Abstract
Toll-like receptor 4 (TLR4) is ubiquitously expressed on parenchymal and immune cells of the liver and is the most studied TLR responsible for the activation of proinflammatory signaling cascades in liver ischemia and reperfusion (I/R). Since pharmacological inhibition of TLR4 during the sterile inflammatory response of I/R has not been studied, we sought to determine whether eritoran, a TLR4 antagonist trialed in sepsis, could block hepatic TLR4-mediated inflammation and end organ damage. When C57BL/6 mice were pretreated with eritoran and subjected to warm liver I/R, there was significantly less hepatocellular injury compared to control counterparts. Additionally, we found that eritoran is protective in liver I/R through inhibition of high-mobility group box protein B1 (HMGB1)-mediated inflammatory signaling. When eritoran was administered in conjunction with recombinant HMGB1 during liver I/R, there was significantly less injury, suggesting that eritoran blocks the HMGB1-TLR4 interaction. Not only does eritoran attenuate TLR4-dependent HMGB1 release in vivo, but this TLR4 antagonist also dampened HMGB1’s release from hypoxic hepatocytes in vitro and thereby weakened HMGB1’s activation of innate immune cells. HMGB1 signaling through TLR4 makes an important contribution to the inflammatory response seen after liver I/R. This study demonstrates that novel blockade of HMGB1 by the TLR4 antagonist eritoran leads to the amelioration of liver injury.
Similar content being viewed by others
Introduction
Hepatic ischemia and reperfusion (I/R) injury has potentially negative clinical implications for patients undergoing liver resection, transplantation and trauma. It is characterized by direct cellular damage as a result of the ischemic insult, as well as delayed dysfunction and damage that results from the activation of inflammatory pathways (1). The mechanism of this injury response has been extensively studied and is associated with the activation of pattern recognition receptors such as toll-like receptor 4 (TLR4) by endogenous ligands (2–5). TLR4-deficient mice have decreased levels of inflammatory cytokines and are significantly protected after liver I/R injury (5–7). It is well known that TLR4 plays a proinflammatory role in liver I/R through the activation of myeloid differentiation primary response 88 (Myd88), interferon regulatory factor 3 (IRF3), mitogen-activated protein kinase (MAPK) and inflammatory cytokines (3,5). Ultimately, activation of TLR4 by endogenous and exogenous ligands leads to hepatocellular apoptosis and necrosis, liver failure and organ injury.
Interest in TLR4 antagonism originated from sepsis studies, since TLR4 is known to bind to the gram-negative lipopolysaccharide (LPS) or endotoxin (8). Eritoran tetrasodium (E5564; Eisai, Andover, MA, USA) is a synthetic lipid A analog of Rhodobacter sphaeroides that has been designed to antagonize the effects of LPS through TLR4 (8–11). Eritoran does not directly interact with TLR4, but competes with LPS for binding to the hydrophobic pocket of the MD2 portion of the TLR4 receptor complex (9). It has been shown that eritoran binding to the TLR4/MD2 complex blocks the activation of nuclear factor (NF)-κB and production of inflammatory mediators such as tumor necrosis factor (TNF)-α and interleukin (IL)-6, both in vivo and in vitro, in response to LPS (9–15). Eritoran was investigated as a possible treatment of sepsis. Unfortunately, the large phase III multicenter ACCESS Randomized Trial failed to show a difference in the 28-d all-cause mortality in septic patients who received eritoran compared with placebo (16). Because TLR4 is also involved in sterile inflammation, eritoran has been tested in models of noninfectious pathobiology and has been shown to be beneficial (17–21). We hypothesized that TLR4 antagonists, such as eritoran, would provide a similar protection after warm hepatic I/R, which is heavily TLR4 mediated.
High-mobility group box protein B1 (HMGB1) is an important damage-associated molecular pattern (DAMP) molecule found in the nucleus of most eukaryotic cells, displays cytokine like activity and mediates sterile inflammation by binding to MD2 in the TLR4 receptor complex (22–25). During liver I/R, HMGB1 is released passively from necrotic cells and can be actively secreted from multiple cell types (22,26). Once bound to TLR4, HMGB1 activates an intracellular signaling cascade that involves recruiting MyD88, IL-1 receptor-associated kinase (IRAK-1), activating MAPK pathways and NF-κB translocation (22,26). HMGB1, like LPS, promotes inflammation, cell death and organ injury. We have previously shown that HMGB1 is a key mediator of liver I/R injury via its interaction with TLR4 (22).
In our study, we sought to determine whether eritoran blocks TLR4 signaling, subsequent inflammatory cascades and end-organ damage. We hypothesized that pharmacological inhibition of TLR4 with eritoran would antagonize the interaction between HMGB1 and TLR4, since HMGB1 binding to TLR4 contributes significantly to the injury response associated with liver I/R. We found that eritoran is protective in liver I/R through inhibition of HMGB1-mediated inflammatory responses. Overall, our investigations reveal a dominant role for the TLR4 antagonist, eritoran, in ameliorating liver I/R injury.
Materials and Methods
Materials
Eritoran tetrasodium (E5564) was obtained from Eisai, Inc., and prepared in phosphate-buffered saline (PBS). A dose of 5 mg/kg eritoran was used in vivo (dosage adopted from Shimamoto et al. [19]) and 8 ng/mL for in vitro experiments.
