Abstract
Three-dimensional (3D) cultures are becoming increasingly popular due to their ability to mimic tissuelike structures more effectively than monolayer cultures. In cancer research, the natural tumor characteristics and architecture are more closely mimicked by 3D cell models. Thus, 3D cell cultures are more promising and suitable models, particularly for in vitro drug screening to predict in vivo efficacy. Different methods have been developed to create 3D cell culture systems for research application. This review will introduce and discuss 3D cell culture methods most popularly used in drug screening. The potential applications of these systems in anticancer drug screening will also be discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
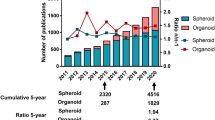
Cancer is one of leading causes of death worldwide with 14 million new cases and 8.2 million deaths in 2012 (2014). Numerous efforts have been aimed at finding new and more effective ways to treat cancer. Among these strategies is screening of anticancer drugs. Standard screening has typically been evaluated in animal models. However, some results have shown that animal experiments do not always predict clinical outcome in humans, especially with regard to toxicity assessments (Knight, 2008). Moreover, the use of animals for research is often restricted due to ethical concerns (Festing, 2007). In light of these issues, an in vitro cell-based model is great alternative, minimizing the need for and number of animal experiments. 2D cell culture was the first procedure established for cell-based screening assays. Although 2D cell culture methods are simple, quick and cost-effective to set up, and have been widely investigated, there remain many disadvantages. The primary disadvantage of a 2D system is that it does not mimic an actual 3D tumor and is not biologically relevant (Carrie J. Lovitt, 2014). Cells in the in vivoenvironment usually interact with neighboring cells and the extracellular matrix (ECM); however, 2D cell models cannot recapitulate those characteristics. Thus, a 2D culture model may be starkly different from an actual growing tumor with regards to cell morphology, cell proliferation, and gene and protein expression (Edmondson et al., 2014). As a result, only 10% of the drugs passed through in vitro testing have had a positive effect in the clinic, or led to drug approval. The percentage of anticancer drugs which have shown clinical efficacy is even lower, at about 5% (Westhouse, 2010). The high rate failure in the clinical testing phase is a waste of time and money. Therefore, it is important to identify promising in vitro culture models for evaluating drug efficacy in the early stages of drug discovery and development (Wong et al., 2012). Given the advantages of 3D versus 2D cell culture models, 3D cell culture techniques garnered increasing attention. The number of publications related to 3D cell cultures have rapidly increased in the last decade- from 7 publications in 1992 to 421 in 2013 (Ferro et al., 2014; Ravi et al., 2015). The 3D cell culture systems allow cell-based assays to be more physiologically relevant, particularly since cell behavior in 3D culture is much more similar to that of cells in in vivo tissues. In 3D models, cell-cell and cell- ECM interactions are maintained, such that cell morphology, proliferation, differentiation, migration, apoptosis, gene expression and protein expression are comparable to those of cells in vivo(Edmondson et al., 2014).
Why 3d culture?
Cell-based assays play a critical role in anticancer drug screening. Traditionally, 2D cell culture was widely used in cancer drug discovery. However, a large number of drugs reported to have strong anticancer effect in 2D cell culture models failed in clinical tests (Xu and Burg, 2007). In 2011, although approximately 900 antineoplastic agents had passed through cell-based assay testing, only 12 were approved by the FDA after clinical testing (America, 2011; Kantarjian et al., 2013).
In recent years, the potential and critical role of 3D cultures in cancer research have gained greater interest. Through the use of sophisticated 3D multicellular tumor spheroid (MCTS) systems, the microenvironment, phenotype and cellular heterogeneity of tumors are effectively represented (Thoma et al., 2014). MCTS systems create a gradient of oxygen and nutrients from the outside of tumor spheroids to the core. Spheroids in MCTS systems are constructed with different zones of cells, including proliferating cells on the outside, quiescent viable cells in the middle, and necrotic cells at the inner core (Fig. 1), which realistically mimic in vivo tumors (Ma et al., 2012). Many research studies have shown that the genotypic profile of cells in MCTS, versus cells grown in monolayer, are more similar to in vivo tumors (Smith et al., 2012). Cells in 3D culture conditions were found to exhibit gene expression profiles different to those grown in monolayer (Luca et al., 2013; Myungjin Lee et al., 2013). This may be a primary reason as to why results of anticancer drug assessments using MCTS are more predictive of clinical efficacy than 2D cell assessments (Carver et al., 2014).
