Abstract
Background
Overweight/obesity in patients after total hip arthroplasty (THA) is a growing problem and is associated with postoperative complications and a negative effect on functional outcome. The objective of this study is to determine to what extent overweight/obesity is associated with physical functioning and health-related quality of life 1 year after primary THA.
Methods
A retrospective analysis of prospectively collected data from 653 patients who had undergone a primary THA was conducted. Physical functioning, health-related quality of life, body mass index (BMI), comorbidity, and postoperative complications were assessed by means of a questionnaire and from medical records. To determine to what extent overweight/obesity is associated with physical functioning and health-related quality of life after THA, a structural equation model (SEM) analysis was conducted.
Results
The association of BMI corrected for age, gender, complications, and comorbidity with physical functioning is −0.63. This means that an increase in 1 kg/m2 BMI leads to a reduction of 0.63 points in the physical functioning score as measured with the Western Ontario and McMaster Universities Osteoarthritis Index (100-point scale). The prevalence of complications or comorbidity leads to a reduction of, respectively, 5.63 and 7.25 (one or two comorbidities) and 14.50 points in the case of more than two comorbidities on the physical functioning score. The same pattern is observed for health-related quality of life.
Conclusions
The influence of overweight/obesity on physical functioning and health-related quality of life is low. The impact of complications and comorbidity is considerable. Refusing a patient a THA solely on the basis of overweight or obesity does not seem justified.
Similar content being viewed by others
Introduction
Osteoarthrosis (OA) of the hip is one of the most prevalent age-related musculoskeletal conditions, leading to a significant impairment in patients’ ability to perform activities of daily living and having a large impact on health-related quality of life [1, 2]. In the US population, symptomatic OA of the hip is reported to affect 8.7% of men and 9.3% of women aged 45 years or older [3]. Among the Dutch population, these prevalences were 2.5% for men and 5.0% for women in 2000 [4]. Total hip arthroplasty (THA) is a highly successful and widely applied treatment for advanced OA of the hip, with 202,500 primary THAs performed in the US in 2003 [5] and 20,266 in the Netherlands in 2008 [6].
In the year 2006, an estimated 40% of adults aged over 65 in the US general population were overweight, and another 22% were obese [7]. In the Dutch general population, almost 57% of adults over age 65 were overweight in 2006, while 14% were obese [8]. Overweight is also a growing problem in patients after a THA. Overweight/obesity is associated with a negative effect on functional outcome after THA and on implant longevity. It can affect polyethylene wear negatively. Studies have also found a correlation between obesity and higher infection rates and risk of dislocation, aseptic loosening, and revision [9–12]. Moreover, with respect to general health, overweight/obesity is considered a risk factor for hypertension, type 2 diabetes, coronary heart disease, stroke, gallbladder disease, respiratory problems, and some forms of cancer (National Institutes of Health) [13]. The World Health Organization considers obesity as a chronic disease [14].
Limited research has been conducted so far into the potentially negative effect of overweight/obesity on functional outcome and health-related quality of life after THA [9]. Based on the scarce research done, it is difficult to draw uniform conclusions, as different instruments, points in time, and perspectives (physician-based vs. patient-based) have been used [15–22]. Moreover, for research conducted into the effect of overweight/obesity on functional outcome and health-related quality of life after THA, one must ask whether comorbidity and complications also have to be taken into account [21]. As mentioned, overweight and obesity are associated with a variety of additional health problems, and the same applies for postoperative complications.
Few studies have taken the influence of comorbidity and complications into account when assessing the influence of overweight/obesity on patient-perceived physical functioning and health-related quality of life. Therefore, the aim of the current study is to analyze the effect of overweight/obesity on patient-perceived physical functioning and health-related quality of life 1 year after THA. As overweight/obesity is considered one of the risk factors for a spectrum of comorbidity and postoperative complications, the additional effect on physical functioning and health-related quality of life of comorbidity and postoperative complications in combination with overweight/obesity was analyzed.
Materials and Methods
Subjects
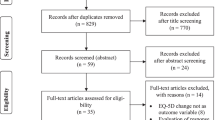
A retrospective analysis was done on prospectively collected data. Data were collected in three orthopedic centers (one university medical center, two regional hospitals) in the Netherlands. All patients who had undergone an elective primary THA because of primary OA of the hip between February 2005 and January 2007 were consecutively included. Patients who had died at the time of follow-up, who had other lower-limb arthroplasties performed in the period of follow-up, or who had cognitive limitations were excluded. Patients were sent a self-report questionnaire with an explanatory letter 1 year postoperatively (mean, 52.4 weeks; SD, 3.9 weeks).
