Abstract
Background and Objective
This study examined the relationship between body mass index (BMI) and sarcopenia with oral function decline in older patients as well as whether a combination of underweight BMI and sarcopenia was associated with decreased oral function in individuals with conservative restorative and prosthetic treatment for masticatory disorders.
Design, Setting, And Participants
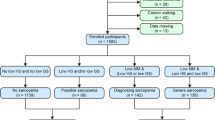
This cross-sectional study included 290 older Japanese patients who regularly attended a general dental clinic. A detailed examination of oral function, sarcopenia, and BMI according to the Asian Working Group for Sarcopenia 2019 criteria was conducted for patients aged 65 years. This study used odds ratios as an epidemiological measure in the cross-sectional survey.
Results
Multinomial logistic regression analysis showed that the number of remaining teeth and tongue pressure was associated with both ideal and overweight BMI in individuals with sarcopenia when compared to healthy individuals. The underweight BMI plus sarcopenia group was associated with tongue and lip motor function [ka] sound test, swallowing function, and the presence of oral hypofunction.
Discussion
Our findings indicated that various aspects of oral function were impaired in community-dwelling older adult Japanese patients with sarcopenia and underweight BMI. Notably, among older adults with sarcopenia, both obese and thin patients exist, suggesting that distinct pathophysiological mechanisms influence oral function.
Conclusion
The above findings support the hypothesis that the coexistence of sarcopenia and underweight BMI is associated with poor oral function. Regular oral function assessments and weight measurements in general dental practice can aid the prompt identification of sarcopenia and reduced swallowing function and can facilitate early intervention. The presence of sarcopenia and impaired swallowing function should be considered in patients with underweight BMI, reduced [ka] sound, and low tongue pressure following a thorough oral function examination.


Similar content being viewed by others
References
Cabinet Office, Status of ageing population and implementation of ageing society measures in 2020, In White Paper on Ageing Society, Government of Japan, 2021. Tokyo, Japan.
Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NHJ. Tooth loss and oral health-related quality of life: A systematic review and meta-analysis. Health Qual Life Outcomes 2010;8:126. doi: https://doi.org/10.1186/1477-7525-8-126.
Chang KV, Wu WT, Chen LR, Wang HI, Wang TG, Han DS. Suboptimal tongue pressure is associated with risk of malnutrition in community-dwelling older individuals. Nutrients 2021;13:1821. doi: https://doi.org/10.3390/nu13061821.
Kwon SH, Park HR, Lee YM, et al. Difference in food and nutrient intakes in Korean elderly people according to chewing difficulty: using data from the Korea National Health and Nutrition Examination Survey 2013 (6th). Nutr Res Pract 2017;11:139–146. 2017. doi: https://doi.org/10.4162/nrp.2017.11.2.139.
Tamura F, Kikutani T, Tohara T, Yoshida M, Yaegaki K. Tongue thickness relates to nutritional status in the elderly. Dysphagia 2012;27:556–561. doi: https://doi.org/10.1007/s00455-012-9407-z.
Inomata C, Ikebe K, Kagawa R, et al. Significance of occlusal force for dietary fibre and vitamin intakes in independently living 70-year-old Japanese: From SONIC Study. J Dent 2014;42:556–564. doi: https://doi.org/10.1016/j.jdent.2014.02.015.
Ney DM, Weiss JM, Kind AJ, Robbins J. Senescent swallowing: impact, strategies, and interventions. Nutr Clin Pract 2009;24:395–413. doi: https://doi.org/10.1177/0884533609332005.
Hirata Y, Nomura K, Kato D, et al. A Piezo1/KLF15/IL-6 axis mediates immobilization-induced muscle atrophy. J Clin Invest 2022;132:1–13. doi: https://doi.org/10.1172/JCI154611.
Xue QL, Bandeen-Roche K, Varadhan R, Zhou J, Fried LP. Initial manifestations of frailty criteria and the development of frailty phenotype in the women’s health and aging Study II. J Gerontol A Biol Sci Med Sci 2008;63:984–990. doi: https://doi.org/10.1093/gerona/63.9.984.
Tanaka T, Takahashi K, Hirano H, et al. Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med Sci 2018;73:1661–1667. doi: https://doi.org/10.1093/gerona/glx225.
