Abstract
Objective
The aim of this study was to evaluate the safety and efficiency of enucleation (EU) for proximal pancreatic non-invasive neoplasms.
Methods
Patients with solitary non-invasive neoplasms in the proximal pancreas from January 1998 to April 2014 at the Second Affiliated Hospital of Zhejiang University, Hangzhou, China were included. Different operations and outcomes were analyzed.
Results
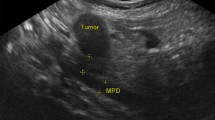
A total of 123 patients were enrolled. Forty patients (32.5%) underwent EU including 18 patients who had tumors close to the main pancreatic duct (MPD). Sixty-one patients (49.6%) had pancreaticoduodenectomy (PD) performed and 22 (17.9%) underwent central pancreatectomy (CP). Pathological outcomes included neuroendocrine tumors, cystic lesions, and solid pseudopapillary tumors. Operation time, intra-operative blood loss, and duration of hospital stay were significantly reduced in the EU group. PD was associated with the greatest complication rate (55.7%), followed by EU (50%) and CP (40.9%), though the pancreatic fistula rate after EU was the highest (50%), especially in patients with tumors larger than 3 cm and tumors close to the MPD. EU had advantages in the preservation of pancreatic parenchyma and endocrine and exocrine function.
Conclusions
EU can be carried out safely and effectively for tumors in the proximal pancreas with improved outcomes compared with standard resections, even if the tumor is larger than 3 cm and close to the MPD.
摘要
目 的
评价近端胰腺非侵袭性肿瘤剜除手术的安全性与有效性。
创新点
以目前为止最大样本量的近端胰腺非侵袭性肿瘤的剜除手术的数据分析, 证实了剜除手术在这类患者中的安全性和有效性, 即使肿瘤直径> 3 cm 或临近主胰管肿瘤。 并且首次报道和证实了在这些患者剜除手术中发生主胰管损伤, 进行主胰管修补与支架置入是安全有效的。分析了同期进行不同手术方式患者的肿瘤资料, 阐明了肿瘤大小影响手术策略的制定。
方 法
详细对比了剜除手术和传统的胰十二脂肠切除术以及胰腺中段切除术的术前情况、 术中情况、 术后并发症资料 (表1~3), 尤其详细描述了临近主胰管和主胰管有损伤的患者剜除手术后并发症情况 (表4)。 同时, 附图说明了主胰管修补手术方法 (图1)。
结 论
近端胰腺非侵袭性肿瘤的剜除手术是安全有效的, 应该是这类患者手术治疗的首选推荐方式, 在大肿瘤和临近主胰管的肿瘤患者中也可施行。
Similar content being viewed by others
References
Atema, J.J., Jilesen, A.P., Busch, O.R., et al., 2015. Pancreatic fistulae after pancreatic resections for neuroendocrine tumours compared with resections for other lesions. HPB, 17(1): 38–45. http://dx.doi.org/10.1111/hpb.12319
Bassi, C., Dervenis, C., Butturini, G., et al., 2005. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery, 138(1): 8–13. http://dx.doi.org/10.1016/j.surg.2005.05.001
Beger, H.G., Poch, B., Vasilescu, C., 2014. Benign cystic neoplasm and endocrine tumours of the pancreas—when and how to operate—an overview. Int. J. Surg., 12(6): 606–614. http://dx.doi.org/10.1016/j.ijsu.2014.03.020
Brient, C., Regenet, N., Sulpice, L., et al., 2012. Risk factors for postoperative pancreatic fistulization subsequent to enucleation. J. Gastrointest. Surg., 16(10): 1883–1887. http://dx.doi.org/10.1007/s11605-012-1971-x
Butte, J.M., Brennan, M.F., Gönen, M., et al., 2011. Solid pseudopapillary tumors of the pancreas. Clinical features, surgical outcomes, and long-term survival in 45 consecutive patients from a single center. J. Gastrointest. Surg., 15(2): 350–357. http://dx.doi.org/10.1007/s11605-010-1337-1
Casadei, R., Ricci, C., Rega, D., et al., 2010. Pancreatic endocrine tumors less than 4 cm in diameter: resect or enucleate? A single-center experience. Pancreas, 39(6): 825–828. http://dx.doi.org/10.1097/MPA.0b013e3181cf155c
Cauley, C.E., Pitt, H.A., Ziegler, K.M., et al., 2012. Pancreatic enucleation: improved outcomes compared to resection. J. Gastrointest. Surg., 16(7): 1347–1353. http://dx.doi.org/10.1007/s11605-012-1893-7