Many antineoplastic agents have been reported to be less effective for cancer cells cultured in 3D than 2D (Frankel et al., 2000; Imamura et al., 2015; Karlsson et al., 2012). The architectural structure of MCTS is the main reason for this difference. Firstly, the 3D structure of MCTS reduces the number of cancer cells exposed to anticancer agents; these drugs have more accessibility to cells in monolayer culture (Carrie J. Lovitt, 2014). Secondly, the tightly adhered cells and ECM in MCTS can limit drug penetration (Frankel et al., 2000). Moreover, the hypoxic core generates a G0- dormant cell population which is highly resistant to chemotherapy (Imamura et al., 2015). Gene expression of cells cultured in 3D systems differs from that of cells in 2D monolayer; for instance, expression of genes related to chemoresistance has been found to vary from 3D versus 2D systems (Lin and Chang, 2008). Studies in breast cancer (Howes et al., 2014a) and colon cancer (Luca et al., 2013) have demonstrated decreased epidermal growth factor (EGFR) and human epidermal growth factor (HER) activation in cells cultured in 3D versus 2D. This could cause decreased sensitivity to anticancer drugs targeting EGFR and HE, and has been observed in 3D cell systems. On the other hand, some drugs show equal, or even greater, therapeutic effect in 3D models compared to 2D (Hongisto et al., 2013; Howes et al., 2007; Pickl and Ries, 2009). The absence of a hypoxic, necrotic core in 2D culture models makes cells more resistant to antineoplastic agents, which are effectively activated by hypoxic conditions of 3D tumors; tirapazamine (TPZ) is an example of this kind of drug (Tung et al., 2011). Given that 3D models not only mimic tumor architecture but mimic similar environmental challenges, these models are great and conservative systems to study candidate drug.
Although MCTS is still an in vitro model, its similarity to an in vivo tumor environment allows for a more accurate model to study drug efficacy while minimizing the cast of failed clinical trials.
Platforms of 3d cell culture systems used for anticancer drug screening
Due to the advantages of 3D culture systems, there have been many studies focused on the development and optimization of 3D cell culture technologies. Up until now, there have been several types of 3D culture modeis, same of which have been used for anticancer drug screening.
Liquid overlay culture
Liquid overlay culture (LOC) is the simplest method of 3D cell culture (Enmon et aI., 2001). To generate models, cell culture plates or flasks are covered with a thin layer of inert substrates, such as agar(Vinci et al., 2012), agarose (Friedrich et aI., 2009), polyHEMA(Friedrich et aI., 2007) or Matrigel(C. S. SHIN 2013). By preventing matrix deposition, LOC easily promotes 3D aggregates or sph eroids(Ca risson and Yuhas, 1984). This technique is low cost and highly reproducible without requirement of sophisticated equipment (Costa et aI., 2014). Different cell types can be co-cultured with this method (Metzger et a1.). However, it is difficult to monitor the number and size of formed spheroids (Lin and Chang, 2008).
Ultra-low attachment plates have been developed as the commercial product of the liquid overlay technique, bypassing the requirement for manual coating. Dishes are designed with a layer of hydrophilic polymer inside, which prevents cells from attaching to the surface. This technique can overcome the limit of culture in gel, has the potential to produce one spheroid per well, and is suitable for medium-throughput screening (Thoma et al., 2014).
Hanging drop
The hanging drop technique was first developed by Johannes Holtfreter in 1944 for culivating embryonic stem cells. lt has also become the foundation of the non-scaffold method for the multicellular spheroid generalion. In the beginning, the petri dish lid was used to generate spheroids by dropping a small volume of cell suspension (15- 30 μL) onto the lid and then inverting it. Due to surface tension, droplets were maintained and cells in the drop lets spontaneously aggregated to form spheroids (Lin and Chang, 2005). Today, there are many types of commercial devices designed for hanging drop cultures (Fig. 2).
The general structure of a hanging drop plate (a). Hanging drop formation process (b). (Image souree: www.3dbiomatrix.com).