Surgery was performed by 15 staff surgeons or under direct supervision of one of these surgeons. Patients were operated on using a posterolateral or anterolateral approach. This approach was surgeon-specific, with each surgeon using the same approach consistently for all THAs performed during the study period. Different types of implants and fixation types were used. Patients were allowed full weight bearing the second day after surgery, using crutches during the first three postoperative months.
The study was approved and conducted in accordance with the regulations of the medical ethical boards of the participating hospitals. Patients were informed in the explanatory letter that return of the completed questionnaire would be taken as consent to participate.
Instruments
To measure patient-perceived physical functioning, the Dutch-language version of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was used [23, 24]. The WOMAC is a widely used disease-specific questionnaire for measuring outcome after THA [25]. Using a Likert scale, individuals rate themselves on multiple items grouped into three domains: pain (5 items), stiffness (2 items), and physical functioning (17 items). The scores of the subscales make up the total score. The total score of 96 points is recoded into a 100-point scale, with a higher score representing better physical functioning. To get an impression of health-related quality of life, the subscale of self-perceived general health of the Short-Form 36 health survey (SF-36) was used [26]. General comorbidity was measured with the 12-item list from Nilsdotter [27]. Patients were rated as having no complications, one or two complications, or more than two. Body mass (in kilograms) and height (in meters) were self-reported. Body mass index (BMI) was calculated by dividing body mass in kilograms by height in square meters. A BMI <25 kg/m2 was considered normal weight, between 25 and 30 kg/m2 overweight, and >30 kg/m2 obese. Age, gender, and complications (perioperative and postoperative) were extracted from the medical records.
Statistical Analysis
Statistical analyses were performed using the SPSS 16 software (SPSS Inc, 233 S. Wacker Drive, Chicago, IL 60606, USA) and Mplus version 5 [28]. Descriptive statistics were used to depict the main characteristics of the patients. ANOVA with Bonferroni adjustment was used to compare continuous variables between the three BMI groups (BMI <25 kg/m2, BMI 25–30 kg/m2, and BMI >30 kg/m2). To determine to what extent overweight/obesity (independent variable) is predictive of patient-perceived physical functioning (WOMAC total score) and self-perceived general health (dependent variables), linear regression analysis was used. In addition, comorbidity (no, one to two, >2; no comorbidity = ref.) and complications (yes/no; no = ref.) were included as dummy variables in the analyses to correct for their influence. A p value of <0.05 was considered statistically significant.
The linear regression analysis was performed with a structural equation model (SEM) technique in order to determine to what extent overweight/obesity is associated with patient-perceived physical functioning and self-perceived general health after THA. Dependent variables were patient-perceived physical functioning and self-perceived general health. Independent variables were BMI, age, gender, complications, and comorbidity. BMI was centered at 25 as being the upper limit of a healthy weight and age at 70 years (the mean age of this study population). In addition, based on the SEM, the correlation of the two dependent variables was calculated.
Results
Of the 848 eligible patients, 653 (77.0%) returned complete questionnaires and were included. There were 484 female patients (74.1%). Mean age at surgery was 70.3 years (SD, 8.2 years; Table 1). Mean BMI of the patients was 27.0 kg/m2 (SD, 4.1 kg/m2). Most of the patients lived with a partner (59.1%) and had a lower educational level (49.3%; Table 1). A total of 181 patients (27.7%) reported no additional comorbidity, 263 patients (40.3%) one to two comorbidities, and 209 patients (32.0%) more than two comorbidities. Complications occurred in 47 (7.2%) patients. There were eight (1.2%) dislocations, three (0.5%) sciatic nerve palsies, three (0.5%) superior gluteal nerve palsies, two (0.3%) periprosthetic fractures, and two (0.3%) malpositioned prostheses necessitating revision surgery.
Patients did not differ with respect to mean age at surgery, comorbidity, or complications between the three BMI categories. With respect to gender, there were significantly more women in the BMI <25 group.
In order to determine to what extent overweight/obesity influences patient-perceived physical functioning and self-perceived general health after THA, an SEM analysis was conducted. The model had four steps. The first step/model determined the association of BMI with patient-perceived physical functioning and self-perceived general health, while the second model determined the independent effect of age and gender. In the third step/model, the effect of BMI, age, and gender were added into the model. In the final step (model 4), comorbidity and complications were added to estimate their additional effect (Table 2).