Crippa, S., Bassi, C., Salvia, R., et al., 2007. Enucleation of pancreatic neoplasms. Br. J. Surg., 94(10): 1254–1259. http://dx.doi.org/10.1002/bjs.5833
Crippa, S., Boninsegna, L., Partelli, S., et al., 2010. Parenchymasparing resections for pancreatic neoplasms. J. Hepatobiliary Pancreat. Sci., 17(6): 782–787. http://dx.doi.org/10.1007/s00534-009-0224-1
Dong, X., Gao, S.L., Xie, Q.P., et al., 2008. In situ highvolume modified continuous closed and/or open lavage for infected necrotizing pancreatitis. Pancreas, 36(1): 44–49. http://dx.doi.org/10.1097/mpa.0b013e31812e9688
Falconi, M., Zerbi, A., Crippa, S., et al., 2010. Parenchymapreserving resections for small nonfunctioning pancreatic endocrine tumors. Ann. Surg. Oncol., 17(6): 1621–1627. http://dx.doi.org/10.1245/s10434-010-0949-8
Ferrone, C.R., Tang, L.H., Tomlinson, J., et al., 2007. Determining prognosis in patients with pancreatic endocrine neoplasms: can the WHO classification system be simplified? J. Clin. Oncol., 25(35): 5609–5615. http://dx.doi.org/10.1200/JCO.2007.12.9809
Ge, C., Luo, X., Chen, X., et al., 2010. Enucleation of pancreatic cystadenomas. J. Gastrointest. Surg., 14(1): 141–147. http://dx.doi.org/10.1007/s11605-009-1023-3
Ghaneh, P., Neoptolemos, J.P., 1999. Exocrine pancreatic function following pancreatectomy. Ann. N. Y. Acad. Sci., 880: 308–318.
Goasguen, N., Bourrier, A., Ponsot, P., et al., 2009. Endoscopic management of pancreatic fistula after distal pancreatectomy and enucleation. Am. J. Surg., 197(6): 715–720. http://dx.doi.org/10.1016/j.amjsurg.2008.03.005
Grobmyer, S.R., Pieracci, F.M., Allen, P.J., et al., 2007. Defining morbidity after pancreaticoduodenectomy: use of a prospective complication grading system. J. Am. Coll. Surg., 204(3): 356–364. http://dx.doi.org/10.1016/j.jamcollsurg.2006.11.017
Hackert, T., Hinz, U., Fritz, S., et al., 2011. Enucleation in pancreatic surgery: indications, technique, and outcome compared to standard pancreatic resections. Langenbeck’s Arch. Surg., 396(8): 1197–1203. http://dx.doi.org/10.1007/s00423-011-0801-z
Heeger, K., Falconi, M., Partelli, S., et al., 2014. Increased rate of clinically relevant pancreatic fistula after deep enucleation of small pancreatic tumors. Langenbeck’s Arch. Surg., 399(3): 315–321. http://dx.doi.org/10.1007/s00423-014-1171-0
Ho, V., Heslin, M.J., 2003. Effect of hospital volume and experience on in-hospital mortality for pancreaticoduodenectomy. Ann. Surg., 237(4): 509–514. http://dx.doi.org/10.1097/01.SLA.0000059981.13160.97
Howard, J.M., Hess, W., 2002. History of the Pancreas: Mystery of a Hidden Organ. Kluwer Academic/Plenum Publisher, New York.
Inchauste, S.M., Lanier, B.J., Libutti, S.K., et al., 2012. Rate of clinically significant postoperative pancreatic fistula in pancreatic neuroendocrine tumors. World J. Surg., 36(7): 1517–1526. http://dx.doi.org/10.1007/s00268-012-1598-9
Kiely, J.M., Nakeeb, A., Komorowski, R.A., et al., 2003. Cystic pancreatic neoplasms: enucleate or resect? J. Gastrointest. Surg., 7(7): 890–897. http://dx.doi.org/10.1007/s11605-003-0035-7
Kulke, M.H., Benson, A.B.3rd, Bergsland, E., et al., 2012. Neuroendocrine tumors. J. Natl. Compr. Canc. Netw., 10(6): 724–764.
le Borgne, J., de Calan, L., Partensky, C., 1999. Cystadenomas and cystadenocarcinomas of the pancreas: a multiinstitutional retrospective study of 398 cases. French Surgical Association. Ann. Surg., 230(2): 152–161.
