Abstract
OBJECTIVE: Prior to the introduction of highly active antiretroviral therapy (HAART), active tuberculosis (TB) was a major contributor to HIV-related morbidity and mortality in Canada and other low-incidence regions. We performed this study to examine TB incidence, clinical manifestations and screening uptake in HIV-infected TB patients during the era of HAART therapy.
METHODS: We performed a retrospective study on all HIV-infected TB patients in British Columbia over a 10-year period (2003–2012). Demographic and clinical characteristics were extracted along with screening and treatment outcomes. Trends in provincial TB incidence, HIV testing and HAART prevalence were also examined.
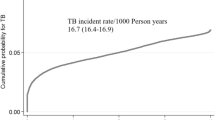
RESULTS: In total, 2,839 TB cases were identified in BC during this period, including 129 HIV-infected TB patients. Surprisingly, only 64 HIV-infected TB patients (50%) had a documented screening tuberculin skin test (TST) prior to TB diagnosis. Of the 39 HIV-infected TB patients with prior TST positivity, 38 (97.4%) had not completed a course of isoniazid preventive therapy. TB incidence decreased significantly in the HIV-infected population of BC over the study period, from 1.9 to 0.5 TB cases per 1,000 HIV-infected individuals (p<0.001).
CONCLUSION: The incidence of HIV-TB decreased significantly over the past decade despite suboptimal latent TB infection screening and prevention practices. This decrease in TB incidence is likely attributable to the increased uptake of HAART. Consideration should be given to intensifying prevention efforts to accelerate TB elimination in HIV-infected populations in low-incidence regions.
Résumé
OBJECTIF : Avant l’avènement de la thérapie antirétrovirale hautement active (TAHA), la tuberculose progressive était l’un des principaux facteurs de morbidité et de mortalité liées au VIH au Canada et dans d’autres régions à faible incidence. Notre étude visait à examiner l’incidence de la tuberculose, ses manifestations cliniques et le recours au dépistage chez les patients tuberculeux infectés par le VIH à l’ère de la TAHA.
MÉTHODE : Nous avons mené une étude rétrospective de tous les patients tuberculeux infectés par le VIH en Colombie-Britannique sur une période de 10 ans (2003–2012). Nous avons extrait leurs caractéristiques démographiques et cliniques, ainsi que les données sur le dépistage et les effets du traitement. Nous avons aussi examiné les tendances de l’incidence de la tuberculose, du dépistage du VIH et de la prévalence de la TAHA dans la province.
RÉSULTATS : En tout, 2 839 cas de tuberculose ont été signalés en C.-B. au cours de la période, dont 129 patients tuberculeux infectés par le VIH. Étonnamment, seuls 64 patients tuberculeux infectés par le VIH (50 %) avaient subi un test cutané à la tuberculine (TCT) consigné en dossier avant leur diagnostic de tuberculose. Sur les 39 patients tuberculeux infectés par le VIH ayant eu un TCT positif au préalable, 38 (97,4 %) n’avaient pas suivi un traitement préventif complet à l’isoniazide. L’incidence de la tuberculose a considérablement diminué dans la population infectée par le VIH en C.-B. au cours de la période de l’étude, passant de 1,9 à 0,5 cas de tuberculose pour 1 000 personnes infectées par le VIH (p<0,001).
CONCLUSION : L’incidence de la comorbidité VIH-tuberculose a considérablement diminué au cours de la dernière décennie malgré les pratiques sous-optimales de prévention et de dépistage de la tuberculose latente. Cette incidence réduite de la tuberculose est probablement imputable au recours accru à la TAHA. Il faudrait envisager d’intensifier les efforts de prévention afin d’accélérer l’élimination de la tuberculose au sein des populations infectées par le VIH dans les régions à faible incidence.
Similar content being viewed by others
References
Barnabas RV, Webb EL, Weiss HA, Wasserheit, JN. The role of coinfections in HIV epidemic trajectory and positive prevention: A systematic review and meta-analysis. AIDS 2011;25(13):1559–73.
Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, et al. The growing burden of tuberculosis: Global trends and interactions with the HIV epidemic. Arch Intern Med 2003;163(9):1009–21.
WHO. Guidelines for intensified tuberculosis case-finding and isoniazid preventive therapy for people living with HIV in resource-constrained settings. Geneva, Switzerland: World Health Organization, 2011.
WHO. Global Tuberculosis Report. Geneva: WHO, 2009.
Metcalfe JZ, Portco TC, Westenhouse J, Damesyn M, Facer M, Hill J, et al. Tuberculosis-HIV Coinfection in California, USA, 1993–2008. Emerging Infect Dis 2013;19(3):400–6.
Menzies D (Ed.). Canadian Tuberculosis Standards, 7th Edition. Can Respir J 2013;20(Suppl A).
Kaplan JE, Benson C, Holmes KH, Brooks JT, Pau A, Masur H. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep 2009;58(RR-4):1–207.
Brassard P, Hottes TS, Lalonde RG, Klein, MB. Tuberculosis screening and active tuberculosis among HIV-infected persons in a Canadian tertiary care centre. Can J Infect Dis Med Microbiol 2009;20(2):51–57.
Lee LM, Lobato MN, Buskin SE, Morse A, Costa, OS. Low adherence to guidelines for preventing TB among persons with newly diagnosed HIV infection, United States. Int J Tuberc Lung Dis 2006;10(2):209–14.