The influence of BMI on patient-perceived physical functioning and self-perceived general health as depicted in model 1 (Table 2) was −0.35 (p = 0.07) and −0.59 (p = 0.001), respectively. This means that, with every increase of 1 kg/m2 BMI, the score on patient-perceived physical functioning as measured with the WOMAC (100-point scale) is reduced by 0.35 and on the self-perceived general health subscale of the SF-36 (100-point scale) by 0.59 points. In model 2, the separate influence of age and gender are reported; in model 3, in combination with BMI. In both models, the influence of gender on patient-perceived physical functioning is distinct (respectively, −3.88 (p = 0.02) and −4.53 (p = 0.01)). Finally, model 4 reports the influence of BMI corrected not only for age and gender but also for complications and comorbidity. With respect to patient-perceived physical functioning, every increase in 1 kg/m2 BMI leads to a reduction of 0.63 points on the WOMAC score (p = 0.001). By contrast, the prevalence of complications or comorbidity leads to a reduction of, respectively, 5.63 (p = <0.001) and 7.25 (p = 0.01) points on the WOMAC score in the case of one or two comorbidities and a reduction of 14.50 points on the WOMAC score in the case of more than two comorbidities. With respect to the self-perceived general health of the SF-36, the same pattern is seen, although the influence of gender is less prominent. The correlation between the two dependent variables, patient-perceived physical functioning and self-perceived general health, is 0.35 in the last model. The R 2 for these last models was 0.10 for patient-perceived physical functioning and 0.13 for self-perceived general health, which implies that 10% and 13% of the variance could be explained (data not shown).
Discussion
It is generally considered that overweight/obesity is associated with a negative effect on outcome after THA and on implant longevity. From the results of our study, it can be concluded that the influence of overweight/obesity on patient-perceived physical functioning and self-perceived general health is low, both without and with correction for the other covariables. The sole influence of 1 kg/m2 increase in BMI leads to a reduction in the score on patient-perceived physical functioning as measured with the WOMAC by 0.35 points and on self-perceived general health as determined with the SF-36 by 0.59 points. This implies that, compared to a person with a BMI of 25 kg/m2, someone with a BMI of 35 kg/m2 of the same age and gender has a reduction in score on physical functioning and health-related quality of life of, respectively, 3.5 and 5.9 points. Corrected for the influence of complications, comorbidity, and the demographic variables, the influence of BMI remains more or less the same. On the other hand, the influence of complications is considerable and leads to a reduction in the physical functioning score of 5.63 points and health-related quality of life of 8.19 points. For comorbidity, the same pattern is seen with a reduction of 7.25 points for one or two comorbidities and 14.50 points for more than two comorbidities on the physical functioning score and a comparable effect on health-related quality of life with a reduction of, respectively, 7.02 and 14.04 points.
The question thus arises as to whether these effects can be considered clinically relevant. Angst et al. [29] report that differences larger than 6% of the maximum score on the WOMAC (96/100 points) and SF-36 (100 points) can be considered clinically relevant. With the exception of more than two comorbidities (reduction of 14.04 points on the SF-36 health perception scale), none of the variables lead to a relevant effect on their own, yet the combination of factors can rapidly lead to relevant differences. For example, being a woman in combination with a BMI of 30 kg/m2 and one or two comorbidities already leads to a clinically relevant effect on the physical functioning score. Still, overall, it can be stated that the sole effect of BMI on physical functioning and health-related quality of life is low and will only lead to a clinically relevant effect in extreme situations. On the other hand, the effects of comorbidity and complications are substantial.
Based on the aforementioned results, it can be argued that, in future research, comorbidity and complications have to be taken into account, otherwise an incorrect and incomplete picture is obtained. Until now, only a few studies have taken comorbidity and complications into account when assessing the influence of overweight/obesity on physical functioning and health-related quality of life. The findings of our study are in line with research by Kessler and Käfer [16], McCalden et al. [17], Moran et al. [18], Stickles et al. [19], and Andrew et al. [20]. Kessler and Käfer used the WOMAC as outcome measure. They concluded that overweight/obesity is of no influence, yet they measured 10 days and 3 months postoperatively. McCalden et al. [17] measured after a mean period of 8.4 years postoperatively and concluded that morbid obesity does not affect the postoperative outcome after THA as measured with the WOMAC, SF-12, and Harris Hip Score (HHS). Moran et al. [18] concluded that BMI did not lead to clinically relevant effects on the postoperative HHS and SF-36. Unlike the aforementioned studies, Moran et al. took both complications and comorbidity into account. However, it must be mentioned that we used a patient-based outcome (WOMAC) and Moran et al. used a physician-based outcome (HHS). Additionally, Stickles et al. [19] and Andrew et al. [20] concluded that obese patients enjoy as much improvement and satisfaction as non-obese patients. Stickles et al. found that there were no significant differences between obese and non-obese patients with respect to their improvement on the WOMAC score and the Physical Component and Mental Component scores of the SF-36. Andrew et al. concluded that there was no difference in the change in the Oxford Hip Score between obese and non-obese patients 5 years postoperatively.