Ministry of Health, Labor and Welfare. Dietary Intake Standards for Japanese, Ver 2020. Government of Japan: Tokyo, Japan, 2020.
Sato Y, Kitagawa N, Shichita T. Examination and management of oral hypofunction in Japanese. Ann Jpn Prosthodont Soc 2020;12:144–149. doi: https://doi.org/10.2186/ajps.12.144.
Kitamura A, Seino S, Abe T, et al. Sarcopenia: Prevalence, associated factors, and the risk of mortality and disability in Japanese olderadults. J Cachexia Sarcopenia Muscle 2021;12:30–38. doi: https://doi.org/10.1002/jcsm.12651.
Go SW, Cha YH, Lee JA, Park HS. Association between sarcopenia, bone density, and health-related quality of life in Korean men. Korean J Fam Med 2013;34:281–288. doi: https://doi.org/10.4082/kjfm.2013.34.4.281.
Tanimura K, Sato S, Fuseya Y, et al. Quantitative assessment of erector spinae muscles in patients with chronic obstructive pulmonary disease. Novel chest computed tomography-derived index for prognosis. Ann Am Thorac Soc 2016;13:334–341. doi: https://doi.org/10.1513/AnnalsATS.201507-446OC.
Kugimiya Y, Iwasaki M, Ohara Y, et al. Association between sarcopenia and oral functions in community-dwelling older adults: Across-sectional study. J Cachexia Sarcopenia Muscle 2023;14:429–438. doi: https://doi.org/10.1002/jcsm.13145.
Fujishima I, Fujiu-Kurachi M, Arai H, et al. Sarcopenia and dysphagia: Position paper by four professional organizations. Geriatr Gerontol Int 2019;19:91–97. doi: https://doi.org/10.1111/ggi.13591.
Hirahata N. What is dysphagia in sarcopenia? in Japanese. Nursing Technology. Jpn J Nurs Sci 2019;65:28–31.
Shirahase R, Watanabe Y, Saito T, et al. A cross-sectional study on the relationship between oral function and sarcopenia in Japanese patients with regular dental maintenance. Int J Environ Res Public Health 2022;19:5178. doi: https://doi.org/10.3390/ijerph19095178.
Kikutani T. Dental Practice aimed at nutritional improvement for the motor masticatory disturbance. Ann Jpn Prosthodont Soc 2015;7:102–105. doi: https://doi.org/10.2186/ajps.7.102.
Watanabe Y. How decline in oral function can be assessed and prevented? in Japanese. Gen Rehabil 2022;50:937–944.
Ministry of Health, Labor and Welfare. Survey of Dental Diseases in Japan, Ver. 2016. Government of Japan, 2017. Tokyo, Japan.
Minakuchi S, Tsuga K, Ikebe K, et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology 2018;35:317–324. doi: https://doi.org/10.1111/ger.12347.
Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc 2020;21:300–307.e2. doi: https://doi.org/10.1016/j.jamda.2019.12.012.
Imai R, Fukai K. A study of bleeding index for clinical application. J Jpn Soc Periodontal 2003;45:229–240. doi: https://doi.org/10.2329/perio.45.229.
Maekawa K, Ikeuchi T, Shinkai S, et al. Number of functional teeth more strongly predicts all-cause mortality than number of present teeth in Japanese older adults. Geriatr Gerontol Int 2020;20:607–614. doi: https://doi.org/10.1111/ggi.13911.
Hirano H, Watanabe Y, Ishiyama N, Watanabe I, Suzuki T, Nasu I. Analysis of factors affecting chewing ability in the elderly. Gerodontics 1995;9:184–190. doi: https://doi.org/10.11259/jsg1987.9.184.
Shimizu T, Ueda T, Sakurai K. New method for evaluation of tongue-coating status. J Oral Rehabil 2007;34:442–447. doi: https://doi.org/10.1111/j.1365-2842.2007.01733.x.
Yamada H, Nakagawa Y, Nomura Y, et al. Preliminary results of moisture checker for Mucus in diagnosing dry mouth. Oral Dis 2005;11:405–407. Doi: https://doi.org/10.1111/j.1601-0825.2005.01136.x.