Animals
Male C57BL/6 mice, weighing 20–30 g, were purchased from The Jackson Laboratory (Bar Harbor, ME, USA) and used for experiments at the age of 8–12 wks. Housing conditions and access to food and water were the same for all mice. All animal protocols were approved by the Animal Care and Use Committee of the University of Pittsburgh. Experimental protocols were followed in strict adherence to the regulations set forth by the National Institutes of Health (NIH) guidelines for the use of laboratory animals (27).
Liver I/R
A hepatic warm ischemia and reperfusion model was used as previously described (28). In brief, a midline laparotomy incision was made, the blood supply to the left and median lobes of the liver were occluded with a microvascular clamp for 60 min and then 1 or 6 h of reperfusion was initiated once the clamp was removed. Sham animals had anesthesia and a laparotomy incision with exposure of the portal triad, without clamping. After 6 h of reperfusion, the mice were killed. The ischemic portions of the liver tissue were collected for Western blot, polymerase chain reaction (PCR), histological, and immunofluorescent analysis. Of note, mice received either eritoran (5 mg/kg) or vehicle control intraperitoneally 30 min before ischemia and recombinant HMGB1 (25 µL/mouse) injected intraperitoneally before the initiation of reperfusion.
Isolation, Culture and Treatment of Hepatocytes and RAW 264.7 Cells In Vitro
Murine macrophages of the RAW 264.7 cell line (donated from Matthew Rosengart’s laboratory, University of Pittsburgh) were cultured in Dulbecco’s modified Eagle medium (DMEM) supplemented with 7.5 mL 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES), 5 mL l-glutamine, 5 mL penicillin-streptomycin and 25 mL fetal bovine serum. RAW 264.7 cells were scraped and resuspended at a concentration of 1 × 106 cells/mL per well of a six-well plate. Cells were allowed to adhere overnight. Before each experiment, cells were washed with PBS, and new media were placed into the wells. RAW 264.7 cells were incubated with LPS (1 µg/mL), eritoran (8 ng/mL) and/or recombinant HMGB1 in the disulfide form (1 µg/mL, donated from Timothy Billiar’s laboratory, University of Pittsburgh) for 18 h. All treatments were performed in duplicate. After the incubation period, the media and cells were collected for analysis.
Hepatocytes were cultured in Williams E. Medium containing 10% calf serum, 15 mmol/L HEPES, 2 mmol/L l-glutamine and 100 U/mL penicillin and streptomycin. Hepatocytes were isolated from mice by an in situ collagenase perfusion technique (type VI, Worthington), as previously described (29). Hepatocytes were separated from the non-parenchymal cells by two cycles of differential centrifugation and further purified over a 30% Percoll gradient (Sigma-Aldrich, St. Louis, MO, USA). Cells were allowed to adhere overnight. Before each experiment, cells were washed with PBS and new media placed into the wells. Hepatocytes were exposed to hypoxia as previously described (1). In brief, cells were placed in the hypoxia chamber for 18 h, whereas normoxic cells remained in the incubator. All treatments were performed in duplicate. After the incubation period, the media and cells were collected for analysis.
Of note, the in vitro activity of eritoran has been confirmed by treating whole blood with increasing concentrations of eritoran (0 to 0.2 mol/L) (11). Plasma TNF-α concentrations were found to be reduced by >50% compared with control at an eritoran dose of 6.25 nmol/L and >95% inhibited at eritoran doses >25 nmol/L (11). Given that there was significant inhibition of inflammatory cytokines with low concentrations of eritoran in whole blood, we also trialed a low dose of 8 ng/mL or 6.25 nmol/L eritoran when assessing HMGB1 release and inflammatory cytokine expression in vitro. The dose of 8 ng/mL eritoran was used for all in vitro experiments after performing titration studies, demonstrating similar inhibition to what was seen in whole blood when measuring HMGB1 release. The data for these studies are not shown.
Measurement of Liver Function Tests
Approximately 1.5 mL blood was obtained from each animal via cardiac puncture. The serum was extracted and analyzed for alanine transaminase (ALT) levels using the DRI-CHEM 4000 Chemistry Analyzer System (Heska, Loveland, CO, USA).
Histological Analysis of Necrosis
Liver tissue was immediately placed in a solution of 4% paraformaldehyde after liver I/R. The extent of parenchymal necrosis in the ischemic lobes was evaluated using hematoxylin and eosin (H&E)-stained histological sections at 40× magnification on an Nikon Eclipse E800 microscope (Nikon Instruments Inc., Melville, NY, USA) (30). The necrotic area was quantitatively assessed with ImageJ (NIH, Bethesda, MD, USA; https://doi.org/rsb.info.nih.gov/ij/) software. Results are presented as the mean of percentage of necrotic area (mm2) with respect to the entire area of one capture (mm2).
SYBR Green Real-Time Reverse-Transcription PCR
Total RNA was isolated by using TRIzol (Life Technologies [Thermo Fisher Scientific, Waltham, MA, USA]). In brief, 50–100 mg liver tissue was homogenized in 1 mL TRIzol reagent, and then 0.2 mL chloroform was added to each sample, incubated for 2–3 min at room temperature and then centrifuged at 12,000g for 15 min at 4°C. The RNA was extracted from the aqueous phase, and 0.5 mL 100% isopropanol was added to each sample of RNA, incubated for 10 min and centrifuged at 12,000g for 10 min at 4°C. Finally, the RNA pellet was washed with 1 mL 75% ethanol and centrifuged at 7,500g for 5 min at 4°C. The RNA pellet was air-dried for 5 min, resuspended in 20–60 µL RNA-free water and dissolved at 60°C. Total RNA was measured using the NanoDrop 2000 machine (Thermo Scientific [Thermo Fisher Scientific]), and 1 µg RNA was reverse-transcribed to cDNA by using RNA to cDNA EcoDry Premix (Clontech Laboratories Inc., Mountain View, CA, USA). The resultant cDNA was subjected to quantitative real-time PCR on the Applied Biosystems StepOnePlus Real-Time PCR System (Thermo Fisher Scientific). mRNA for TNF-α, IL-6 and β-actin was quantified in triplicate by using described primers (1).