This technique has many advantages, including being cost-effective, easy to generate one spheroid per well, and easy to control the size of spheroids. Moreover, different cell types can be cocultured and generated into spheroids at high-throughput using liquid handling systems (Hsiao et al., 2012; Kelm et al., 2003; Pham, 2015; Yip and Cho, 2013). However, it is difficult to maintain spheroids and change the medium due to the limited volume of drop lets (Mehta et al., 2012).
Microtechnology
In the last few years, microtechnologies have attracted the attention of scientists, particularly with regard to the use of microtechniques to generate 3D cell models (Hirschhaeuser et al., 2010).
The photolithography technique is one exampleand used to create micropattem surface plates with special surfaces, including attaching and non-attaching areas. Seeded cells are guided to grow and farm 3D structureson the adhesion islands. The size and shape of spheroids rely on the design of the attachment sites (Fig. 3 ) (Degot et al., 2010).
Microwell plates are designed with the bottom containing a large number of microsize chambers, which vary in shape, e.g. round, square, honeycomb, slit and multiple pores(Larson, 2015) (Fig. 4 ). Under gravity and hydrodynamic forces, cells are located in tiny wells and then concentrated to form 30 structure with dimensions and geometry specific to each type of microwell (Karp et al., 2007).
Microtechnologies, including microwells and micropattern surfaces, are promising for producing mass production of controlled sized spheroids. It is possible to co-culture different type of cells through the requirement of special and expensive equipment (Lin and Chang, 200S).
Bioreactor
When the important role of 3D cultures in testing chemical effects of anticancer drugs was discovered, scale-up screening from laboratory to industrial scale became a critical next step. Bioreactors became part of the standard process for spheroid generation as they provided greater production control and reproducibility (Ou and Hosseinkhani, 2014). In a typical process, spheroids are formed in bioreactors via continuous moving fluid (Breslin and O'Driscoll, 2013). The dynamic culture condition is mainly created by stirring (spinner flask) or rotating (NASA rotating wall vessel) (c. S. SHIN 2013).
The modern glass spinner flask was first developed by W.F. McLimans in 1957 (Mc et al., 1957). Cell suspension was contained in flasks, which were designed with two arms and could be opened for gas exchange; a stir bar was used for stirring the fluid (Delphine Antoni 2015) (Fig. 5a ). In 1990, rotating wall vessels (RWVs) were made for cell culture by NASA (National Aeronautics and Space Administration) (K. C. O'Connor', 2013). RWVs are constructed of an inner cylinder, a chamber of rotating concentric cylinders for growing cells, and a membrane for gas exchange (Rauh et al., 2011) (Fig. b ). The low shear environment of RWVs creates larger sized spheroids than spinner flasks (Lelkes and Cherian, 1995). HepG2 spheroids formed in RWVs reach 100 μm in diameter after 72 h of culture and up to 1 mm in diameter after long-term culture (Chang and Hughes-Fulford, 2009).
Components of a general bioreactor. Spinner flask (a) (Image source: www.sigmaaldrich.com) and NASA rotating wall vessel (b) (Image source: www.genengnews.com).
Bioreactors are labor-intensive due to their ability to produce a large number of spheroids (Tostoes et al., 2012). However, the created spheroids are usually heterogeneous in size and cell population (Mehta et al., 2012). Therefore, a manual selection would be required afterward to select suitably sized spheroids for re-plating onto dishes for drug screening assays, if the similarity of spheroid size is required (Breslin and O'Driscoll, 2013). Although generation of spheroids via bioreactors requires expensive instruments (Kim et al., 2004) and high quality of medium, the advantages of bioreactors for long-term culture is undeniable (Ebrahimkhani et al., 2014).