Yamada A, Kanazawa M, Komagamine Y, Minakuchi S. Association between tongue and lip functions and masticatory performance in young dentate adults. J Oral Rehabil 2015;42:833–839. doi: https://doi.org/10.1111/joor.12319.
Yoshikawa M, Fukuoka T, Mori T, et al. Comparison of the Iowa oral performance instrument and JMS tongue pressure measurement device. J Dent Sci 2021;16:214–219. doi: https://doi.org/10.1016/j.jds.2020.06.005.
Uesugi H, Shiga H. Relationship between masticatory performance using a gummy jelly and masticatory movement. J Prosthodont Res 2017;61:419–425. doi: https://doi.org/10.1016/j.jpor.2017.01.001.
Ohkuma R, Fujishima I, Kojima C, Hojo K, Takehara I, Motohashi Y. Development of a questionnaire to screen dysphagi. Jpn J Dysphagia Rehabilitation 2022;6:3–8.doi: https://doi.org/10.32136/jsdr.6.1_3.
Nakamura M, Hamada T, Tanaka A, et al. Association of oral hypofunction with frailty, sarcopenia, and mild cognitive impairment: A cross-sectional study of community-dwelling Japanese older adults. J Clin Med 2021;10:1626. doi: https://doi.org/10.3390/jcm10081626.
Minakuchi S, Tsuga K, Ikebe K, et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology 2028;35:317–324. doi: https://doi.org/10.1111/ger.12347.
Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175–191. doi: https://doi.org/10.3758/bf03193146.
Gilmour MM. Using causal diagrams to understand common problems in social epidemiology. Oakes JM, Kaufman JS (ed). In Methods in Social Epidemiology, 2nd edit 2017. Jossey-Bass, San Francisco, CA, USA, pp. 458–492.
Sakai K, Nakayama E, Tohara H, et al. Diagnostic accuracy of lip force and tongue strength for sarcopenic dysphagia in older inpatients: A cross-sectional observational study. Clin Nutr 2016;38:1078–1083. doi: https://doi.org/10.1016/j.clnu.2018.01.016.
Sakai K, Nakayama E, Tohara H, et al. Relationship between tongue strength, lip strength, and nutrition-related sarcopenia in older rehabilitation inpatients: A cross-sectional study. Clin Interv Aging 2017;12, 1207–1214. doi: https://doi.org/10.2147/CIA.S141148.
Tsushima E. Medical Data analysis, 2021. Tokyo Shobo, Tokyo, Japan.
León S, Giacaman RA. Proposal for a conceptual framework for the development of geriatric dentistry. J Dent Res 2022;101:247–252. doi: https://doi.org/10.1177/00220345211042268.
Cha S, Kim WS, Kim KW, et al. Sarcopenia is an independent risk factor for dysphagia in community-dwelling older adults. Dysphagia 2019;34:692–697. doi: https://doi.org/10.1007/s00455-018-09973-6.
Suzuki M, Kimura Y, Otobe Y, et al. Relationship between sarcopenia and swallowing capacity in community-dwelling older women. Gerontol 2020;66:549–552. doi: https://doi.org/10.1159/000511359.
Batsis JA, Villareal DT. Sarcopenic obesity in older adults: A etiology, epidemiology and treatment strategies. Nat Rev Endocrinol 2018;14:513–537. doi: https://doi.org/10.1038/s41574018-0062-9.
Matsuo K, Taniguchi H, Nakagawa M, et al. Association between oral function decline and undernutrition in elderly patients admitted to acute care hospitals, in Japanese. Geriatr Dent 2016;31:123–133. doi: https://doi.org/10.11259/jsg.31.123.
Wakai K, Naito M, Naito T, et al. Tooth loss and intakes of nutrients and foods: A nationwide survey of Japanese dentists. Community Dent Oral Epidemiol 2010;38:43–49. doi: https://doi.org/10.1111/j.1600-0528.2009.00512.x.
Mizuguchi T, Tsuga K, Ikebe K, et al. Oral functional decline in old age - Society opinion paper, 2016 edit, in Japanese. Geriatric Dentistry 2016;31:81–99. doi: https://doi.org/10.11259/jsg.31.81.