Sodium Dodecyl Sulfate-Polyacrylamide Gel Electrophoresis (SDS-PAGE) and Western Blotting
Western blot assays were performed by using whole cell lysates from liver tissue or media from cell cultures as previously described (22). In brief, protein was extracted from liver tissue, and the concentration was determined by bicinchoninic acid (BCA) assay. Equal amounts of protein were loaded onto the SDS-PAGE gel, which ran for 1.5–2 h. The protein was then transferred from the gel to the membrane and blocked with 5% bovine serum albumin (BSA) in Tris-buffered saline with Tween (TBST) for 1 h at room temperature. The membrane was then incubated with the primary antibody overnight at 4°C. Membranes were incubated by using the following antibodies: HMGB1 (Abcam, Cambridge, MA, USA) and β-actin (Sigma-Aldrich), phospho-p38, p38, phospho-c-Jun N-terminal kinase (JNK), JNK, extracellular signal-regulated kinase (ERK), phospho-ERK, p65, phospho-p65 (Cell Signaling Technology Inc., Danvers, MA, USA), Myd88 (Abcam), IRAK-1 and phospho-IRAK-1 (Cell Signaling Technology Inc.). Membranes were developed with the Odyssey Detection Systems (LI-COR, Lincoln, NE, USA).
Immunofluorescent Staining
Liver tissue was immediately placed in a solution of 4% paraformaldehyde for 2 h and then transferred to a 30% sucrose solution for 24 h. Liver sections were fixed, stained and imaged with the Fluoview 500 confocal microscope (Olympus, Center Valley, PA, USA) at the Center for Biologic Imaging, as previously described (1,31). Liver tissue or hepatocytes were incubated with HMGB1 primary antibody (1:1,000; Abcam) to assess nuclear release of HMGB1.
Enzyme-Linked Immunosorbent Assay
Murine serum and media from RAW 264.7 cells were analyzed for TNF-α and IL-6 levels using an enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems, Minneapolis, MN, USA). HMGB1 levels were measured in the media from hepatocytes and the in vivo serum samples by using an ELISA kit (IBL International Corp., Toronto, ON, Canada).
Statistical Analysis
Data are presented as means ± standard deviation. Group comparisons were performed by using a Student t test or analysis of variance (ANOVA). Differences were considered significant at p < 0.05.
Results
Pharmacological Inhibition of TLR4 with Eritoran Is Protective in Liver I/R
To determine the impact of TLR4 antagonism on the injury and histological response induced by I/R, C57BL/6 mice were subjected to warm hepatic I/R. Animals were given eritoran (5 mg/kg) or vehicle control 30 min before ischemia. Sixty minutes of warm hepatic ischemia followed by 6 h of reperfusion significantly decreased serum ALT levels in eritoran-treated mice compared with vehicle-treated controls (Figure 1A). In addition, liver histology correlated with the serum ALT estimation of liver damage. Mice that were treated with vehicle control demonstrated severe sinusoidal congestion and hepatocellular necrosis, whereas mice that were treated with eritoran had minimal damage to the liver architecture (Supplementary Figure 1). The extent of necrotic area was significantly decreased in eritoran-treated mice at 6 h of reperfusion (Figure 1B). These results demonstrate that the TLR4 antagonist eritoran is protective in liver I/R and confirms the role of TLR4 in liver damage in warm I/R.
Pharmacological inhibition of TLR4 with eritoran protects against liver I/R injury. (A) Sham or I/R-treated mice were given eritoran (5 mg/kg body weight) or vehicle control intraperitoneally 30 min before ischemia. Data represent the mean ± SEM (n ≥ 6 mice per group). Gray, eritoran; black, control. *P < 0.05, by oneway ANOVA. (B) Quantification of necrotic hepatocytes in H&E-stained liver sections from sham, control and eritorantreated animals 6 h after reperfusion. The graph is representative of liver sections from three or more mice per group. *P < 0.05, by one-way ANOVA.
Eritoran Suppresses TLR4 Signaling Pathways in Liver I/R
Most TLRs use MyD88 to initiate intracellular signaling (3). MyD88 recruitment initiates activation of additional intermediate signaling molecules; these proteins include IRAK-1 and eventually culminates in the activation of MAPK cascades (3). In I/R injury, the cascade of events that result in organ damage is initiated at the onset of ischemia (22,32). To provide evidence that eritoran inhibited TLR4 signaling, we next examined the downstream mediators associated with TLR4 and MAPK signaling pathways. We found that after 1 h of reperfusion, Myd88 and the phosphorylation of IRAK-1 were suppressed in eritoran-treated mice compared with controls (Figure 2A). In addition, the phosphorylation of JNK, p38, ERK and NF-κB (p65 subunit) were less in eritoran-treated mice (Figure 2B). These results demonstrate that the action of eritoran on TLR4 reduces the activation of the inflammatory signaling cascade in liver I/R.
