Abstract
Background
Noncontiguous cervical spondylotic myelopathy (CSM) is a special degenerative disease because of the intermediate normal level or levels between supra and infraabnormal levels. Some controversy exists over the optimal procedure for two noncontiguous levels of CSM. The study was to evaluate the outcomes of the anterior cervical discectomy and fusion (ACDF) with zero-profle devices for two noncontiguous levels of CSM.
Materials and Methods
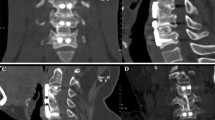
17 consecutive patients with two noncontiguous levels of CSM operated between December 2009 and August 2012 were included in the study. There were 12 men and 5 women with a mean age of 60.7 years (range 45–75 years). Involved disc levels were C3/4 and C5/6 in 11 patients and C4/5 and C6/7 in six patients. Preoperative plain radiographs, computed tomography (CT) with 3-D reconstruction and magnetic resonance imaging (MRI) of the cervical spine were taken in all patients. All radiographs were independently evaluated by 2 spine surgeons and 1 radiologist. The outcomes were assessed by the average operative time, blood loss, Japanese Orthopedic Association (JOA) score, improvement rate, neck dysfunction index (NDI), swallowing quality of life (SWAL-QOL) score, the cervical lordosis and complications.
Results
The mean followup was 48.59 months (range 24-56 months). The average operative time and blood loss was 105.29 min and 136.47 ml, respectively. The preoperative JOA score was 8.35, which signifcantly increased to 13.7 at the fnal followup (P < 0.01). The NDI score was signifcantly decreased from preoperative 13.06 to postoperative 3.35 (P < 0.01). The operation also provided a signifcant increase in the cervical lordosis (P < 0.01) from preoperative 10.17° to postoperative 17.06°. The fusion rate was 94.1% at 6 months postoperatively, and 100% at 12 months after surgery. The mean SWAL-QOL score decreased from preoperative 68.06 to immediate postoperatively 65.65 and then increased to 67.65 at fnal followup. There was a statistically signifcant difference between preoperative and immediate postoperatively values (P < 0.05), but none between preoperative and at fnal followup (P < 0.05). Cerebrospinal fuid leak, dysphagia and radiological adjacent segment degeneration occurred in one patient, respectively.
Conclusion
The ACDF with zero-profle devices is generally effective and safe in treating two noncontiguous levels of CSM.
Similar content being viewed by others
References
Cho SK, Riew KD. Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg 2013;21:3–11.
Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310–7.
Scholzl M, Reyes PM, Schleicherl P, Sawa AG, Baekl S, Kandzioral F, et al. A new stand-alone cervical anterior interbody fusion device: Biomechanical comparison with established anterior cervical fixation devices. Spine (Phila Pa 1976) 2009;34:156–60.
Qizhil S, Xueleil W, Lilil Y, Leil L, Linweil C, Yangl L, et al. Segmental anterior decompression and fusion for multilevel ossification of the posterior longitudinal ligament. Orthopedics 2012;35:e403–8.
Robertson JT, Papadopoulos SM, Traynelis VC. Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: A prospective 2-year study. J Neurosurg Spine 2005;3:417–23.
Kim SW, Limson MA, Kim SB, Arbatin JJ, Chang KY, Park MS, et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. Eur Spine J 2009;18:218–31.
Siska PA, Ponnappan RK, Hohl JB, Lee JY, Kang JD, Donaldson WF 3rd. Dysphagia after anterior cervical spine surgery: A prospective study using the swallowing-quality of life questionnaire and analysis of patient comorbidities. Spine (Phila Pa 1976) 2011;36:1387–91.
Matsumotol M, Okadal E, Ichiharal D, Watanabel K, Chibal K, Toyamal Y, et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: Comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging followup study. Spine (Phila Pa 1976) 2010;35:36–43.
Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002;27:2431–4.
Lopez-Espina CG, Amirouchel F, Havaladl V. Multilevel cervical fusion and its effect on disc degeneration and osteophyte formation. Spine (Phila Pa 1976) 2006;31:972–8.
