Abstract
OBJECTIVES: Following implementation of a publicly funded rotavirus immunization program in Quebec (Canada) in 2011, its impact on gastroenteritis hospitalization rates, a proxy for severe gastroenteritis, was assessed.
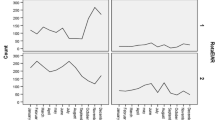
METHODS: Using a tertiary hospital database and a regional vaccination registry, temporal trends in rates of hospitalization for acute gastroenteritis (AGE) and rotavirus gastroenteritis before the age of five years and rotavirus vaccine coverage were examined from June 2004 through May 2014 in a large retrospective birth cohort in the Eastern Townships region. The mean annual AGE hospitalization rate in post-program years (2011/2012–2013/2014) was compared with that in pre-program years (2004/2005–2010/2011) overall and according to the characteristics of the children, families and residential neighbourhoods at birth.
RESULTS: The AGE hospitalization rate significantly decreased from 81/10,000 in the pre-program period to 46/10,000 in the post-program period (relative reduction = 43%). Following implementation of the program, vaccine coverage rapidly increased and reached 81 %. All socio-economic categories showed a reduced hospitalization rate in the post-program period, but the lowest relative reductions were observed in children living in neighbourhoods with higher rates of unemployment, low-income families and single mothers. However, these disadvantaged subgroups did not have lower vaccine coverage.
CONCLUSIONS: Three years following its introduction in a universal vaccination program, rotavirus vaccine significantly reduced severe gastroenteritis in young children. Despite similar vaccine coverage among all children, disadvantaged socio-economic groups appeared to have a less pronounced AGE reduction, suggesting that factors other than vaccination could partially influence the reduction of gastroenteritis morbidity in young children.
Résumé
OBJECTIFS: Suite à l’implantation d’un programme de vaccination contre le rotavirus financé publiquement au Québec en 2011, son impact sur les taux d’hospitalisation pour gastro-entérite, un proxy pour les gastroentérites sévères, a été évalué.
MÉTHODES: Grâce à l’utilisation d’une base de données hospitalières et d’un registre de vaccination régional, les tendances temporelles des taux d’hospitalisation pour gastro-entérite aiguë (GEA) et gastro-entérite à rotavirus (GERV) survenues avant l’âge de cinq ans ainsi que la couverture vaccinale ont été examinées de juin 2004 à mai 2014 parmi une large cohorte rétrospective d’enfants nés dans la région de l’Estrie. Le taux annuel moyen d’hospitalisation pour GEA des années post-programme (2011/2012–2013/2014) a été comparé à celui des années pré-programme (2004/2005–2010/2011 ), globalement et selon plusieurs caractéristiques de l’enfant, de sa famille et de son quartier résidentiel à la naissance.
RÉSULTATS: Le taux d’hospitalisation pour GEA a diminué de 81 /10 000 dans la période pré-programme à 46/10 000 dans la période post-programme (réduction relative = 43 %). Suite à l’implantation du programme, la couverture vaccinale a rapidement augmenté et a atteint 81 %. Toutes les catégories socioéconomiques ont démontré un taux d’hospitalisation réduit dans la période postprogramme, néanmoins les plus faibles réductions relatives ont été observées chez les enfants vivant dans des quartiers ayant des taux élevés d’inemploi, de familles à faible revenu et de mères vivant seules. Cependant, ces sous-groupes défavorisés ne présentaient pas une couverture vaccinale plus faible.
CONCLUSIONS: Trois ans après son introduction dans un programme de vaccination universel, le vaccin contre le rotavirus a significativement réduit les gastro-entérites sévères chez les jeunes enfants. Malgré une couverture vaccinale similaire parmi tous les enfants, les groupes socioéconomiquement défavorisés semblent avoir connu une réduction moins prononcée des GEA, suggérant que des facteurs autre que la vaccination peuvent partiellement influencer la réduction de la morbidité reliée à la gastro-entérite chez les jeunes enfants.
Similar content being viewed by others
References
Parashar UD, Gibson CJ, Bresse JS, Glass RI. Rotavirus and severe childhood diarrhea. Emerg Infect Dis 2006;12(2):304–06. PMID: 16494759. doi: 10.3201/eid1202.050006.
Kilgore A, Donauer S, Edwards KM, Weinberg GA, Payne DC, Szilagyi PG, et al. Rotavirus-associated hospitalization and emergency department costs and rotavirus vaccine program impact. Vaccine 2013;31(38):4164–71. PMID: 23845802. doi: 10.1016/j.vaccine.2013.06.085.