Eritoran suppresses TLR4 signaling pathways and mediates inflammatory signaling in liver I/R. (A) Myd88 and the phosphorylation of IRAK-1 were determined by Western blot and quantitative densitometry analysis of the protein expressions in eritoran-treated mice and control mice that underwent ischemia, and 1 h of reperfusion was determined. Hepatic protein lysates from ischemic lobes were obtained; each lane represents a separate animal. The blots shown are representative of three experiments with similar results. *P < 0.05 versus control, by Student t test. (B) MAPK activation and phosphorylation at serine 536 of the p65 subunit of NF-κB were determined by Western blot and quantitative densitometry analysis of the protein expressions in eritoran-treated mice and control mice that underwent ischemia and 1 h of reperfusion. Hepatic protein lysates from ischemic lobes were obtained; each lane represents a separate animal. The blots shown are representative of three experiments with similar results. *P < 0.05 versus control, by Student t test.
Eritoran Decreases Production of I/R-Induced Inflammatory Mediators
Inflammatory cytokines, such as TNF-α and IL-6, have been shown to play key roles in the pathophysiology of hepatic I/R injury (22,33,34). Using realtime PCR (RT-PCR), we measured mRNA levels for these cytokines in the liver after I/R. Compared with control animals subjected to I/R, eritoran treatment significantly suppressed expression of TNF-α and IL-6 mRNA after 6 h of reperfusion (Figure 3). This result is consistent with our previous finding demonstrating that eritoran diminishes TLR4 and MAPK signaling.
Eritoran decreases I/R-induced inflammatory cytokine gene expression. Serum levels of TNF-α and IL-6 obtained from control and eritoran-treated mice at 6 h after reperfusion were measured by RT-PCR. Results are expressed as a relative increase of mRNA expression compared with sham-treated animals. Data represent the mean ± SEM (n ≥ 3 mice per group). *P < 0.05.
Eritoran Has the Capacity to Attenuate HMGB1-Mediated Liver I/R Injury
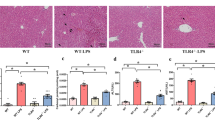
Considerable evidence supports a role for HMGB1 as a DAMP that promotes inflammation and liver damage in liver I/R (22). In addition, evidence suggests that TLR4 acts as a receptor to HMGB1 (23). Knowing that HMGB1 has such an important role in triggering inflammation in liver I/R, we next sought to determine whether eritoran could block the downstream inflammatory signaling cascade associated with the HMGB1-TLR4 interaction. We found that recombinant HMGB1 significantly increased serum ALT levels compared with control. Eritoran blocked the enhancement of liver damage induced by recombinant HMGB1 treatment (Figure 4A). Liver histology confirmed the ALT estimation of liver damage. Mice that were treated with vehicle control demonstrated severe sinusoidal congestion and hepatocellular necrosis, which was even more exaggerated with the addition of recombinant HMGB1 treatment. However, mice that received both eritoran and recombinant HMGB1 had minimal changes in liver architecture and a significant protection from hepatocellular necrosis (Figure 4B). Using ELISA, we found that eritoran also blocked the increase in circulating TNF-α and IL-6 resulting from HMGB1 treatment during I/R (Figure 4C). These results confirm that HMGB1 enhances liver damage and inflammation in I/R via TLR4.
Treatment with eritoran attenuates HMGB1-mediated liver I/R injury. (A) Sham, control, eritoran-treated, control with recombinant HMGB1, and eritoran with recombinant HMGB1-treated mice underwent 6 h of reperfusion, and serum ALT levels were analyzed. Eritoran (5 mg/kg body weight) administered intraperitoneally 30 min before ischemia and recombinant HMGB1 (25 µL/mouse) administered intraperitoneally immediately before reperfusion. Data represent the mean ± SEM (n ≥ 3 mice per group). *P < 0.05, by one-way ANOVA. (B) Quantification of necrotic hepatocytes in H&E-stained liver tissue. The graph is representative of liver sections from three or more mice per group. *P < 0.05, by one-way ANOVA. (C) Hepatic TNF-α and IL-6 ELISA. Data are expressed as mean ± SEM of three independent experiments. *P < 0.05, by one-way ANOVA.
Eritoran Suppresses HMGB1 Release During Liver I/R in a TLR4-Dependent Manner
TLR4 not only functions as a receptor for HMGB1, but also mediates its nucleocytoplasmic shuttling and subsequent release in ischemic hepatocytes (1,35,36). To determine whether eritoran diminishes I/R-induced HMGB1 release, nuclear and cytoplasmic fractions were separated from whole cell lysate and HMGB1 protein expression was determined. We found that eritoran prevented HMGB1 loss from the nucleus induced by I/R (Figure 5A). This result was confirmed, with HMGB1 ELISA demonstrating significantly lower HMGB1 serum levels in eritoran-treated mice during liver I/R (Figure 5B). Immunofluorescent images reveal increased nuclear staining and minimal cytoplasmic HMGB1 in hepatocytes of eritoran-treated mice compared with controls undergoing liver I/R, where there was loss of HMGB1 from the nucleus (Figure 5C). Furthermore, we have redemonstrated that in TLR4 wild-type mice undergoing liver I/R, HMGB1 levels in serum collected 6 h after reperfusion is significantly decreased in the mice treated with eritoran. However, in TLR4 knockout mice, eritoran did not cause a significant decrease in released HMGB1 compared with controls (Figure 5D). This shows that eritoran decreases HMGB1 release through a TLR4-dependent mechanism. This result is in concordance with our previous work that HMGB1 release from hepatocytes during ischemia is TLR4 dependent (36). Thus, by inhibiting TLR4, eritoran blocks the release of HMGB1. In addition, as a result of restricted hepatic inflammation with TLR4 blockade, HMGB1 release is further decreased. Overall, these results highlight that eritoran attenuates HMGB1 release in a TLR4-dependent manner during liver I/R, a novel role for this TLR4 antagonist.