Gaol Y, Liul M, Lil T, Huangl F, Tangl T, Xiangl Z. A meta-analysis comparing the results of cervical disc arthroplasty with anterior cervical discectomy and fusion (ACDF) for the treatment of symptomatic cervical disc disease. J Bone Joint Surg Am 2013;95:555–61.
Park DH, Ramakrishnanl P, Cho TH, Lorenzl E, Eck JC, Humphreys SC, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine 2007;7:336–40.
Finn MA, Samuelson MM, Bishopl F, Bachus KN, Brodke DS. Two-level noncontiguous versus three-level anterior cervical discectomy and fusion: A biomechanical comparison. Spine (Phila Pa 1976) 2011;36:448–53.
Ji GY, Oh CH, Shin DA, Hal Y, Kim KN, Yoon dol H, et al. Stand¬alone cervical cages versus anterior cervical plates in 2-level cervical anterior interbody fusion patients: Analysis of adjacent segment degeneration. J Spinal Disord Tech 2015;28:E433–8.
Yue WM, Brodnerl W, Highland TR. Persistent swallowing and voice problems after anterior cervical discectomy and fusion with allograft and plating: A 5 to 11 year followup study. Eur Spine J 2005;14:677–82.
Lee MJ, Bazazl R, Furey CG, Yool J. Influence of anterior cervical plate design on Dysphagia: A 2-year prospective longitudinal followup study. J Spinal Disord Tech 2005;18:406–9.
Chin KR, Eiszner JR, Adams SB Jr. Role of plate thickness as a cause of dysphagia after anterior cervical fusion. Spine (Phila Pa 1976) 2007;32:2585–90.
Papaverol L, Heesel O, Klotz-Regenerl V, Buchallal R, Schröderl F, Westphall M. The impact of esophagus retraction on early dysphagia after anterior cervical surgery: Does a correlation exist? Spine (Phila Pa 1976) 2007;32:1089–93.
Mendoza-Lattesl S, Cliffordl K, Barteltl R, Stewartl J, Clark CR, Boezaart AP. Dysphagia following anterior cervical arthrodesis is associated with continuous, strong retraction of the esophagus. J Bone Joint Surg Am 2008;90:256–63.
Kang SH, Kim DK, Seo KM, Kim KT, Kim YB. Multi-level spinal fusion and postoperative prevertebral thickness increase the risk of dysphagia after anterior cervical spine surgery. J Clin Neurosci 2011;18:1369–73.
Scholzl M, Schnake KJ, Pingel A, Hoffmannl R, Kandzioral F. A new zero-profile implant for stand-alone anterior cervical interbody fusion. Clin Orthop Relat Res 2011;469:666–73.
Kepler CK, Rihn JA, Bennett JD, Anderson DG, Vaccaro AR, Albert TJ, et al. Dysphagia and soft-tissue swelling after anterior cervical surgery: A radiographic analysis. Spine J 2012;12:639–44.
Riley LH 3rd, Skolasky RL, Albert TJ, Vaccaro AR, Heller JG. Dysphagia after anterior cervical decompression and fusion: Prevalence and risk factors from a longitudinal cohort study. Spine (Phila Pa 1976) 2005;30:2564–9.
Rihn JA, Kanel J, Albert TJ, Vaccaro AR, Hilibrand AS. What is the incidence and severity of dysphagia after anterior cervical surgery? Clin Orthop Relat Res 2011;469:658–65.
McAfee PC, Cappuccinol A, Cunningham BW, Devine JG, Phillips FM, Regan JJ, et al. Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech 2010;23:1–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qizhi, S., Peijia, L., Lei, S. et al. Anterior cervical discectomy and fusion for noncontiguous cervical spondylotic myelopathy. IJOO 50, 390–396 (2016). https://doi.org/10.4103/0019-5413.185603
Published:
Issue Date:
DOI: https://doi.org/10.4103/0019-5413.185603
Key words
- Cervical spondylotic myelopathy
- noncontiguous levels
- zero-profle devices
- anterior cervical decompression
- anterior cervical fusion