Abstract
Objectives
To determine volumes and rates of multimorbidity in Ontario by age group, sex, material deprivation, and geography.
Methods
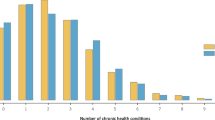
A cross-sectional population-based study was completed using linked provincial health administrative databases. Ontario residents were classified as having multimorbidity (3+ chronic conditions) or not, based on the presence of 17 chronic conditions. The volumes (number of residents) of multimorbidity were determined by age categories in addition to crude and age-sex standardized rates.
Results
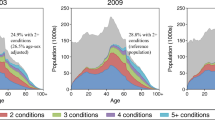
Among the 2013 Ontario population, 15.2% had multimorbidity. Multimorbidity rates increased across successively older age groups with lowest rates observed in youngest (0–17 years, 0.2%) and highest rates in the oldest (80+ years, 73.5%). The rate of multimorbidity increased gradually from ages 0 to 44 years, with a substantial and graded increase in the rates as the population aged. The top five chronic conditions, of the 17 examined, among those with multimorbidity were mood disorders, hypertensive disorders, asthma, arthritis, and diabetes.
Conclusion
Much of the common rhetoric around multimorbidity concerns the aging ‘grey tsunami’. This study demonstrated that the volume of multimorbidity is derived from adults beginning as young as age 35 years old. A focus only on the old underestimates the absolute burden of multimorbidity on the health care system. It can mask the association of material deprivation and geography with multimorbidity which can turn our attention away from two critical issues: (1) potential inequality in health and health care in Ontario and (2) preventing younger and middle-aged people from moving into the multimorbidity category.
Résumé
Objectif
Déterminer les volumes et les taux de multimorbidité en Ontario selon le groupe d’âge, le sexe, la défavorisation matérielle et la géographie.
Méthode
Une étude populationnelle transversale a été exécutée en maillant des bases de données administratives de santé provinciales. Les résidents de l’Ontario ont été catégorisés comme ayant ou non des multimorbidités (3 états chroniques ou plus) en fonction de la présence de 17 états chroniques. Les volumes (nombre de résidents) de multimorbidité ont été déterminés par catégorie d’âge en plus des taux bruts et des taux standardisés pour l’âge et le sexe.
Résultats
Dans la population ontarienne de 2013, 15,2% des gens étaient atteints de multimorbidités. Les taux de multimorbidité augmentaient avec chaque groupe d’âge, les taux les plus faibles étant observés chez les plus jeunes (0-17 ans : 0,2%), et les taux les plus élevés, chez les plus âgés (80 ans et plus : 73,5%). Le taux de multimorbidité augmentait progressivement entre 0 et 44 ans, avec une hausse graduelle considérable dans les taux avec l’âge de la population. Sur les 17 états chroniques compris dans l’étude, les 5 états les plus courants chez les personnes atteintes de multimorbidités étaient les troubles de l’humeur, les troubles hypertensifs, l’asthme, l’arthrite et le diabète.
Conclusion
Le discours sur la multimorbidité s’articule principalement autour du « tsunami gris » du vieillissement. Notre étude démontre que le volume de multimorbidité comprend des adultes aussi jeunes que 35 ans. La restriction des études aux seules personnes âgées sous-estime le fardeau absolu de la multimorbidité sur le système de soins de santé. Elle peut masquer l’association entre la défavorisation matérielle ou la géographie et les multimorbidités, ce qui peut détourner notre attention de deux questions névralgiques : 1) les inégalités possibles sur le plan de la santé et des soins de santé en Ontario et 2) comment empêcher les jeunes et les personnes d’âge moyen de passer dans la catégorie des personnes atteintes de multimorbidités.



Similar content being viewed by others
References
Bains N. (2009). Standardization of rates. Report from the Association of Public Health Epidemiologists in Ontario (APHEO) through the Core Indicators for Public Health in Ontario Project.
Barnett, K., Mercer, S. W., Norbury, M., Watt, G., Wyke, S., & Guthrie, B. (2012). Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet, 380, 37–43. https://doi.org/10.1016/S0140-6736(12)60240-2.