Morton VK, Thomas MK, McEWEN SA. Estimated hospitalizations attributed to norovirus and rotavirus infection in Canada, 2006–2010. Epidemiol Infect 2015:143(16):3528–37. PMID: 25991407. doi: 10.1017/S0950268815000734.
Bernard S, Valiquette L, De Wals P, Nault V, Babakissa C, Cyr C, et al. Burden of rotavirus disease: A population-based study in Eastern Townships, Quebec. Can J Infect Dis Med Microbiol 2013;24(3):138–42. PMID: 24421824.
Rivest P, Proulx M, Lonergan G, Lebel MH, Bédard L. Hospitalisations for gastroenteritis: The role of rotavirus. Vaccine 2004;22(15–16):2013–17. PMID: 15121314. doi: 10.1016/j.vaccine.2003.10.029.
National Advisory Committee on Immunization. Updated statement on the use of rotavirus vaccines. Can Commun Dis Rep 2010;36(ACS-4):1–37.
Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z, et al. Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine. N Engl J Med 2006;354(1):23–33. PMID: 16394299. doi: 10. 1056/NEJMoa052664.
Ruiz-Palacios GM, Pérez-Schael I, Velázquez FR, Abate H, Breuer T, Clemens SC, et al. Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. N Engl J Med 2006;354(1):11–22. PMID: 16394298. doi: 10. 1056/NEJMoa052434.
Karafillakis E, Hassounah S, Atchison C. Effectiveness and impact of rotavirus vaccines in Europe, 2006–2014. Vaccine 2015;33(18):2097–107. PMID: 25795258. doi: 10.1016/j.vaccine.2015.03.016.
Rha B, Tate JE, Payne DC, Cortese MM, Lopman BA, Curns AT, et al. Effectiveness and impact of rotavirus vaccines in the United States–2006–2012. Expert Rev Vaccines 2014;13(3):365–76. PMID: 24392657. doi: 10.1586/14760584.2014.877846.
Giaquinto C, Dominiak-Felden G, Van Damme P, Htar Myint TT, Maldonado YA, Spoulou V, et al. Summary of effectiveness and impact of rotavirus vaccination with the oral pentavalent rotavirus vaccine: A systematic review of the experience in industrialized countries. Hum Vaccin 2011;7(7):734–48. PMID: 21734466. doi: 10.4161/hv.7.7.15511.
Esparza-Aguilar M, Gastanaduy PA, Sânchez-Uribe E, Desai R, Parashar UD, Richardson V, et al. Diarrhoea-related hospitalizations in children before and after implementation of monovalent rotavirus vaccination in Mexico. Bull World Health Organ 2014;92(2):117–25. PMID: 24623905. doi: 10.2471/BLT.13.125286.
Gastañaduy PA, Sánchez-Uribe E, Esparza-Aguilar M, Desai R, Parashar UD, Patel M, et al. Effect of rotavirus vaccine on diarrhea mortality in different socioeconomic regions of Mexico. Pediatrics 2013;131(4):e1115–20. PMID: 23460689. doi: 10.1542/peds.2012-2797.
Roy M, Généreux M, Laverdière É, Vanasse A. Surveillance of social and geographic inequalities in housing-related issues: The case of the Eastern Townships, Quebec (Canada). Int J Environ Res Public Health 2014;11(5):4825–44. PMID: 24806192. doi: 10.3390/ijerph110504825.
Hsu VP, Staat MA, Roberts N, Thieman C, Bernstein DI, Bresee J, et al. Use of active surveillance to validate international classification of diseases code estimates of rotavirus hospitalizations in children. Pediatrics, 2005;115(1):78–82. PMID: 15629984.
Statistics Canada. Dissemination Area (DA). 2011 Census Dictionary. Ottawa, ON: Statistics Canada, 2012. Available at: http://www12.statcan.gc.ca/census-recensement/2011/ref/dict/geo021-eng.cfm (Accessed November 24, 2015).
Bettinger JA, Wills K, Le Saux N, Scheitele DW, Halperin SA, Vaudry W. Heterogeneity of rotavirus testing and admitting practices for gastroenteritis among 12 tertiary care pediatric hospitals: Implications for surveillance. Can J Infect Dis Med Microbiol 2011;22(1):15–8. PMID: 22379483.