Applications in anticancer drug screening
Cell culture systems have long been a foundation for testing and comparing the cytotoxicity and pharmacodynamics of anticancer drug candidates. Even now, many results from 3D cell culture have consistently stressed the importance of these models in drug screening. Research by Jayme L. Horning et al., published in 2008, indicated that 3D MCF7 cells were more resistant to many popular anticancer drugs (e.g. doxorubicin, paclitaxel and tamoxifen) compared with MCF7 cells cultured in monolayer. Using polymeric microparticle surfaces to create 3D tumors, they found that 2D MCF7 cells were significantly more sensitive to these drugs than 3D MCF7 cells, with a 12- to 23- fold disparity in the IC50 values. The study also showed that the sum of collagen in the 3D model was 2 times greater than that of 2D condition and the expression of many genes were different, possibly accounting for the difference in responses to the drugs (Horning et al., 2008). Vesa Hongisto et al. suggested in their 2013 studies that 3D cell models can effectively replace traditional 2D cell monolayers and that with regard to screening of drug compounds, 3D models provide better comparability to clinical results. In their study, 102 compounds were tested on JIMT1 breast cancer cells. Results showed that JIMT1 cells were significantly more sensitive to 63 compounds when cultured on Matrigel as compared to 2D condition (Hongisto et al., 2013). Using 96-well roundbottom ultra-low attachment plates to create 3D cancer tumors, Amy L. Howes et al. showed, from their studies in 2014, that 3D BT-474 cells were more sensitive to lapatinib, gefitinib, vinblastine and vinorelbine than 3D MCF-10A cells. The authors also found that microtubule-targeting agents and epidermal growth factor receptor (EGFR) inhibitors are two classes of compounds to have selective effects on cancer cells in 3D culture (Howes et al., 2014b). Work by Yukie Yoshii et al., published in 2016, on human colon cancer HCT116 cell line demonstrated that regorafenib was most effective on 3D HCT116- RFP cells among 8 drugs tested (capecitabine, bevacizumab, irinotecan, cetuximab, 5-fluorouracil (5- FU), panitumumab, oxaliplatin and regorafenib). Based on their 3D culture studies, the authors were able to demonstrate effective and non-effective drugs for colon cancer treatment (Yoshii et al., 2016).
Conclusion
Anticancer drug screening is an important component in the fight against cancer. Several 3D cell culture systems have been developed as suitable platforms for drug screening and are serve as more reliable models for in vitro testing, compared to 2D, given that MCTS have greater structural similarity and cellular zone components to in vivo tumors. The 3D model systems should provide more accurate results for prediction of clinical outcome. Tremendous efforts have been made to establish various 3D cell culture systems. It is important for researchers to look carefully at the advantages and disadvantages of each to find the most suitable system for their studies. However, all the 3D systems can be utilized for cancer research, particularly for testing of new anticancer agents.
References
America, P.R.a.M.o. (2011). Medicines in Development for Cancer.
Breslin, S., and O’Driscoll, L. (2013). Three-dimensional cel culture: the missing link in drug discovery. Drug discovery today 18, 240–249.
C. S. SHIN, B.K., B. HAN, K. PARK and A. PANITCH (2013). 3D cancer tumor models for evaluating chemotherapeutic efficacy. Carlsson, J., and Yuhas, J.M. (1984). Liquid-overlay culture of cellular spheroids. Recent results in cancer research Fortschritte der Krebsforschung Progres dans les recherches sur le cancer 95, 1–23.
Carrie J. Lovitt, T.B.S.a.V.M.A. (2014). Advanced Cell Culture Techniques for Cancer Drug Discovery.
Carver, K., Ming, X., and Juliano, R.L. (2014). Multicellular Tumor Spheroids as a Model for Assessing Delivery of Oligonucleotides in Three Dimensions. Mol Ther Nucleic Acids 3, e153.
Chang, T.T., and Hughes-Fulford, M. (2009). Monolayer and spheroid culture of human liver hepatocellular carcinoma cell line cells demonstrate distinct global gene expression patterns and functional phenotypes. Tissue engineering Part A 15, 559–567.
Costa, E.C., Gaspar, V.M., Coutinho, P., and Correia, I.J. (2014). Optimization of liquid overlay technique to formulate heterogenic 3D co-cultures models. Biotechnology and bioengineering 111, 1672–1685.
Degot, S., Auzan, M., Chapuis, V., Béghin, A., Chadeyras, A., Nelep, C., Calvo-Muñoz, M.L., Young, J., Chatelain, F., and Fuchs, A. (2010). Improved Visualization and Quantitative Analysis of Drug Effects Using Micropatterned Cells. Journal of Visualized Experiments: JoVE.
Delphine Antoni, H.B., Elodie Josset and Georges Noel (2015). Three-Dimensional Cell Culture: A Breakthrough in Vivo. International journal of molecular sciences.
Ebrahimkhani, M.R., Neiman, J.A.S., Raredon, M.S.B., Hughes, D.J., and Griffith, L.G. (2014). Bioreactor Technologies to Support Liver Function In Vitro. Advanced drug delivery reviews 0, 132–157.