Eritoran treatment suppresses HMGB1 release in vivo. (A) Nuclear and cytoplasmic HMGB1 levels were determined by Western blot and quantitative densitometry analysis of the protein expressions in eritoran-treated mice and control mice that underwent ischemia and 6 h of reperfusion determined. Hepatic protein lysates from ischemic lobes were obtained; each lane represents a separate animal. The blots shown are representative of two experiments with similar results. (B) Serum HMGB1 ELISA after 6 h of reperfusion. Data are representative of two experiments with similar results. Gray, eritoran; white, control. *P < 0.05 when compared against control by one-way ANOVA. (C) Immunofluorescent stain of HMGB1 from sections of sham liver and liver 6 h after I/R in placebo control, and eritoran-treated mice (magnification 40×). Images are representative of liver sections from two mice per group. Red, HMGB1; blue, nuclei; green, F-actin. (D) TLR4 wild-type and knockout mice were given eritoran (5 mg/kg body weight) or vehicle control intraperitoneally 30 min before ischemia. HMGB1 levels in serum were collected 6 h after reperfusion and quantified using ELISA. Data represent the mean ± SEM (n ≥ 6 mice per group). Gray, eritoran; white, control. *P < 0.05, by one-way ANOVA.
Eritoran Decreases HMGB1 Release by Hepatocytes and Interferes with HMGB1 Activation of RAW 264.7 Cells In Vitro
Hepatocytes contribute significantly to the evolution of liver I/R injury by generating reactive oxygen species, releasing proinflammatory cytokines and chemokines and thus enhancing the inflammation (37). Hepatocytes are the major source of HMGB1 (38), and our lab has previously shown that hypoxia induces HMGB1 release in a time-dependent manner (36). Thus, we further investigated the effect of eritoran on hepatocyte HMGB1 release in the setting of hypoxia in vitro. We found that eritoran (8 ng/mL) suppressed the release of HMGB1 into the media of hypoxic hepatocytes (18 h) (Figure 6A). Immunofluo-rescent images corroborate these findings. Images reveal increased nuclear staining and minimal cytoplasmic HMGB1 in hypoxic hepatocytes cultured with eritoran (Figure 6B). These findings confirm the in vivo results and suggest that eritoran has the capacity to decrease hypoxia-induced HMGB1 release.
Eritoran decreases HMGB1 release by hepatocytes and blocks the inflammatory response of RAW 264.7 cells by HMGB1 in vitro. (A) Eritoran-treated (8 ng/mL) or control hepatocytes were cultured under normoxia or 18 h hypoxia. The media were then analyzed using ELISA for HMGB1. White, control; gray, eritoran. *P < 0.05 when compared against control by one-way ANOVA. (B) Immunofluorescent staining depicting the translocation of HMGB1 in cultured hepatocytes from eritoran-treated (8 ng/mL) or control hepatocytes that were stimulated with either 18 h hypoxia or normoxia was visualized and observed under confocal microscope (magnification ×120). Green, actin; blue, nuclei; red, HMGB1. (C) Hepatocytes were stimulated with LPS (1 µg/mL), recombinant HMGB1 (1 µg/mL), or eritoran (8 ng/mL) in the above combinations for a total of 18 h of stimulation. The media were then analyzed using ELISA for TNF-α and IL-6. Data are representative of two experiments with similar results. White, PBS; gray, eritoran. *P < 0.05 versus control, by one-way ANOVA.
It is well known that LPS stimulation of the RAW 264.7 macrophage cell line leads to the production of inflammatory cytokines. It has also been shown that eritoran can block LPS activation of innate immune cells (5,10) and induction of inflammatory cytokines by LPS stimulation in ex vivo blood samples from septic patients (11). HMGB1, like LPS, can activate macrophages and cause the release of TNF-α and IL-6 in vitro (24,39,40–43), but it is unknown whether eritoran can block activation of immune cells by HMGB1. We sought to investigate this by culturing RAW 264.7 cells with recombinant HMGB1 (1 µg/mL), LPS (1 µg/mL), eritoran (8 ng/mL) with LPS and eritoran with HMGB1 for 18 h. We found that eritoran blocked TNF-α and IL-6 production induced by recombinant HMGB1 (Figure 6C). Thus, eritoran interferes with HMGB1 recognition in macrophages.