Desai R, Curns AT, Steiner CA, Tate JE, Patel MM, Parashar UD. All-cause gastroenteritis and rotavirus-coded hospitalizations among US children, 2000–2009. Clin Infect Dis 2012;55(4):e28–34. PMID: 22543022. doi: 10.1093/cid/cis443.
Yen C, Tate JE, Wenk JD, Harris JM, Parashar UD. Diarrhea-associated hospitalizations among US children over 2 rotavirus seasons after vaccine introduction. Pediatrics 2011;127(1):e9–15. PMID: 21172995. doi: 10.1542/peds.2010-1393.
Dey A, Wang H, Menzies R, Macartney K. Changes in hospitalisations for acute gastroenteritis in Australia after the national rotavirus vaccination program. Med J Aust 2012;197(8):453–57. PMID: 23072242. doi: 10.5694/mjal2.10062.
Clarke MF, Davidson GP, Gold MS, Marshall HS. Direct and indirect impact on rotavirus positive and all-cause gastroenteritis hospitalisations in South Australian children following the introduction of rotavirus vaccination. Vaccine 2011;29(29–30):4663–67. 21575665. doi: 10.1016/j.vaccine.2011.04.109.
Payne DC, Szilagyi PG, Staat MA, Edwards KM, Gentsch JR, Weinberg GA, et al. Secular variation in United States rotavirus disease rates and serotypes: Implications for assessing the rotavirus vaccination program. Pediatr Infect Dis J 2009;28(11):948–53. PMID: 19859013. doi: 10.1097/INF.0b013e3181a6ad6e.
Aliabadi N, Tate JE, Haynes AK, Parashar UD. Centers for Disease Control and Prevention (CDC). Sustained decrease in laboratory detection of rotavirus after implementation of routine vaccination—United States, 2000–2014. MMWR Morb Mortal Wkly Rep 2015;64(13):337–42. PMID: 25856253.
Boulianne N, Audet D, Ouakki M. Enquête sur la couverture vaccinale des enfants de 1 an et 2 ans au Québec en 2014. Québec: Institut national de santé publique, 2015. Available at: http://www.inspq.qc.ca/pdf/publications/1973_Enquete_Couverture_Vaccinale_Enfants.pdf (Accessed August 19, 2015).
Poirier B. Rapport de la couverture vaccinale des 0–2 ans en Estrie. Sherbrooke, QC: Direction de santé publique de l’Estrie, 2015. Available at: http://www.santeestrie.qc.ca/sante_publique/protection_maladies_infectieuses/vaccination/documents/RapportCV2014_Estrie_VFACCWeb.pdf (Accessed August 19, 2015).
Guay M, Gallagher F, Petit G, Ménard S, Clément P, Boyer G. Pourquoi les couvertures vaccinales chez les nourrissons de l’estrie sont-elles sous-optimales? Québec: CSSS-IUGS, 2009. Available at: http://www.santeestrie.qc.ca/publication_documentation/documents/etude_couvertures_vaccinales_chez_les_nourrissons_sous-optimales.pdf (Accessed August 19, 2015).
Bradley RH, Corwyn RF. Socioeconomic status and child development. Annu Rev Psychol 2002;53:371–99. PMID: 11752490. doi: 10.1146/annurev.psych.53.100901.135233.
Givon-Lavi N, Ben-Shimol S, Cohen R, Greenberg D, Dagan R. Rapid impact of rotavirus vaccine introduction to the National Immunization Plan in Southern Israel: Comparison between 2 distinct populations. Vaccine 2015;33(16):1934–40. PMID: 25744226. doi: 10.1016/j.vaccine.2015.02.062.
Amre DK, Infante-Rivard C, Gautrin D, Malo J-L. Socioeconomic status and utilization of health care services among asthmatic children. J Asthma 2002;39(7):625–31. PMID: 12442952. doi:10.1081/JAS-120014927.
Author information
Authors and Affiliations
Corresponding author
Additional information
Source of funding: VC was supported by the Eastern Townships Public Health Scholarship from the Fellowship Program of Graduate Studies of the University of Sherbrooke. The funding source had no involvement in any part of the study.
Conflict of Interest: None to declare.
Rights and permissions
About this article
Cite this article
Gosselin, V., Petit, G., Gagneur, A. et al. Trends in severe gastroenteritis among young children according to socio-economic characteristics before and after implementation of a rotavirus vaccination program in Quebec. Can J Public Health 107, e161–e167 (2016). https://doi.org/10.17269/cjph.107.5286
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/cjph.107.5286