Edmondson, R., Broglie, J.J., Adcock, A.F., and Yang, L. (2014). Three-Dimensional Cell Culture Systems and Their Applications in Drug Discovery and Cell-Based Biosensors. Assay and Drug Development Technologies 12, 207–218.
Enmon, R.M., Jr., O’Connor, K.C., Lacks, D.J., Schwartz, D.K., and Dotson, R.S. (2001). Dynamics of spheroid self-assembly in liquid-overlay culture of DU 145 human prostate cancer cells. Biotechnology and bioengineering 72, 579–591.
Ferro, F., Shields Baheney, C., and Spelat, R. (2014). Three- Dimensional (3D) Cell Culture Conditions, Present and Future Improvements. Razavi Int J Med 2, e17803.
Festing, S. (2007). The ethics of animal research. Talking Point on the use of animals in scientific research. 8, 526–530.
Frankel, A., Man, S., Elliott, P., Adams, J., and Kerbel, R.S. (2000). Lack of multicellular drug resistance observed in human ovarian and prostate carcinoma treated with the proteasome inhibitor PS-341. Clinical cancer research: an official journal of the American Association for Cancer Research 6, 3719–3728.
Friedrich, J., Ebner, R., and Kunz-Schughart, L.A. (2007). Experimental anti-tumor therapy in 3-D: spheroids–old hat or new challenge? International journal of radiation biology 83, 849–871.
Friedrich, J., Seidel, C., Ebner, R., and Kunz-Schughart, L.A. (2009). Spheroid-based drug screen: considerations and practical approach. Nature protocols 4, 309–324.
Hirschhaeuser, F., Menne, H., Dittfeld, C., West, J., Mueller- Klieser, W., and Kunz-Schughart, L.A. (2010). Multicellular tumor spheroids: an underestimated tool is catching up again. Journal of biotechnology 148, 3–15.
Hongisto, V., Jernstrom, S., Fey, V., Mpindi, J.P., Kleivi Sahlberg, K., Kallioniemi, O., and Perala, M. (2013). Highthroughput 3D screening reveals differences in drug sensitivities between culture models of JIMT1 breast cancer cells. PloS one 8, e77232.
Horning, J.L., Sahoo, S.K., Vijayaraghavalu, S., Dimitrijevic, S., Vasir, J.K., Jain, T.K., Panda, A.K., and Labhasetwar, V. (2008). 3-D tumor model for in vitro evaluation of anticancer drugs. Molecular pharmaceutics 5, 849–862.
Howes, A.L., Chiang, G.G., Lang, E.S., Ho, C.B., Powis, G., Vuori, K., and Abraham, R.T. (2007). The phosphatidylinositol 3- kinase inhibitor, PX-866, is a potent inhibitor of cancer cell motility and growth in three-dimensional cultures. Molecular cancer therapeutics 6, 2505–2514.
Howes, A.L., Richardson, R.D., Finlay, D., and Vuori, K. (2014a). 3-Dimensional Culture Systems for Anti-Cancer Compound Profiling and High-Throughput Screening Reveal Increases in EGFR Inhibitor-Mediated Cytotoxicity Compared to Monolayer Culture Systems. PloS one 9.
Howes, A.L., Richardson, R.D., Finlay, D., and Vuori, K. (2014b). 3-Dimensional culture systems for anti-cancer compound profiling and high-throughput screening reveal increases in EGFR inhibitor-mediated cytotoxicity compared to monolayer culture systems. PloS one 9, e108283.
Hsiao, A.Y., Tung, Y.C., Qu, X., Patel, L.R., Pienta, K.J., and Takayama, S. (2012). 384 hanging drop arrays give excellent Zfactors and allow versatile formation of co-culture spheroids. Biotechnology and bioengineering 109, 1293–1304.
Imamura, Y., Mukohara, T., Shimono, Y., Funakoshi, Y., Chayahara, N., Toyoda, M., Kiyota, N., Takao, S., Kono, S., Nakatsura, T., et al. (2015). Comparison of 2D- and 3D-culture models as drug-testing platforms in breast cancer. Oncology reports 33, 1837–1843.
