Abstract
Background
Pancreatic adenocarcinoma located in the pancreatic body might require a portomesenteric venous resection (PVR), but data regarding surgical risks after distal pancreatectomy (DP) with PVR are sparse. Insight into additional surgical risks of DP-PVR could support preoperative counseling and intraoperative decision making. This study aimed to provide insight into the surgical outcome of DP-PVR, including its potential risk elevation over standard DP.
Methods
We conducted a retrospective, multicenter study including all patients with pancreatic adenocarcinoma who underwent DP ± PVR (2018–2020), registered in four audits for pancreatic surgery from North America, Germany, Sweden, and The Netherlands. Patients who underwent concomitant arterial and/or multivisceral resection(s) were excluded. Predictors for in-hospital/30-day major morbidity and mortality were investigated by logistic regression, correcting for each audit.
Results
Overall, 2924 patients after DP were included, of whom 241 patients (8.2%) underwent DP-PVR. Rates of major morbidity (24% vs. 18%; p = 0.024) and post-pancreatectomy hemorrhage grade B/C (10% vs. 3%; p = 0.041) were higher after DP-PVR compared with standard DP. Mortality after DP-PVR and standard DP did not differ significantly (2% vs. 1%; p = 0.542). Predictors for major morbidity were PVR (odds ratio [OR] 1.500, 95% confidence interval [CI] 1.086–2.071) and conversion from minimally invasive to open surgery (OR 1.420, 95% CI 1.032–1.970). Predictors for mortality were higher age (OR 1.087, 95% CI 1.045–1.132), chronic obstructive pulmonary disease (OR 4.167, 95% CI 1.852–9.374), and conversion from minimally invasive to open surgery (OR 2.919, 95% CI 1.197–7.118), whereas concomitant PVR was not associated with mortality.
Conclusions
PVR during DP for pancreatic adenocarcinoma in the pancreatic body is associated with increased morbidity, but can be performed safely in terms of mortality.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Pancreatic adenocarcinoma may present with involvement of the portomesenteric vein.1 Nowadays, major venous tumor involvement is not considered a contraindication for surgical resection,2,3 particularly due to the increasing use of preoperative chemotherapy and improved surgical techniques.4 Since approximately two-thirds of the pancreatic adenocarcinomas are located in the pancreatic head,5 pancreatoduodenectomy (PD) with portomesenteric venous resection (PVR) is the most commonly performed procedure in patients with portomesenteric venous involvement. PD-PVR is associated with similar or slightly elevated surgical risks in comparison with standard PD without PVR.6,7,8 However, evidence on pancreatic adenocarcinoma located in the pancreatic body requiring a distal pancreatectomy (DP) with concomitant PVR is sparse and is thus far based only on single-center series.9,10,11,12
DP-PVR is a rarely performed procedure,11,13 which comprises 4–13% of all pancreatectomies where a concomitant PVR is needed.14,15,16,17,18,19,20 Performing DP-PVR is challenging due to restricted mobilization of the portomesenteric venous axis as the pancreatic head remains in situ. Depending on the tumor size, surgeons may consider an extended PD, or total pancreatectomy (TP) could be considered as alternatives to facilitate the venous reconstruction; however, TP is associated with endocrine and exocrine insufficiency,21 although these are more manageable nowadays with acceptably reduced quality of life.22,23 Moreover, PD is associated with higher risks for major morbidity and mortality in comparison with DP.24,25
More insight into the surgical outcome after DP-PVR in comparison with standard DP is needed for preoperative counseling and surgical decision making. Therefore, the present international observational study aimed to compare the surgical outcome after DP-PVR versus standard DP.
Methods
This retrospective, observational, multicenter study was performed following the Strengthening the Reporting of Observational Studies (STROBE) guidelines.26 Informed consent was not necessary owing to the use of anonymous datasets.
Study Design and Patients
All patients who were registered in the four registries of the Global Audits on Pancreatic Surgery Group (GAPASURG)27 between 2018 and 2020 who underwent DP for pancreatic adenocarcinoma were included, with or without PVR. Patients were included regardless of the surgical approach (i.e., minimally invasive or open), and regardless of upfront surgery or surgery following preoperative chemo(radio)therapy. Patients were excluded in the case of concomitant colon, gastric, and/or arterial resection(s),28,29 and/or a histopathological diagnosis other than pancreatic adenocarcinoma.