Li J, Munsiff SS, Tarantino T, Dorsinville M. Adherence to treatment of latent tuberculosis infection in a clinical population in New York City. Int J Infect Dis 2010;14(4):e292–7.
Marks SM, Taylor Z, Qualls NL, Shrestha-Kuwahara RJ, Wilce MA, Nguyen CH. Outcomes of contact investigations of infectious tuberculosis patients. Am J Respir Crit Care Med 2000;162(6):2033–38.
Suthar AB, Lawn SD, del Amo J, Getahun H, Dye C, Sculier D, et al. Antiretroviral therapy for prevention of tuberculosis in adults with HIV: A systematic review and meta-analysis. PLoS Med 2012;9(7):e1001270.
Rice B, Elford J, Yin Z, Kruijshaar M, Abubakar I, Lipman M, et al. Decreasing incidence of tuberculosis among heterosexuals living with diagnosed HIV in England and Wales. AIDS 2013;27(7):1151–57.
Badri M, Wilson D, Wood R. Effect of highly active antiretrovi ral therapy on incidence of tuberculosis in South Africa: A cohort study. Lancet 2002;359:2059–64.
Montaner JS, Lima VD, Barrios R, Yip B, Wood E, Kerr T, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: A population-based study. Lancet 2010;376(9740):532–39.
Carpenter CC, Fischl MA, Hammer SM, Hirsch MS, Jacobsen DM, Katzenstein DA, et al. Antiretroviral therapy for HIV infection in 1996. Recommendations of an international panel. International AIDS Society-USA. JAMA 1996;276(2):146–54.
Thompson MA, Aberg JA, Hoy JF, Telenti A, Benson C, Cahn P, et al. Antiretroviral treatment of adult HIV infection: 2012 recommendations of the International Antiviral Society-USA panel. JAMA 2012;308(4):387–402.
Canadian Tuberculosis Reporting System. Reporting form Completion Guidelines version 1.9 For use with: Active Tuberculosis Case Report Form. Available at: http://www.phac-aspc.gc.ca (Accessed September 19, 2013).
Elzi L, Schlegel M, Weber R, Hirschel B, Cavassini M, Schmid P, et al. Reducing tuberculosis incidence by tuberculin skin testing, preventative treatment, and antiretroviral therapy in an area of low tuberculosis transmission. Clin Infect Dis 2007;44(1):94–102.
Aichelburg MC, Reiberger T, Breitenecker F, Mandorfer M, Makristathis A, Rieger A. Reversion and conversion of interferon-gamma release assay results in HIV-1–infected individuals. J Infect Dis 2014:209(5):729–33.
Samandari T, Agizew TB, Nyirenda S, Tedla Z, Sibanda T, Shang N, et al. 6-month versus 36-month isoniazid preventive treatment for tuberculosis in adults with HIV infection in Botswana: A randomised, double-blind, placebocontrolled trial. Lancet 2011;377(9777):1588–98.
Badri M, Wilson D, Wood R. Effect of highly active antiretroviral therapy on incidence of tuberculosis in South Africa: A cohort study. Lancet 2002;359:2059–64.
Golub JE, Pronyk P, Mohapi L, Thsabangu N, Moshabela M, Struthers H, et al. Isoniazid preventive therapy, HAART and tuberculosis risk in HIV-infected adults in South Africa: A prospective cohort. AIDS 2009;23(5):631–36.
Golub JE, Saraceni V, Cavalcante SC, Pacheco AG, Moulton LH, King BS, et al. The impact of antiretroviral therapy and isoniazid preventive therapy on tuberculosis incidence in HIV-infected patients in Rio de Janeiro, Brazil. AIDS 2007;21(11):1441–48.
Jerene D, Naess A, Lindtjorn B. Antiretroviral therapy at a district hospital in Ethiopia prevents death and tuberculosis in a cohort of HIV patients. AIDS Res Ther 2006;7(3):10.
Dembélé M, Saleri N, Carvalho AC, Saouadogo T, Hien AD, Zabsonre I, et al. Incidence of tuberculosis after HAART initiation in a cohort of HIV-positive patients in Burkina Faso. Int J Tuberc Lung Dis 2010;14(3):318–23.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011;365:493–505.
Lannoy LH, Cortez-Escalante JJ, Evangelista Mdo S, Romero, GA. Tuberculosis incidence and risk factors among patients living with HIV/AIDS in public health service institutions in Brasilia, Federal District. Rev Soc Bras Med Trop 2008;41(6):549–55.
Miranda A, Morgan M, Jamal L, Laserson K, Barreira D, Silva G, et al. Impact of antiretroviral therapy on the incidence of tuberculosis: The Brazilian experience, 1995–2001. PLoS ONE 2007;2(9):e826.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of Interest: Dr. Montaner is supported by the British Columbia Ministry of Health and by the US National Institutes of Health (R01DA036307). He has also received limited unrestricted funding from Abbvie, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck, and ViiV Healthcare. Other authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Cheng, M.P., Hirji, A., Roth, D.Z. et al. Tuberculosis in HIV-infected persons in British Columbia during the HAART era. Can J Public Health 105, e258–e262 (2014). https://doi.org/10.17269/cjph.105.4260
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/cjph.105.4260