It can be concluded that the results of our study are contrary to results reported by Busato et al. [21], who measured the effect of a high BMI on functional outcome in a cohort of 18,968 patients. They found that a high BMI is associated with decreased ambulation during a follow-up period of 15 years. By contrast, we measured only 1 year postoperatively, and our good results at that point do not rule out deterioration later on. Comparing our results with those of the study of Jackson et al. [22] leads to a mixed picture: they found a significant difference between obese and non-obese patients in favor of the non-obese group with respect to the postoperative HHS. And yet, they found no difference between the two groups in overall satisfaction with surgery.
Finally, it can be concluded that, with the exception of the Moran study, none of these studies takes the additional effect of comorbidity into account. The substantial impact of comorbidity found in our study is in line with suggestions stated in a research by Braeken et al. [15], who argued that more attention should be paid in future research to the potentially negative influence of comorbidity on physical functioning after THA.
Once again, a strength of our study is that not only the influence of overweight and obesity were taken into account but also the influence of additional comorbidity and postoperative complications. Additional strong points of our study are the size of our study group and the response rate of 77.0%. In order to get an impression of the representativeness of our study group, we determined the response rate by BMI category. As the BMI of the nonresponders was not available 1 year after THA, we used the BMI (of both responders and nonresponders) that was determined when the patients were admitted to the hospital for surgery. Divided by BMI category, the response rate was, respectively, 76.0% (BMI <25 kg/m2), 81.5% (BMI 25–30 kg/m2), and 71.1% (BMI >30 kg/m2). From this, it can be concluded that no response bias was present. A weak point is that height and weight and thus BMI were self-reported. This probably leads to an underestimation of the problem, as it is known that people tend to underestimate their weight and overestimate their height [30]. Secondly, we used the 12-item list from Nilsdotter [27] to get an impression of the presence of comorbidity. It can be argued that not all comorbidities are included in this instrument. On the other hand, the most prevalent comorbidities or health problems associated with overweight/obesity, like heart disease, hypertension, peripheral artery disease, diabetes, and cancer, are included in this instrument. Finally, our study was limited to the patients’ 1-year postoperative status. The long-term influence of overweight/obesity on patient-perceived physical functioning, health-related quality of life, and prosthetic longevity could not be determined. This latter point needs particular attention, as the present study used self-reported instruments and consequently no objective information was gathered about the effect of overweight on the prosthesis.
Conclusions
Overall, it can be concluded that the influence of overweight/obesity on physical functioning and health-related quality of life both with and without correcting for the other covariables is low. On the other hand, the impact of complications and comorbidity is considerable. Especially the combination of factors can rapidly lead to clinically relevant differences. In that sense, it can be concluded that future research into the effect of obesity/comorbidity on physical functioning and health-related quality of life must take comorbidity and complications into account, otherwise an incorrect and incomplete picture is obtained. Finally, based on the results of this study, it can be concluded that refusing a patient a THA solely on the basis of overweight or obesity seems unjustified.
References
Alonso J, Ferrer M, Gandek B, et al. Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) project. Qual Life Res. 2004;13:283–98.
Fautrel B, Hilliquin P, Rozenberg S, et al. Impact of osteoarthritis: results of a nationwide survey of 10,000 patients consulting for OA. Joint Bone Spine. 2005;72:235–40.
Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Arthritis Rheum. 1998;58:26–35.
RIVM. Frequency of occurrence of osteoarthrosis and what is the mortality rate? http://www.rivm.nl/vtv/object_document/o1778n18371.html.
Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5.
Prismant. Yeardisk for the hospitals. http://cognosserver.prismant.nl/cognos7/cgi-bin/ppdscgi.cgi?DC=Q&E=/Prisma-Landelijke-LMR/Landelijke+LMR-informatie+−+Verrichtingen.