Takeuchi N, Sawada N, Ekuni D, Morita M. Oral factors as predictors of frailty in community-dwelling older people: A prospective cohort study. Int J Environ Res Public Health 2022;19:1145. doi: https://doi.org/10.3390/ijerph19031145.
Ito K, Yoshihara A, Takano N, et al. Comparison of methods for the measurement of oral diadochokinesis, in Japanese. Geriatr Dent 2009;24:48–54. doi: https://doi.org/10.11259/jsg.24.48.
Chen KC, Lee TM, Wu WT, Wang TG, Han DS, Chang KV. Assessment of tongue strength in sarcopenia and sarcopenic dysphagia: A systematic review and meta-analysis. Front Nutr 2021;8:684840. doi: https://doi.org/10.3389/fnut.2021.684840.
Matsuo K. Response to oral hypofunction and future directions, in Japanese. Gerontol Geriatr Med 2018;33:304–311. doi: https://doi.org/10.11259/jsg.33.304.
Okuno K, Kobuchi R, Morita S, Masago A, Imaoka M, Takahashi K. Relationships between the nutrition status and oral measurements for sarcopenia in older Japanese adults. J Clin Med 2022;11:7382. doi: https://doi.org/10.3390/jcm11247382.
Ikebe K, Hatta K, Mihara Y, Murakami K. Discussion paper on ‘Oral hypofunction’, in Japanese. Geriatr Dent 2020;34:451–456. doi: https://doi.org/10.11259/jsg.34.451.
Yoshida D, Suzuki T, Shimada H, et al. Using two different algorithms to determine the prevalence of sarcopenia. Geriatr Gerontol Int 2014;14:46–51. doi: https://doi.org/10.1111/ggi.12210.
Watanabe Y, Hirano H, Arai H, et al. Relationship between frailty and oral function in community-dwelling elderly adults. J Am Geriatr Soc 2017;65:66–76. doi: https://doi.org/10.1111/jgs.14355.
Iwasaki M, Ohara Y, Motokawa K, et al. Population-based reference values for tongue pressure in Japanese older adults: A pooled analysis of over 5,000 participants. J Prosthodont Res 2023;67:62–69. doi:https://doi.org/10.2186/jpr.JPR_D_21_00272.
Hokkaido National Health Insurance Federation. Obihiro City National Health Insurance Specific Health Examination, 2015. Hokkaido, Japan.
Docherty M, Smith R. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. BMJ 2018;35:317–324. doi: https://doi.org/10.1111/ger.12347.
Ministry of Health, Labour and Welfare, Japan. Summary of the results of the survey on dental diseases in 2008. Government of Japan: Tokyo, Japan, 2021.
Minakuchi S, Tsuga K, Ikebe K, et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontol 2018;35:317–324. doi: https://doi.org/10.1111/ger.12347.
Offenbacher S, Barros SP, Singer RE, Moss K, Williams RC, Beck JD. Periodontal disease at the biofilm-gingival interface. J Periodontol 2007;78:1911–1925. doi: https://doi.org/10.1902/jop.2007.060465.
Petersen PK, Yamamoto T, Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2005;33:81–92. doi: https://doi.org/10.1111/j.1600-0528.2004.00219.x.
Acknowledgments
We would like to thank Gerodontology, Department of Oral Health Science, Faculty of Dental Medicine, Hokkaido University and Tsugayasu Dental Clinic, Medical Corporation Shuwakai for their support. In addition, we would like to thank Editage (https://www.editage.com) for English language editing services.
Funding
Funding: This research received no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest: The authors declare no conflicts of interest.
Additional information
Institutional review board statement: This study was conducted in accordance with the guidelines of the Declaration of Helsinki. The study protocol was approved by the Ethical Review Committee for Clinical and Epidemiological Research of the Faculty of Dentistry, Hokkaido University (Approval no. 2019-4).
Rights and permissions
About this article
Cite this article
Matsushita, Y., Watanabe, Y., Shirahase, R. et al. Relationship between Body Mass Index and Sarcopenia with Oral Function Decline in Older Japanese Patients Who Regularly Attend a General Dental Clinic. J Frailty Aging 13, 21–30 (2024). https://doi.org/10.14283/jfa.2024.5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jfa.2024.5