The GAPASURG database comprises the following four registries: (1) North America (American College of Surgeons National Surgical Quality Improvement Program [NSQIP], multicenter, 160 centers in 2019), Germany (Deutsche Gesellschaft für Allgemein- und Viszeralchirurgie—Studien-, Dokumentations-und Qualitätszentrum [StuDoQ]30, multicenter, 58 centers in 2019), Sweden (Swedish National Pancreatic and Periampullary Cancer Registry,31 nationwide, 6 centers in 2020), and The Netherlands (Dutch Pancreatic Cancer Audit,32 nationwide, 17 centers in 2019). Differences in registry design among these four registries are presented in “Appendix 1”.
Endpoints
The primary endpoints were in-hospital/30-day mortality and major morbidity, while secondary endpoints concerned pancreas surgery-specific complications (i.e., post-pancreatectomy hemorrhage [PPH], postoperative pancreatic fistula [POPF], delayed gastric emptying [DGE]), relaparotomy rate, length of hospital stay, and rate of readmission.
Definitions
Differences in parameters between registries due to the different metric systems were resolved by converting the data; ounces were converted to kilograms and inches into meters. Several variables were recategorized, such that data could be combined.
The Eastern Cooperative Oncology Group (ECOG) performance status was recategorized to match functional health status of being independent (ECOG 0–1), partially dependent (ECOG 2–3), and totally dependent (ECOG 4). In addition, the American Society of Anesthesiologists performance status (ASA-PS) is used.
Hospital volumes for pancreatic surgery are classified based on the annual number of PDs performed; dichotomized into low-volume (i.e., < 40 PDs/year) and high-volume (i.e., ≥ 40 PDs/year) hospitals. The annual PD volume was used as this better illustrates the experience with more complex pancreatic surgery compared with the annual DP volume.33 Not all registries contained information on the type of PVR resection and reconstruction;3 therefore, no distinction is made between the PVR type. Furthermore, portomesenteric venous tangential resections with primary closure (International Study Group of Pancreatic Surgery [ISGPS] type 1)3 are not included in the NSQIP as PVR.
All complications and mortality were measured during a 30-day postoperative follow-up. In addition, in-hospital events, when hospital stay exceeded > 30 days, were registered, except within the NSQIP, in which only 30-day follow-up was registered. Major morbidity was defined as Clavien–Dindo grade IIIa or higher.34 Pancreas surgery-specific complications (i.e., POPF, DGE, and PPH) were defined in accordance with the ISGPS definitions, whereby grade B/C is considered as clinically relevant.35,36,37 Readmission was defined as any readmission (i.e., to the same or another hospital) for any reason within 30 days after the principal operative procedure.
Within North America, Germany, and The Netherlands, the American Joint Committee on Cancer (AJCC) TNM 8th edition was used to determine the T and N stage, whereas Sweden used the AJCC 7th edition. For the current study, the (y)pTNM parameters are categorized into T0–T3 versus T4, and N0 versus N1–2. Resection margin status (R status) was defined following the Royal College of Pathologists definition.38
Statistical Analyses
Statistical analyses were performed using IBM SPSS Statistics for Windows (version 28.0.1.1; IBM Corporation, Armonk, NY, USA). Statistical significance was reached in case of a two-tailed p value < 0.050.
Categorical variables are presented as percentages and frequencies, analyzed using Pearson’s Chi square test or Fisher’s exact test where appropriate. Continuous variables with normal distributions are presented as means with standard deviations (± SD) and compared with the independent Student t test. Non-normally distributed continuous variables are presented as medians with interquartile ranges (IQRs) and compared using the Mann–Whitney U test.
A missing data category was introduced for each categorical variable with ≥ 2% missing data. Otherwise, patients with missing data for variables missing < 2% were excluded (arbitrary cut-off). If a categorical variable had < 2% missing data, the missing patients were not included in the overall proportions reported, and they were not included in the test of association. If a categorical variable had ≥ 2% missing, these patients were classified as missing and were included in the overall proportions and the test of association. For all continuous variables, the missing patients were not included in the test of association. This strategy was used for both the descriptive analyses and the logistic regression analyses.
Some variables of interest were not collected in all four registries during the study period (i.e., hospital volume, intraoperative blood loss, PPH, admission to the intensive care unit [ICU], and R status were not collected in the NSQIP), and were therefore categorized as ‘not available’; this category was not tested in the test of association, except for the logistic regression analyses when applicable.
Logistic regression analyses were performed to investigate the potential predictors for major morbidity and mortality, whereby the results are presented in odds ratios (ORs) with 95% confidence intervals (CIs). Independent variables with p < 0.050 in the univariable analysis were subsequently tested in the multivariable analysis. When an independent variable was significant based on only the ‘missing data’ category, this variable was not used in the selection either for or within the multivariable analysis. In the multivariable analysis, backward selection was used until the model only contained independent parameters that were statistically significant.