K. C. O’Connor’, T.L.P., T. J. Goodwinft, K. M. Francis’, A. D. Andrews’ and G. F. Spauldingff (2013). Animal cell cultivation in the NASA roating wall vessel.
Karlsson, H., Fryknas, M., Larsson, R., and Nygren, P. (2012). Loss of cancer drug activity in colon cancer HCT-116 cells during spheroid formation in a new 3-D spheroid cell culture system. Experimental cell research 318, 1577–1585.
Karp, J.M., Yeh, J., Eng, G., Fukuda, J., Blumling, J., Suh, K.Y., Cheng, J., Mahdavi, A., Borenstein, J., Langer, R., et al. (2007). Controlling size, shape and homogeneity of embryoid bodies using poly(ethylene glycol) microwells. Lab on a chip 7, 786–794.
Kelm, J.M., Timmins, N.E., Brown, C.J., Fussenegger, M., and Nielsen, L.K. (2003). Method for generation of homogeneous multicellular tumor spheroids applicable to a wide variety of cell types. Biotechnology and bioengineering 83, 173–180.
Kim, J.B., Stein, R., and O’Hare, M.J. (2004). Three-dimensional in vitro tissue culture models of breast cancer– a review. Breast cancer research and treatment 85, 281–291.
Knight, A. (2008). Systematic reviews of animal experiments demonstrate poor contributions toward human healthcare. Reviews on recent clinical trials 3, 89–96.
Larson, B. (2015). 3D Cell Culture: A Review of Current Techniques.
Lelkes, P.I., Galvan, D. L., Thomas Hayman, G., Goodwin, T. J., Chatman, D. Y., and Cherian, S., Garcia, R. M. G. and Unsworth, B. R. (1998). Simulated microgravity conditions enhance differentiation of cultured PC12 cells towards the neuroendocrine phenotype. In Vitro Cell Dev Biol-Anim.
Lin, R.Z., and Chang, H.Y. (2008). Recent advances in threedimensional multicellular spheroid culture for biomedical research. Biotechnology journal 3, 1172–1184.
Luca, A.C., Mersch, S., Deenen, R., Schmidt, S., Messner, I., Schafer, K.L., Baldus, S.E., Huckenbeck, W., Piekorz, R.P., Knoefel, W.T., et al. (2013). Impact of the 3D microenvironment on phenotype, gene expression, and EGFR inhibition of colorectal cancer cell lines. PloS one 8, e59689.
Ma, H.L., Jiang, Q., Han, S., Wu, Y., Cui Tomshine, J., Wang, D., Gan, Y., Zou, G., and Liang, X.J. (2012). Multicellular tumor spheroids as an in vivo-like tumor model for three-dimensional imaging of chemotherapeutic and nano material cellular penetration. Molecular imaging 11, 487–498.
Mc, L.W., Davis, E.V., Glover, F.L., and Rake, G.W. (1957). The submerged culture of mammalian cells; the spinner culture. Journal of immunology (Baltimore, Md: 1950) 79, 428–433.
Mehta, G., Hsiao, A.Y., Ingram, M., Luker, G.D., and Takayama, S. (2012). Opportunities and Challenges for use of Tumor Spheroids as Models to Test Drug Delivery and Efficacy. Journal of controlled release: official journal of the Controlled Release Society 164, 192–204.
Metzger, W., Sossong, D., Bächle, A., Pütz, N., Wennemuth, G., Pohlemann, T., and Oberringer, M. The liquid overlay technique is the key to formation of co-culture spheroids consisting of primary osteoblasts, fibroblasts and endothelial cells. Cytotherapy 13, 1000–1012.
Myungjin Lee, J., Mhawech-Fauceglia, P., Lee, N., Cristina Parsanian, L., Gail Lin, Y., Andrew Gayther, S., and Lawrenson, K. (2013). A three-dimensional microenvironment alters protein expression and chemosensitivity of epithelial ovarian cancer cells in vitro. Lab Invest 93, 528–542.
Ou, K.L., and Hosseinkhani, H. (2014). Development of 3D in vitro technology for medical applications. International journal of molecular sciences 15, 17938–17962.
Pham, P. (2015). Breast Cancer Stem Cell Culture and Proliferation. In Breast Cancer Stem Cells & Therapy Resistance (Cham: Springer International Publishing), pp. 41–55.