Centers for Disease Control and Prevention (CDC). Behavioral risk factor surveillance system survey data. Atlanta, Georgia: US Department of Health and Human Services, Centers for Disease Control and Prevention. http://apps.nccd.cdc.gov/brfss/age.asp?cat=OB&Yr=2006&qkey=4409&state=UB.
CBS. Health-well being statistics. http://www.cbs.nl/nl-NL/menu/themas/gezondheid-welzijn/cijfers/default/htm.
Dowsey MM, Choong PFM. Early outcomes and complications following joint arthroplasty in obese patients: a review of the published reports. ANZ J Surg. 2008;78:439–44.
Münger P, Röder C, Ackermann-Liebrich U, et al. Patient-related risk factors leading to aseptic stem loosening in total hip arthroplasty. A case–control study of 5,035 patients. Acta Orthop. 2006;77:567–74.
Rosenbaum TG, Bloebaum RD, Ashrafi S, et al. Ambulatory activities maintain cortical bone after total hip arthroplasty. Clin Orthop Relat Res. 2006;450:129–37.
Lübbeke A, Stern R, Garavaglia G, et al. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum. 2007;57:327–34.
Powell KE, Blair SN. The public health burdens of sedentary living habits: theoretical but realistic estimates. Med Sci Sports Exerc. 1994;26:851–6.
WHO. International statistical classification of diseases and related health problems 10th revision version for 2007. http://apps.who.int/classifications/apps/icd/icd10online/.
Braeken AM, Lochhaas-Gerlach JA, Gollish JD, et al. Determinants of 6–12 month postoperative functional status and pain after elective total hip replacement. Int J Qual Health C. 1997;9:413–8.
Kessler S, Käfer W. Overweight and obesity: two predictors for worse early outcome in total hip replacement? Obesity. 2007;15:2840–5.
McCalden RW, Charron KD, MacDonald SJ, et al. Does morbid obesity affect the outcome of total hip replacement? An analysis of 3290 THRS. J Bone Joint Surg Br. 2011;93B:321–5.
Moran M, Walmsley P, Gray A, et al. Does body mass index affect the early outcome of primary total hip arthroplasty? J Arthroplast. 2005;20:866–9.
Stickles B, Phillips L, Brox WT, et al. Defining the relationship between obesity and total joint arthroplasty. Obes Res. 2001;9:219–23.
Andrew JG, Palan J, Kurup HV, et al. Obesity in total hip replacement. J Bone Joint Surg Br. 2008;90B:424–9.
Busato A, Roder C, Herren S, et al. Influence of high BMI on functional outcome after total hip arthroplasty. Obes Surg. 2008;18:595–600.
Jackson MP, Sexton SA, Yeung E, et al. The effect of obesity on the mid-term survival and clinical outcome of cementless total hip replacement. J Bone Joint Surg Br. 2009;91B:1296–300.
Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically-important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Rheumatol. 1988;15:1833–40.
Roorda LD, Jones CA, Waltz M, et al. Satisfactory cross cultural equivalence of the Dutch WOMAC in patients with hip osteoarthritis waiting for arthroplasty. Ann Rheum Dis. 2004;73:36–42.
McConnell S, Kolopack P, Davis AM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum. 2001;45:453–61.
Aaronson NK, Muller M, Cohen PD, et al. Translation, validation, and norming of the Dutch language version of the SF-36 health survey in community and chronic disease populations. J Clin Epidemiol. 1998;51:1055–68.
Nilsdotter AK, Peterson IF, Roos EM, et al. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Ann Rheum Dis. 2003;62:923–30.
Muthén LK, Muthén BO. Mplus user’s guide (1998–2007). 5th ed. Los Angeles: Muthén & Muthén; 2007.
Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arth Rheum Arthr. 2001;45:384–91.
Dekkers JC, van Wier MF, Hendriksen IJM, et al. Accuracy of self-reported body weight, height and waist circumference in a Dutch overweight working population. BMC Med Res Meth. 2008;8:69.
Competing Interests
The authors declare that they have no competing interests.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Stevens, M., Paans, N., Wagenmakers, R. et al. The Influence of Overweight/Obesity on Patient-Perceived Physical Functioning and Health-Related Quality of Life After Primary Total Hip Arthroplasty. OBES SURG 22, 523–529 (2012). https://doi.org/10.1007/s11695-011-0483-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-011-0483-1