and misoprostol during acute radiation-induced enteritis in rats. Dig Dis Sci 1992;37:205–14.
Gilbertson TJ, Ruwart MJ, Stryd RP, et al. Partial characterization of the gastrointestinal weight changes produced in the female rat by 16,16-dimethylprostaglandin E2. Prostaglandins 1983;26:745–59.
Hanson WR, DeLaurentiis K. Comparison of in vivo murine intestinal radiation protection by E-prostaglandins. Prostaglandins 1987;33:Suppl:93–104.
Hanson WR, Houseman KA, Collins PW. Radiation protection in vivo by prostaglandins and related compounds of the arachidonic acid cascade. Pharmacol Ther 1988;39:347–56.
Hanson WR, Houseman KA, Nelson AK, et al. Radiation protection of the murine intestine by misoprostol, a prostaglandin E1 analogue, given alone or with WR-2721, is stereospecific. Prostaglandins Leukot Essent Fatty Acids 1988;32:101–5.
Hanson WR, Marks JE, Reddy SP, et al. Protection from radiation-induced oral mucositis by a mouth rinse containing the prostaglandin E1 analog, misoprostol: a placebo controlled double blind clinical trial. Adv Exp Med Biol 1997;400B:811–8.
Hanson WR, Thomas C. 16,16-dimethyl prostaglandin E2 increases survival of murine intestinal stem cells when given before photon radiation. Radiat Res 1983;96:393–8.
Henriksson R, Franzen L, Littbrand B. Effects of sucralfate on acute and late bowel discomfort following radiotherapy of pelvic cancer. J Clin Oncol 1992;10:969–75.
Hille A, Schmidberger H, Hermann RM, et al. A phase III randomized, placebo-controlled, double-blind study of misoprostol rectal suppositories to prevent acute radiation proctitis in patients with prostate cancer. Int J Radiat Oncol Biol Phys 2005;63:1488–93.
International Commission on Radiation Units and Measurements. ICRU report 50: prescribing, recording, and reporting photon beam therapy. Washington: International Commission on Radiation Units and Measurements, 1993.
Keelan M, Thomson AB, Clandinin MT, et al. Effect of oral enprostil, a synthetic prostaglandin E2, on intestinal brush border membrane lipid composition following abdominal irradiation in the rat. Clin Invest Med 1989;12:350–6.
Khan AM, Birk JW, Anderson JC, et al. A prospective randomized placebo-controlled double-blinded pilot study of misoprostol rectal suppositories in the prevention of acute and chronic radiation proctitis symptoms in prostate cancer patients. Am J Gastroenterol 2000;95:1961–6.
Kneebone A, Mameghan H, Bolin T, et al. The effect of oral sucralfate on the acute proctitis associated with prostate radiotherapy: a double-blind, randomized trial. Int J Radiat Oncol Biol Phys 2001;51:628–35.
Koper JC, Stroom JC, van Puten WL, et al. Acute morbidity reduction using 3DCRT for prostate carcinoma: a randomized study. Int J Radiat Oncol Biol Phys 1999;43:727–34.
Kouvaris J, Kouloulias V, Malas E, et al. Amifostine as radioprotective agent for the rectal mucosa during irradiation of pelvic tumors. A phase II randomized study using various toxicity scales and rectosigmoidoscopy. Strahlenther Onkol 2003;179:167–74.
LENT SOMA scales for all anatomic sites. Int J Radiat Oncol Biol Phys 1995;31:1049–91.
Lin C, Turner S, Mai T, et al. Late rectal and urinary toxicity from conformal, dose-escalated radiation therapy for prostate cancer: a prospective study of 402 patients. Australas Radiol 2007;51:578–83.
Martenson JA, Bollinger JW, Sloan JA, et al. Sucralfate in the prevention of treatment-induced diarrhea in patients receiving pelvic radiation therapy: A North Central Cancer Treatment Group phase III double-blind placebo-controlled trial. J Clin Oncol 2000;18:1239–45.
Michalski JM, Purdy JA, Winter K, et al. Preliminary report of toxicity following 3D radiation therapy for prostate cancer on 3DOG/RTOG 9406. Int J Radiat Oncol Biol Phys 2000;46:391–402.
Montana GS, Anscher MS, Mansbach CM II, et al. Topical application of WR-2721 to prevent radiation-induced proctosigmoiditis. A phase I/II trial. Cancer 1992;69:2826–30.