Results
A total of 9801 DPs were performed during the study period, of which 6877 patients (70.2%) were excluded because of a diagnosis other than pancreatic adenocarcinoma (n = 6177, 63.0%), had missing data regarding the diagnosis (n = 260, 2.7%), had missing data on whether a vascular resection was performed (n = 45, 0.5%), or underwent DP with concomitant arterial resection[s] (n = 168, 1.7%) or multivisceral resection[s] (n = 227, 2.3%).
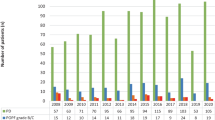
The final study cohort comprised 2924 patients, of whom 8.2% (n = 241) underwent a concomitant PVR. In North America, Germany, Sweden, and The Netherlands, the proportion of patients who underwent a concomitant PVR among the included patients was 9.2% (n = 199/2165), 5.9% (n = 27/461), 1.9% (n = 3/157), and 8.5% (n = 12/141), respectively (p = 0.002).
Baseline Characteristics
See Table 1 for the baseline characteristics. Patients undergoing DP-PVR were younger (mean 67 ± 10 years) in comparison with patients who underwent a standard DP (mean 69 ± 10; p = 0.004), were more likely to be female (n = 1342 [50.0%] vs. n = 143 [59.3%]; p < 0.006), and had a lower mean body mass index (27 ± 6 vs. 26 ± 6; p = 0.040). The performance status and the prevalence of cardiovascular and pulmonary comorbidities were similar between both groups. More patients undergoing DP-PVR were treated with preoperative chemotherapy than patients without PVR (n = 124 [51.5%] vs. n = 702 [26.2%]; p < 0.001).
Surgery Details and Surgical Outcome
Details regarding surgery and surgical outcomes are presented in Table 2. The rate of primary open surgery was higher in the DP-PVR group (n = 199, 82.6%) compared with the standard DP group (n = 1626, 60.7%) [p < 0.001]. Among the patients who underwent minimally invasive surgery, the conversion rate was higher in the DP-PVR group (n = 19/36, 52.8%) compared with the standard DP group (n = 212/875, 24.2%) [p < 0.001].
The rate of major morbidity was higher after DP-PVR versus standard DP (n = 57 [23.8%] vs. n = 479 [17.9%]; p = 0.024), without significant differences in the relaparotomy rate (n = 12 [5.0%] vs. n = 94 [3.5%]; p = 0.237) and ICU admission (n = 4 [9.8%] vs. n = 24 [3.4%]; p = 0.060). However, the rate of PPH grade B/C was higher after DP-PVR (n = 4, 9.8%) in comparison with standard DP (n = 21, 2.9%) [p = 0.041]. From those patients who developed PPH grade B/C, 75.0% (n = 3/4) of patients after DP-PVR and 47.6% (n = 10/21) after standard DP also had POPF grade B/C (p = 0.593). In the subgroup of patients who developed POPF grade B/C (with available data on PPH), the rate of PPH grade B/C was higher after DP-PVR compared with standard DP (n = 3/10 [30.0%] vs. n = 10/133 [7.5%]; p = 0.049). The median length of hospital stay was longer after DP-PVR (7 days [IQR 6–11]) compared with patients who underwent standard DP (6 days [IQR 5–10]) [p < 0.001].
The in-hospital/30-day mortality did not differ between DP-PVR and standard DP (n = 4 [1.7%] vs. n = 33 [1.2%]; p = 0.542). Mortality rates among patients undergoing primary open DP-PVR versus minimally invasive DP-PVR versus minimally invasive surgery requiring conversion to open were 2.0% (n = 4/199), 0% (n = 0/17), and 0% (n = 0/19) [p > 0.999], respectively. See Table 3 for the histopathological outcome.
Predictors for Major Morbidity and Mortality
See Table 4 for the logistic regression analysis for predictors of major morbidity. PVR was an independent predictor for major morbidity (OR 1.500, 95% CI 1.086–2.071). Minimally invasive surgery converted to open surgery was also associated with major morbidity (OR 1.420, 95% CI 1.023–1.970). On the other hand, preoperative chemotherapy was associated with a lower likelihood of developing major morbidity (OR 0.765, 95% CI 0.611–0.959). Moreover, the Swedish registry was associated with less major morbidity.
See Table 5 for the logistic regression analysis for predictors of 30-day/in-hospital mortality. PVR was not associated with mortality (OR 1.355, 95% CI 0.476–3.857). A higher age (OR 1.087, 95% CI 1.045–1.132), chronic obstructive pulmonary disease (OR 4.167, 95% CI 1.852–9.374), and minimally invasive surgery converted to open surgery (OR 2.919, 95% CI 1.197–7.118) were independent predictors for mortality. The different registries were not associated with mortality.