Benchimol, E. I., Smeeth, L., Guttmann, A., Harron, K., Moher, D., Petersen, I., et al. (2015). The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med, 12(10), e1001885. https://doi.org/10.1371/journal.pmed.1001885.
Boyd, C. M., & Fortin, M. (2010). Future of multimorbidity research: how should understanding of multimorbidity inform health system design? Public Health Review, 32, 451–474.
Brady, T. J., Anderson, L. A., & Kobau, R. (2015). Chronic disease self-management support: public health perspectives. Front Public Health, 2(Article 234), 1–5.
Canadian Foundation for Healthcare Improvement. (2011). Myth: the aging populations is to blame for uncontrollable healthcare costs. Mythbusters: using evidence to debunk common misconceptions in Canadian Healthcare. February 2011. Retrieved June 23, 2017. http://www.cfhi-fcass.ca/sf-docs/default-source/mythbusters/Myth_AgingPopulation_EN_FINAL.pdf?sfvrsn=0
CBC News. (2012). Baby boomers’ health demands will pose challenges. May 29, 2012. Retrieved Jun 23, 2017. http://www.cbc.ca/news/health/baby-boomers-health-demands-will-pose-challenges-1.1151890.
CBC News (2014). June 11, 2014. Retrieved Jun 23, 2017. https://www.theglobeandmail.com/opinion/our-hospitals-are-not-ready-forthegreytsunami/article19113784/.
Durbin, A., Moineddin, R., Lin, E., Steele, L. S., & Glazer, R. H. (2015). Examining the relationship between neighbourhood deprivation and mental health service use of immigrants in Ontario, Canada: a cross-sectional study. BMJ Open, 5, e006690. https://doi.org/10.1136/bmjopen-2014-006690.
Fortin, M., Hudon, C., Haggerty, J., Akker, M., & Almirall, J. (2010). Prevalence estimates of multimorbidity: a comparative study of two sources. BMC Health Services Research, 10(1), 111.
Fortin, M., et al. (2012). A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Annals of Family Medicine, 10, 142–151.
Fortin, M., Almirall, J., & Nicholson, K. (2017). Development of a research tool to document self-reported chronic conditions in primary care. Journal of Comorbidity, 7(1), 117–123.
Fung, K. Y., Luginaah, I. N., & Gorey, K. M. (2007). Impact of air pollution on hospital admissions in southwestern Ontario, Canada: generating hypotheses in sentinel high-exposure places. Environ Health, 6, 18. https://doi.org/10.1186/1476-069X-6-18.
Hall RE, Khan F, Levi J, Ma H, Fang J, Martin C, et al. (2017). Ontario and LHIN 2015/16 stroke report cards and progress reports: Setting the bar higher. Toronto, ON: Institute for Clinical Evaluative Sciences
Holzer BM, Siebenhuener K, Bopp M, Minder CE. (2014). Overcoming cut-off restrictions in multimorbidity prevalence estimates. BMC Public Health, 14: 780. http://www.biomedcentral.com/1471-2458/14/780.
Kiran, T., Kopp, A., Moineddin, R., & Glazier, R. H. (2015). Longitudinal evaluation of physician payment reform and team-based care for chronic disease management and prevention. CMAJ, 187(17), E494–E502.
Kiran, T., Kopp, A., & Glazier, R. H. (2016). Those left behind from voluntary medical home reforms in Ontario, Canada. Annals of Family Medicine, 14(6), 517–525.
Koné Pefoyo, A. J., Bronskill, S. E., Gruneir, A., Calzavara, A., Thavorn, K., Petrosyan, Y., et al. (2015). The increasing burden and complexity of multimorbidity. BMC Public Health, 15, 415. https://doi.org/10.1186/s12889-015-1733-2.
Matheson, F. I., Dunn, J. R., Smith, K. L. W., Moineddin, R., & Glazier, R. H. (2012). Development of the Canadian Marginalization Index: a new tool for the study of inequality. Canadian Journal of Public Health, 103(Suppl. 2), S12–S16.