O’Brien PC, Franklin CI, Dear KB, et al. A phase III double-blind randomised study of rectal sucralfate suspension in the prevention of acute radiation proctitis. Radiother Oncol 1997;45:117–23.
Pinkawa M, Siluschek J, Gagel B, et al. Postoperative radiotherapy for prostate cancer: evaluation of target motion and treatment techniques (intensity-modulated versus conformal radiotherapy). Strahlenther Onkol 2007;183:23–9.
Rauch K, Weiland H. Therapy of radiogenic colitis with salicylazosulfapyridine (azulfidine) Strahlentherapie 1972;143:660–3.
Reinhart WH, Muller O, Halter F. Influence of long-term 16,16-dimethyl prostaglandin E2 treatment on the rat gastrointestinal mucosa. Gastroenterology 1983;85:1003–10.
Sanguineti G, Cavey ML, Endres EJ, et al. Does treatment of the pelvic nodes with IMRT increase late rectal toxicity over conformal prostate-only radiotherapy to 76 Gy? Strahlenther Onkol 2006;182:543–9.
Sanguineti G, Franzone P, Marcenaro M, et al. Sucralfate versus mesalazine versus hydrocortisone in the prevention of acute radiation proctitis during conformal radiotherapy for prostate carcinoma. A randomized study. Strahlenther Onkol 2003;179:464–70.
Schultheiss TE, Lee WR, Hunt MA, et al. Late GI and GU complications in the treatment of prostate cancer. Int J Radiat Oncol Biol Phys 1997;37:3–11.
Shrader-Bogen CL, Kjellberg JL, McPherson CP, et al. Quality of life and treatment outcomes: prostate carcinoma patients’ perspectives after prostatectomy or radiation therapy. Cancer 1997;79:1977–86.
Simone NL, Ménard C, Soule BP, et al. Intrarectal amifostine during external beam radiation therapy for prostate cancer produces significant improvements in quality of life measured by EPIC score. Int J Radiat Oncol Biol Phys 2008;70:90–5.
Singh AK, Ménard C, Guion P, et al. Intrarectal amifostine suspension may protect against acute proctitis during radiation therapy for prostate cancer: a pilot study. Int J Radiat Oncol Biol Phys 2006;65:1008–13.
Storey MR, Pollack A, Zagars G, et al. Complications from radiotherapy dose escalation in prostate cancer: preliminary results of a randomized trial. Int J Radiat Oncol Biol Phys 2000;48:635–42.
Szepesi S, Jakobi V, Vecsei P, et al. Treatment of radiogenic colitis with a rectal foam containing cortisol. Clinical and pharmacologic data. Strahlenther Onkol 1990;166:271–4.
Thomson AB, Keelan M, Clandinin MT, et al. Lack of protective effect of oral enprostil, a synthetic prostaglandin E2, on intestinal transport and morphology following abdominal irradiation in the rat. Can J Physiol Pharmacol 1989;67:1351–6.
Trotti A, Byhardt R, Stetz J, et al. Common Toxicity Criteria: version 2.0. an improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys 2000;47:13–47.
Weiss E, Hirnle P, Arnold-Bofinger H, et al. Therapeutic outcome and relation of acute and late side effects in the adjuvant radiotherapy of endometrial carcinoma stage I and II. Radiother Oncol 1999;53:37–44.
Weiss W, Horninger W, Forthuber BC, et al. Single-institution results of primary external-beam radiation for the treatment of T1–T3 prostate cancer. Strahlenther Onkol 2007;183:321–6.
Wertz H, Lohr F, Dobler B, et al. Dosimetric impact of image-guided translational isocenter correction for 3-D conformal radiotherapy of the prostate. Strahlenther Onkol 2007;183:203–10.
Widmark A, Fransson P, Tavelin B, et al. Self-assessment questionnaire for evaluating urinary and intestinal late side effects after pelvic radiotherapy in patients with prostate cancer compared with an age-matched control population. Cancer 1994;74:2520–32.
Zelefsky MJ, Levin EJ, Hunt M, et al. Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 2008;70:1124–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kertesz, T., Herrmann, M.K.A., Zapf, A. et al. Effect of a Prostaglandin – Given Rectally for Prevention of Radiation-Induced Acute Proctitis – on Late Rectal Toxicity. Strahlenther Onkol 185, 596–602 (2009). https://doi.org/10.1007/s00066-009-1978-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-009-1978-8