Discussion
To date, this largest observational international study in 2924 patients with pancreatic adenocarcinoma demonstrated that PVR during DP is associated with higher rates of in-hospital/30-day major morbidity (24% vs. 18%) and PPH grade B/C (10% vs. 3%), whereas it did not increase the in-hospital mortality/30-day major morbidity (1.7% vs. 1.2%). PVR was an independent predictor for developing major morbidity, but did not impact the mortality. In contrast, older age, chronic obstructive pulmonary disease, and conversion from minimally invasive to open surgery were associated with mortality. Nevertheless, no mortality occurred among patients who underwent DP-PVR after conversion from minimally invasive to open surgery.
Previously, two single-center, observational studies investigated the surgical outcome after DP-PVR versus standard DP.9,11 Loos et al. compared 79 patients after DP-PVR with 1383 patients who underwent standard DP for any indication, without concomitant arterial and/or multivisceral resection(s).11 Of note, the DP-PVR group was defined as either a concomitant PVR or left renal vein resection. Their univariable logistic regression analyses supported the findings from the current study that DP-PVR is associated with major morbidity but not with short-term mortality.11 However, no distinction was made between standard DP and DP-PVR in the multivariable analyses. Although Loos et al. did not perform direct statistical comparisons from DP-PVR versus standard DP, differences in surgical outcome between both procedures in that study seemed in line with our study: major morbidity (41% vs. 22%), PPH grade C (5% vs. 2%), and 90-day mortality (1% vs. 1%).11 A second single-center, observational study compared DP-PVR (n = 41) with standard DP (n = 82) without concomitant arterial resection(s), again performed for any indication.9 Both 90-day mortality (0% vs. 3%) and major morbidity (17% vs. 13%) did not differ significantly. However, the rate of PPH was significantly higher after DP-PVR (17% vs. 4%), as was also found in our study.9
Among patients who developed POPF grade B/C in this study, the rate of PPH grade B/C was higher after DP-PVR compared with standard DP (30% vs. 8%), but no information was available on the timing and cause of PPH. Unfortunately, only two of four registries/audits collected data on both PPH and intraoperative drain management, leaving too few patients to sufficiently investigate patterns in drain management between DP-PVR and standard DP. No difference in the rate of PPH grade B/C was observed in the international PANDORINA trial wherein 282 patients who underwent a DP were randomized between drain versus no drain placement.39 Since the detection of POPF grade B/C was lower in the no drain group, drain placement during DP-PVR might detect POPF in an earlier stage, hypothetically reducing the risk for PPH grade B/C from the reconstructed vein.40 Another potential cause of PPH is the use (and type) of thromboprophylaxis,41,42 but no data on the use of anti-coagulance were available—an important understudied topic with variances in local protocols.42
The findings from both single-center series9,11 suggest that, in particular, the increased risk for PPH after DP-PVR contributes to the higher major morbidity. The lack of significance in the current study from the differences in ICU admission and relaparotomy rates suggests that the complications related to PVR can mostly be managed with minimally invasive interventions (i.e., Clavien–Dindo grade IIIa34). In contrast, the results from the Heidelberg series suggested that the rates of relaparotomy and ICU admission are higher after PD-PVR compared with standard DP, although this observation could also be related to the higher rates of POPF after DP-PVR compared with standard DP (33% vs. 20%).11
The technical challenge of a DP-PVR is the limited mobilization of the portomesenteric venous axis, in contrast to a PD or TP due to removal of the pancreatic head and the Kocher and Cattell–Braasch maneuvers.43 As a consequence, a DP-PVR for a pancreatic body tumor is mostly only performed in the presence of limited left-sided venous involvement. Segmental venous resections are performed in 22–56% of the DP-PVRs.9,14,18,19 Hypothetically, the limited capability to mobilize the portomesenteric veins increases the risk for narrowing of the venous reconstruction and thus the risk for early portomesenteric venous thrombosis.12 Other known risk factors for thrombosis are the use of synthetic grafts for the venous reconstruction and performing a segmental venous resection.14,44,45 Three studies reported on the incidence of thrombosis after DP-PVR.12,17,46 A single-center experience from Roch et al. revealed that 4 of 14 patients (29%) developed portomesenteric venous thrombosis after DP-PVR for any indication.17 Another single-center study reported a 7% incidence of portomesenteric venous thrombosis among 15 patients who underwent DP-PVR for a locally advanced pancreatic neuroendocrine tumor,46 while a third single-center study described high rates of occlusion (22%) and > 50% narrowing (28%) among 32 patients who underwent a DP-PVR for pancreatic adenocarcinoma.12 Based on these findings, Maekawa et al. proposed to perform a PD-PVR instead of DP-PVR if the length of venous involvement is ≥ 30 mm.12 Unfortunately, information regarding the incidence of thrombosis was not available in the four registries used for the present study.