Lu, W.J., Xu, B., Gao, S.L., et al., 2012. Enucleation of benign or borderline pancreatic head tumors adjacent to the common pancreatic duct. Pancreas, 41(2): 336–337. http://dx.doi.org/10.1097/MPA.0b013e318229b891
Madan, A.K., Weldon, C.B., Long, W.P., et al., 2004. Solid and papillary epithelial neoplasm of the pancreas. J. Surg. Oncol., 85(4): 193–198. http://dx.doi.org/10.1002/jso.20019
Norton, J.A., 2006. Surgery for primary pancreatic neuroendocrine tumors. J. Gastrointest. Surg., 10(3): 327–331. http://dx.doi.org/10.1016/j.gassur.2005.08.023
Papavramidis, T., Papavramidis, S., 2005. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. J. Am. Coll. Surg., 200(6): 965–972. http://dx.doi.org/10.1016/j.jamcollsurg.2005.02.011
Pitt, S.C., Pitt, H.A., Baker, M.S., et al., 2009. Small pancreatic and periampullary neuroendocrine tumors: resect or enucleate? J. Gastrointest. Surg., 13(9): 1692–1698. http://dx.doi.org/10.1007/s11605-009-0946-z
Ramage, J.K., Davies, A.H., Ardill, J., et al., 2005. Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours. Gut, 54: iv1–iv16. http://dx.doi.org/10.1136/gut.2004.053314
Reid-Lombardo, K.M., Ramos-de la Medin, A., Thomsen, K., et al., 2007. Long-term anastomotic complications after pancreaticoduodenectomy for benign diseases. J. Gastrointest. Surg., 11(12): 1704–1711. http://dx.doi.org/10.1007/s11605-007-0369-7
Schmidt, C.M., White, P.B., Waters, J.A., et al., 2007. Intraductal papillary mucinous neoplasms: predictors of malignant and invasive pathology. Ann. Surg., 246(4): 644–654. http://dx.doi.org/10.1097/SLA.0b013e318155a9e5
Sciaudone, G., Perniceni, T., Lévy, P., et al., 2000. Enucleation of intraductal papillary-mucinous tumor of the head of the pancreas. Report of 2 cases. Gastroenterol. Clin. Biol., 24(1): 121–124 (in French).
Talamini, M.A., Moesinger, R., Yeo, C.J., et al., 1998. Cystadenomas of the pancreas: is enucleation an adequate operation? Ann. Surg., 227(6): 896–903.
Tran, T.C., van Lanschot, J.J., Bruno, M.J., et al., 2009. Functional changes after pancreatoduodenectomy: diagnosis and treatment. Pancreatology, 9(6): 729–737. http://dx.doi.org/10.1159/000264638
Turrini, O., Schmidt, C.M., Pitt, H.A., et al., 2011. Side-branch intraductal papillary mucinous neoplasms of the pancreatic head/uncinate: resection or enucleation? HPB, 13(2): 126–131. http://dx.doi.org/10.1111/j.1477-2574.2010.00256.x
Valsangkar, N.P., Morales-Oyarvide, V., Thayer, S.P., et al., 2012. 851 resected cystic tumors of the pancreas: a 33-year experience at the Massachusetts General Hospital. Surgery, 152(3 Suppl.):S4–S12. http://dx.doi.org/10.1016/j.surg.2012.05.033
Wente, M.N., Veit, J.A., Bassi, C., et al., 2007a. Postpancreatectomy hemorrhage (PPH)—an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery, 142(1): 20–25. http://dx.doi.org/10.1016/j.surg.2007.02.001
Wente, M.N., Bassi, C., Dervenis, C., et al., 2007b. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery, 142(5): 761–768. http://dx.doi.org/10.1016/j.surg.2007.05.005
Yan, J.F., Kuang, T.T., Ji, D.Y., et al., 2015. Laparoscopic versus open distal pancreatectomy for benign or premalignant pancreatic neoplasms: a two-center comparative study. J. Zhejiang Univ.-Sci. B (Biomed. & Biotechnol.), 16(7): 573–579. http://dx.doi.org/10.1631/jzus.B1400257
Zhang, T., Xu, J., Wang, T., et al., 2013. Enucleation of pancreatic lesions: indications, outcomes, and risk factors for clinical pancreatic fistula. J. Gastrointest. Surg., 17(12): 2099–2104. http://dx.doi.org/10.1007/s11605-013-2355-6
Author information
Authors and Affiliations
Corresponding author
Additional information
Project supported by the National Natural Science Foundation of China (Nos. 30672072 and 30872531), the Foundation of Science and Technology Department of Zhejiang Province, China (Nos. 2014C 33187), and the National High-Tech R&D Program (863) of China (No. 2007AA02Z476)
Rights and permissions
About this article
Cite this article
Lu, Wj., Cai, Hl., Ye, Md. et al. Enucleation of non-invasive tumors in the proximal pancreas: indications and outcomes compared with standard resections. J. Zhejiang Univ. Sci. B 18, 906–916 (2017). https://doi.org/10.1631/jzus.B1600597
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1631/jzus.B1600597