Discussion
The pathogenesis of hepatic I/R results from a local inflammatory response caused by cessation of blood flow and subsequent reperfusion injury. The excessive generation of inflammatory mediators can lead to hepatic nonfunction. Therefore, suppression of the excessive release of such mediators provides one avenue by which potential therapies may be beneficial. This study was undertaken to determine whether a well characterized inhibitor of the TLR4/MD2 complex protected mice during liver I/R. We postulated that blocking the TLR4 receptor would reduce liver damage during I/R because of the known role of TLR4 in driving the inflammatory response (4–7). Our results showed that eritoran was protective and revealed a valuable role for TLR4 antagonism in the pathophysiology of liver I/R injury. In this study, we have illustrated that blocking the innate immune receptor TLR4 with eritoran leads to two major intracellular changes responsible for decreasing hepatocellular injury, including (a) decreased inflammatory mediators associated with the TLR4 signal transduction pathway and (b) inhibition of HMGB1 release from hepatocytes leading to decreased production of inflammatory cytokines.
The generation of inflammatory cytokines after I/R injury is one of the early events that leads to the propagation of the injury response (2). TNF-α is the central component of the proinflammatory cytokine cascade (2). TNF-α recruits neutrophils to the ischemic liver and further increases the inflammatory response via the release of cell-specific cytokines, resulting in a vicious cycle of inflammation and organ damage. Previous work using animal models of kidney and cardiac I/R have consistently shown that eritoran is capable of attenuating inflammation, as evidenced by a decrease in TNF-α and IL-6 (18,19). Our results are consistent with previously published work showing decreased inflammation with eritoran treatment. This finding not only provides evidence that eritoran is antagonizing TLR4, but also shows that eritoran has therapeutic potential in liver I/R.
We found that not only does eritoran decrease the inflammatory response associated with liver I/R, but it also reduces the inflammation associated with HMGB1 signaling. HMGB1 is upregulated by hypoxia during warm I/R (6,22). It is well established that HMGB1 plays a central role in sterile inflammation (44–46) and that it functions as a proinflammatory DAMP via TLR4 (22). Administration of recombinant HMGB1 worsens hepatic injury only in TLR4-competent mice, while neutralizing antibody to HMGB1 decreases liver damage and suppresses the activation of inflammatory cascades, mimicking the TLR4-deficient state (6,22). We show that eritoran decreases DAMP signaling in liver I/R as evidenced by decreased serum ALT levels, decreased necrosis and reduced expression of inflammatory cytokines. It is also known that HMGB1 modulates inflammatory responses in LPS-activated macrophages (24). We show that eritoran reduces inflammatory cytokine production in HMGB1-stimulated macrophages. Together, our results demonstrate that eritoran attenuates HMGB1’s activation of inflammatory signaling in vitro and in vivo and therefore counteracts not only LPS recognition by TLR4 but also the capacity of the TLR4 receptor complex to react to HMGB1.
In addition to blocking the cytokine-like properties of HMGB1, we chose to further investigate the potential role of eritoran on HMGB1 release from the liver, since we have previously published that HMGB1 release is TLR4 dependent (35,36). We show that eritoran attenuates the release of HMGB1 from hepatocytes both in vivo and in vitro. More specifically, eritoran treatment during liver I/R was associated with decreased nuclear-to-cytoplasmic translocation of HMGB1, which was confirmed with an HMGB1 ELISA demonstrating reduced serum HMGB1. Our studies show that the mechanism by which eritoran suppresses HMGB1 release is TLR4 dependent, which is in concordance with our previous work that HMGB1 release from hepatocytes during ischemia is TLR4 dependent (35,36). Of note, eritoran can also block HMGB1 release in the absence of I/R. In culture, we show that eritoran decreases the release of HMGB1 in the setting of hypoxia from hepatocytes, the main source of HMGB1 (38). Our findings corroborate our previous work illustrating the dependence on TLR4 for HMGB1 release and are unique from other studies where the more global effect of TLR4 antagonism with eritoran has been demonstrated.
We believe that the protective effect of eritoran in liver I/R is related to HMGB1 and eritoran binding to the MD2 portion of the TLR4 receptor. The interaction of MD2 with eritoran has been extensively studied and has been described above (8). Yang et al. (26) showed that HMGB1 binds to MD2 with high affinity and is unable to stimulate macrophages in which MD2 was knocked down. It is known that efficient recognition of HMGB1 by the TLR4/MD2 complex requires the appropriate redox status of the three cysteine groups on HMGB1 (47). There are two main redox states of HMGB1: the disulfide HMGB1 and the all-thiol HMGB1 (48,49). The three conserved cysteines of HMGB1 are in positions 23 and 45 within the A box and position 106 in the B box (48,49). The cysteines in the A box are ideally placed to form a disulfide bond, while C106 in the B box remains unpaired (48,49). Because of the strongly reducing redox potential inside the cell, intracellular HMGB1 is largely in the reduced state (48,49). Therefore, HMGB1 release by passive mechanisms is typically in the all-thiol configuration. However, mild oxidizing conditions convert all-thiol HMGB1 to C23-C45 disulfide (49). The disulfide-containing form of HMGB1 is the state that was shown to bind the MD2 domain within the TLR4 receptor complex and induce an inflammatory response as long as C106 is in the thiol configuration (49). Therefore, eritoran appears to compete with disulfide HMGB1 for binding to MD2/TLR4 and thus ameliorates the driving force of the immunopathology of liver I/R. The exact binding domain within MD2 for HMGB1 is yet to be resolved, and further studies are needed to examine whether eritoran and HMGB1 bind the same or adjacent domains within MD2. In addition, by inhibiting the release of all-thiol HMGB1, eritoran would also indirectly ameliorate function of HMGB1 as a chemoattractant. Therefore, eritoran can block the two main functions of HMGB1 as a chemoattractant and as a proinflammatory cytokine; as a result, it confers protection in liver I/R.