Ontario Local Health Integration Network. (2014). Ontario’s LHINs. © Queen’s Printer for Ontario. Retrieved June 23, 2017. http://www.lhins.on.ca/
Ontario Ministry of Health and Long Term Care. (2012). Legislation: Local Health System Integration Act, 2006. © Queen’s Printer for Ontario. Retrieved June 23, 2017. http://www.health.gov.on.ca/en/common/legislation/lhins/default.aspx
Ontario Ministry of Health and Long-Term Care. (2015). Putting patients first: action plan for health care. http://www.health.gov.on.ca/en/ms/ecfa/healthy_change/. Retrieved November 16, 2015.
Ontario Ministry of Health and Long Term Care. (2017). Data Catalogue: Legislation: Local Health Integration Network (LHIN) Offices. © Queen’s Printer for Ontario Added January 17, 2017. Retrieved June 23, 2017. https://www.ontario.ca/data/local-health-integration-network-office-lhin-locations
Statistics Canada. (2013). Postal Code OM Conversion File (PCCF). Statistics Canada Catalogue no. 92-154-X.
Statistics Canada. (2015). The Daily: Canada’s population estimates: age and sex, July 1, 2015. Updated September 29, 2015. Retrieved July 7, 2017. http://www.statcan.gc.ca/daily-quotidien/150929/dq150929b-eng.htm
Statistics Canada. (2012). The Canadian population in 2011: age and sex. Catalogue no. 98-311-X2011001. Statistics Canada.
The Globe and Mail (2015) Canada’s health-care system braces for hike in costs with influx of seniors. November 8, 2015. Retrieved June 23, 2017. https://www.theglobeandmail.com/globe-investor/retirement/canadas-health-care-system-braces-for-hike-in-costs-with-influx-of-seniors/article27169986/
The Star (2015). Get moving on prepaing for ‘grey tsunami’: Editorial. February 2, 2015. Retrieved June 23, 2017. https://www.thestar.com/opinion/editorials/2015/02/02/get-moving-on-preparing-for-greytsunami-editorial.html.
van den Akker, M., Buntinx, F., Roos, S., & Knottnerus, J. A. (2001). Problems in determining occurrence rates of multimorbidity. Journal of Clinical Epidemiology, 54(7), 675–679.
Violan, C., Foguet-Boreu, Q., Flores-Meteo, G., Salisbury, C., Blom, J., Freitag, M., et al. (2014). Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One, 9(7), e102149. https://doi.org/10.1371/journal.pone.0102149.
Wilkins R. (2004). Neighbourhood income quintiles derived from Canadian postal codes are apt to be misclassified in rural but not urban areas. working paper. Statistics Canada.
Funding
This study was supported by the ICES Western site through participation in the ICES Western Faculty Scholar’s Program. Support for Dr. Bridget Ryan’s participation in the ICES Western Faculty Scholars Program came from the Department of Family Medicine, Schulich School of Medicine and Dentistry, Western University. Dr. Ryan was also funded by the Canadian Institutes of Health Research Community-based Primary Health Care Innovation Team, Patient-centred Innovations for Persons with Multimorbidity.
ICES is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Core funding for ICES Western is provided by the Academic Medical Organization of Southwestern Ontario, the Schulich School of Medicine & Dentistry, Western University and the Lawson Health Research Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the institutional review board at Sunnybrook Health Sciences Centre, Toronto, Canada.
Conflict of interest
The authors declare that they have no conflicts of interest.
Disclaimer
This project was conducted at the Institute for Clinical Evaluative Sciences (ICES) Western Site. These datasets were linked using unique encoded identifiers and analyzed at the Institute for Clinical Evaluative Sciences (ICES). The data were analyzed by Britney Allen, MSc (Biostatistician at ICES Western). Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors, and not necessarily those of CIHI or the other funding sources. No endorsement by CIHI or the other funding sources is intended or should be inferred.
Rights and permissions
About this article
Cite this article
Ryan, B.L., Bray Jenkyn, K., Shariff, S.Z. et al. Beyond the grey tsunami: a cross-sectional population-based study of multimorbidity in Ontario. Can J Public Health 109, 845–854 (2018). https://doi.org/10.17269/s41997-018-0103-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/s41997-018-0103-0