Pickl, M., and Ries, C.H. (2009). Comparison of 3D and 2D tumor models reveals enhanced HER2 activation in 3D associated with an increased response to trastuzumab. Oncogene 28, 461–468.
Rauh, J., Milan, F., Gunther, K.P., and Stiehler, M. (2011). Bioreactor systems for bone tissue engineering. Tissue engineering Part B, Reviews 17, 263–280.
Ravi, M., Paramesh, V., Kaviya, S.R., Anuradha, E., and Solomon, F.D. (2015). 3D cell culture systems: advantages and applications. Journal of cellular physiology 230, 16–26.
Smith, S.J., Wilson, M., Ward, J.H., Rahman, C.V., Peet, A.C., Macarthur, D.C., Rose, F.R., Grundy, R.G., and Rahman, R. (2012). Recapitulation of tumor heterogeneity and molecular signatures in a 3D brain cancer model with decreased sensitivity to histone deacetylase inhibition. PloS one 7, e52335.
Thoma, C.R., Zimmermann, M., Agarkova, I., Kelm, J.M., and Krek, W. (2014). 3D cell culture systems modeling tumor growth determinants in cancer target discovery. Advanced drug delivery reviews 69–70, 29–41.
Tostoes, R.M., Leite, S.B., Serra, M., Jensen, J., Bjorquist, P., Carrondo, M.J., Brito, C., and Alves, P.M. (2012). Human liver cell spheroids in extended perfusion bioreactor culture for repeated-dose drug testing. Hepatology (Baltimore, Md) 55, 1227–1236.
Tung, Y.C., Hsiao, A.Y., Allen, S.G., Torisawa, Y.S., Ho, M., and Takayama, S. (2011). High-throughput 3D spheroid culture and drug testing using a 384 hanging drop array. The Analyst 136, 473–478.
Vinci, M., Gowan, S., Boxall, F., Patterson, L., Zimmermann, M., Court, W., Lomas, C., Mendiola, M., Hardisson, D., and Eccles, S.A. (2012). Advances in establishment and analysis of three-dimensional tumor spheroid-based functional assays for target validation and drug evaluation. BMC Biology 10, 29.
Westhouse, R.A. (2010). Safety assessment considerations and strategies for targeted small molecule cancer therapeutics in drug discovery. Toxicologic pathology 38, 165–168.
Wong, C.C., Cheng, K.W., and Rigas, B. (2012). Preclinical Predictors of Anticancer Drug Efficacy: Critical Assessment with Emphasis on Whether Nanomolar Potency Should Be Required of Candidate Agents. The Journal of Pharmacology and Experimental Therapeutics 341, 572–578.
Xu, F., and Burg, K.J.L. (2007). Three-dimensional polymeric systems for cancer cell studies. Cytotechnology 54, 135–143.
Yip, D., and Cho, C.H. (2013). A multicellular 3D heterospheroid model of liver tumor and stromal cells in collagen gel for anti-cancer drug testing. Biochemical and biophysical research communications 433, 327–332.
Yoshii, Y., Furukawa, T., Aoyama, H., Adachi, N., Zhang, M.R., Wakizaka, H., Fujibayashi, Y., and Saga, T. (2016). Regorafenib as a potential adjuvant chemotherapy agent in disseminated small colon cancer: Drug selection outcome of a novel screening system using nanoimprinting 3-dimensional culture with HCT116-RFP cells. International journal of oncology 48, 1477–1484.
Kantarjian, H.M., Fojo, T., Mathisen, M., and Zwelling, L.A. (2013). Cancer drugs in the United States: Justum Pretium—the just price. Journal of Clinical Oncology 31, 3600–3604.
Cite this article as:
Nguyen, H., Nguyen, S., & Pham, P. (2016). Concise review: 3D cell culture systems for anticancer drug screening. Biomedical Research and Therapy, 3(5), 625-632.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding and grants
This research was funded by Vietnam National University, Ho Chi Minh city, Viet Nam under grant number A2015-18-01/HD-KHCN
Competing interests
The authors declare that they have no competing interests.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nguyen, HL., Nguyen, S. & Van Pham, P. Concise Review: 3D cell culture systems for anticancer drug screening. Biomed Res Ther 3, 22 (2016). https://doi.org/10.7603/s40730-016-0022-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.7603/s40730-016-0022-8