Conclusion
In summary, the present study demonstrates that pharmacological inhibition of TLR4 with eritoran is protective in a mouse model of liver I/R. By antagonizing the HMGB1-TLR4 interaction, eritoran is capable of interfering with HMGB1 release from hepatocytes and attenuating the cytokine-like actions of HMGB1 on innate immune cells. Therefore, targeting the TLR4 receptor directly with agents such as eritoran provides an avenue to reduce I/R-related hepatic injury.
Disclosure
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
References
Tsung A, et al. (2005) Hepatic ischemia/reperfusion injury involves functional TLR4 signaling in non-parenchymal cells. J. Immunol. 175:7661–8.
Abu-Amara M, et al. (2010) Liver ischemia/reperfusion injury: processes in inflammatory networks: a review. Liver Transpl. 16:1016–32.
Evankovich J, Billiar T, Tsung A. (2010) Toll-like receptors in hepatic ischemia/reperfusion and transplantation. Gastroenterol. Res. Pract. 2010:537263.
Wu HS, et al. (2004) Toll-like receptor 4 involvement in hepatic ischemia/reperfusion injury in mice. Hepatobiliary Pancreat. Dis. Int. 3:250–3.
Zhai Y, et al. (2004) Cutting edge: TLR4 activation mediates liver ischemia/reperfusion inflammatory response via IFN regulatory factor 3-dependent MyD88-independent pathway. J. Immunol. 173:7115–9.
Gill R, Tsung A, Billiar T. (2010) Linking oxidative stress to inflammation: Toll-like receptors. Free Radic. Biol. Med. 48:1121–32.
Shen XD, et al. (2005) Toll-like receptor and heme oxygenase-1 signaling in hepatic ischemia/reperfusion injury. Am. J. Transplant. 5:1793–800.
Kim HM, et al. (2007) Crystal structure of the TLR4-MD-2 complex with bound endotoxin antagonist Eritoran. Cell 130:906–17.
Barochia A, Solomon S, Cui X, Natanson C, Eichacker PQ. (2011) Eritoran tetrasodium (E5564) treatment for sepsis: review of preclinical and clinical studies. Expert Opin. Drug Metab. Toxicol. 7:479–94.
Mullarkey M, et al. (2003) Inhibition of endotoxin response by e5564, a novel Toll-like receptor 4-di-rected endotoxin antagonist. J. Pharmacol. Exp. Ther. 304:1093–102.
Rossignol DP, et al. (2004) Safety, pharmacokinetics, pharmacodynamics, and plasma lipoprotein distribution of eritoran (E5564) during continuous intravenous infusion into healthy volunteers. Antimicrob. Agents Chemother. 48:3233–40.
Czeslick E, Struppert A, Simm A, Sablotzki A. (2006) E5564 (Eritoran) inhibits lipopolysaccharide-induced cytokine production in human blood monocytes. Inflamm. Res. 55:511–5.
Ehrentraut S, et al. (2011) In vivo Toll-like receptor 4 antagonism restores cardiac function during endotoxemia. Shock. 36:613–20.
Figueiredo MD, Moore JN, Vandenplas ML, Sun WC, Murray TF. (2008) Effects of the second-generation synthetic lipid A analogue E5564 on responses to endotoxin in [corrected] equine whole blood and monocytes. Am. J. Vet. Res. 69:796–803.
Rossignol DP, Lynn M. (2002) Antagonism of in vivo and ex vivo response to endotoxin by E5564, a synthetic lipid A analogue. J. Endotoxin. Res. 8:483–8.
Opal SM, et al. (2013) Effect of eritoran, an antagonist of MD2-TLR4, on mortality in patients with severe sepsis: the ACCESS randomized trial. JAMA. 309:1154–62.
Korff S, et al. (2013) Eritoran attenuates tissue damage and inflammation in hemorrhagic shock/trauma. J. Surg. Res. 184:e17–25.
Liu M, et al. (2010) Protective effects of Toll-like receptor 4 inhibitor eritoran on renal ischemia-reperfusion injury. Transplant Proc. 42:1539–44.
Shimamoto A, et al. (2006) Inhibition of Toll-like receptor 4 with eritoran attenuates myocardial ischemia-reperfusion injury. Circulation. 114 (1 Suppl): 1270–4.
Shirey KA, et al. (2013) The TLR4 antagonist Eritoran protects mice from lethal influenza infection. Nature. 497:498–502.
Sun Y, Pearlman E. (2009) Inhibition of corneal inflammation by the TLR4 antagonist Eritoran tetrasodium (E5564). Invest. Ophthalmol. Vis. Sci. 50:1247–54.
Tsung A, et al. (2005) The nuclear factor HMGB1 mediates hepatic injury after murine liver ischemia-reperfusion. J. Exp. Med. 201:1135–43.
Park JS, et al. (2004) Involvement of toll-like receptors 2 and 4 in cellular activation by high mobility group box 1 protein. J. Biol. Chem. 279:7370–7.
El GM. (2007) HMGB1 modulates inflammatory responses in LPS-activated macrophages. Inflamm. Res. 56:162–7.
Yu M, et al. (2006) HMGB1 signals through tolllike receptor (TLR) 4 and TLR2. Shock. 26:174–9.
Yang H, Antoine DJ, Andersson U, Tracey KJ. (2013) The many faces of HMGB1: molecular structure-functional activity in inflammation, apoptosis, and chemotaxis. J. Leukoc. Biol. 93:865–73.
Committee for the Update of the Guide for the Care and Use of Laboratory Animals, Institute for Laboratory Animal Research, Division on Earth and Life Studies, National Research Council of the National Academies. (2011) Guide for the Care and Use of Laboratory Animals. 8th edition. Washington (DC): National Academies Press.
Tsung A, et al. (2006) The transcription factor interferon regulatory factor-1 mediates liver damage during ischemia-reperfusion injury. Am. J. Physiol. Gastrointest. Liver Physiol. 290:G1261–8.
West MA, Billiar TR, Curran RD, Hyland BJ, Simmons RL. (1989) Evidence that rat Kupffer cells stimulate and inhibit hepatocyte protein synthesis in vitro by different mechanisms. Gastroenterology. 96:1572–82.
Huang H, et al. (2011) Hepatic arterial perfusion is essential for the spontaneous recovery from focal hepatic venous outflow obstruction in rats. Am. J. Transplant. 11:2342–52.
Sun Q, et al. (2013) Caspase 1 activation is protective against hepatocyte cell death by up-regulating beclin 1 protein and mitochondrial autophagy in the setting of redox stress. J. Biol. Chem. 288:15947–58.
McCloskey CA, Kameneva MV, Uryash A, Gallo DJ, Billiar TR. (2004) Tissue hypoxia activates JNK in the liver during hemorrhagic shock. Shock. 22:380–6.
Colletti LM, et al. (1996) The role of cytokine networks in the local liver injury following hepatic ischemia/reperfusion in the rat. Hepatology. 23:506–14.
Wanner GA, et al. (1999) Differential effect of anti-TNF-alpha antibody on proinflammatory cytokine release by Kupffer cells following liver ischemia and reperfusion. Shock. 11:391–5.
Nace GW, et al. (2013) Cellular-specific role of toll-like receptor 4 in hepatic ischemia-reperfusion injury in mice. Hepatology. 58:374–87.
Tsung A, et al. (2007) HMGB1 release induced by liver ischemia involves Toll-like receptor 4 dependent reactive oxygen species production and calcium-mediated signaling. J. Exp. Med. 204:2913–23.
Bhogal RH, Sutaria R, Afford SC. (2011) Hepatic liver ischemia/reperfusion injury: processes in inflammatory networks: a review. Liver Transpl. 17:95.
Evankovich J, et al. (2010) High mobility group box 1 release from hepatocytes during ischemia and reperfusion injury is mediated by decreased histone deacetylase activity. J. Biol. Chem. 285:39888–97.
Gero D, et al. (2013) Identification of pharmacological modulators of HMGB1-induced inflammatory response by cell-based screening. PLoS One. 8:e65994.
Li J, et al. (2003) Structural basis for the proin-flammatory cytokine activity of high mobility group box 1. Mol. Med. 9:37–45.
Wang H, Yang H, Czura CJ, Sama AE, Tracey KJ. (2001) HMGB1 as a late mediator of lethal systemic inflammation. Am. J. Respir. Crit. Care Med. 164:1768–73.
Kim S, et al. (2013) Signaling of high mobility group box 1 (HMGB1) through toll-like receptor 4 in macrophages requires CD14. Mol. Med. 19:88–98.
Li J, et al. (2004) Recombinant HMGB1 with cytokine-stimulating activity. J. Immunol. Methods. 289:211–23.
Andersson U, Tracey KJ. (2011) HMGB1 is a therapeutic target for sterile inflammation and infection. Annu. Rev. Immunol. 29:139–62.
Harris HE, Andersson U, Pisetsky DS. (2012) HMGB1: a multifunctional alarmin driving autoimmune and inflammatory disease. Nat. Rev. Rheumatol. 8:195–202.
Klune JR, Dhupar R, Cardinal J, Billiar TR, Tsung A. (2008) HMGB1: endogenous danger signaling. Mol. Med. 14:476–84.
Park JS, et al. (2006) High mobility group box 1 protein interacts with multiple Toll-like receptors. Am. J. Physiol. Cell Physiol. 290:C917–24.
Hoppe G, Talcott KE, Bhattacharya SK, Crabb JW, Sears JE. (2006) Molecular basis for the redox control of nuclear transport of the structural chromatin protein Hmgb1. Exp. Cell Res. 312:3526–38.
Venereau E, et al. (2012) Mutually exclusive redox forms of HMGB1 promote cell recruitment or proinflammatory cytokine release. J. Exp. Med. 209:1519–28.
Acknowledgments
This work was supported by a Howard Hughes Medical Institute Physician-Scientist Award (to A Tsung), R01-GM95566 (to A Tsung) and R01-GM50441 (to T Billiar). The authors would like to thank Eisai for the generous gift of eritroran and Xinghua Liao for technical assistance in preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, and provide a link to the Creative Commons license. You do not have permission under this license to share adapted material derived from this article or parts of it.
The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this license, visit (https://doi.org/creativecommons.org/licenses/by-nc-nd/4.0/)
About this article
Cite this article
McDonald, KA., Huang, H., Tohme, S. et al. Toll-like Receptor 4 (TLR4) Antagonist Eritoran Tetrasodium Attenuates Liver Ischemia and Reperfusion Injury through Inhibition of High-Mobility Group Box Protein B1 (HMGB1) Signaling. Mol Med 20, 639–648 (2014). https://doi.org/10.2119/molmed.2014.00076
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2119/molmed.2014.00076