The results from the current study suggest that DP-PVR is associated with a significant but limited increased risk for major morbidity without an increase in short-term mortality in comparison with a standard DP. Therefore, DP-PVR seems to be a reasonably safe and feasible procedure in patients with pancreatic adenocarcinoma located in the pancreatic body, with limited portomesenteric venous involvement when performed by experienced surgeons. Importantly, the seemingly limited additional risks of DP-PVR over standard DP could be related to more high-volume surgeons/centers performing these procedures. However, this remains speculative because volume data are not available within the NSQIP. Nevertheless, this limited risk elevation seems to outbalance the risks and long-term sequalae from alternative procedures (i.e., extended PD-PVR or TP-PVR). Established benchmarks for major morbidity (≤ 28%) and in-hospital mortality (≤ 4%) after PD-PVR performed in a high-volume center are higher than the outcomes after DP-PVR in our study.6 Another option is a TP-PVR, which is associated with similar surgical outcomes as the benchmarks for PD-PVR when performed in high-volume centers.47,48 However, TP should be avoided when possible considering the associated endocrine and exocrine insufficiencies.22 Furthermore, TP-PVR is associated with gastric venous congestion, particularly when combined with left gastric vein ligation.49 Of note, it might also be needed to sacrifice the left gastric vein as part of DP-PVR, after which the gastric venous drainage depends on the right gastric vein, right gastroepiploic vein, and distal esophageal veins, which might be associated with gastric venous congestion. Eventually, the left gastric vein could be reconstructed.50 Since the extent of tumor involvement with the portomesenteric venous axis was not available in the currently used registries, it is possible that an extended PD or TP is a more safe and feasible procedure in the case of more extensive venous involvement, depending on the surgeon’s preference.
Over the last decade, the use of minimally invasive DP for benign and (pre-)malignant pancreatic diseases has increased.51 It is likely this trend will continue based on the results from the DIPLOMA trial, which demonstrated the non-inferiority of minimally invasive DP over open DP in patients with resectable pancreatic adenocarcinoma.52 The present observational study showed that conversion from minimally invasive to open surgery is independently associated with both in-hospital/30-day major morbidity and mortality. As vascular involvement is known to be the main indication to convert, caution is required for adenocarcinomas located in the pancreatic body with proximity to the portomesenteric venous axis.53 Unfortunately, the reasons for conversion to open surgery (e.g., unexpected vascular involvement, intraoperative bleeding) are not registered in the four audits/registries. It would seem prudent to use recent imaging when embarking on a minimally invasive DP with potential vascular involvement. The DIPLOMA trial required computed tomography at a maximum of 4 weeks before surgery.48
The present study showed that preoperative chemo(radio)therapy was associated with lower odds of developing major morbidity. This might be related to a lower rate of POPF as a consequence of radiotherapy, however data regarding treatment with preoperative radiotherapy were not available in all four registries.54
The results from this study should be seen in the light of several limitations. First, no data were available regarding either the extent of venous involvement or the type of PVR, which was why no proper comparison could be made with the GAPASURG data to compare DP-PVR with either TP-PVR or PD-PVR. Both PD and TP procedures can be performed for a wide spectrum of indications and with various concomitant procedures, associated with different levels of complexity and outcomes.47,48,55 Second, only ISPGS type 2–4 resections were registered as PVR in the NSQIP registry, which might have influenced the surgical outcome in this study. Third, no data were available regarding anti-coagulance therapy, short- and long-term patency of the venous reconstruction, timing and origin of PPH, and detailed data on perioperative oncological treatments and survival. Fourth, the rule of thumb for the logistic regression analysis on predictors for mortality was more or less violated, testing one more dependent variable than allowed, considering the number of events. Fifth, even though all patients who underwent an arterial resection were excluded, a minority of patients was classified as having (y)pT4, most likely due to a misclassification by the pathologist. Sixth, the small numbers of patients who underwent DP-PVR in Germany, The Netherlands, and Sweden did not allow comparative analyses between DP-PVR and standard DP for each of the four registries separately; therefore, the results could have been influenced by (potential) differences in clinical practices among countries (e.g., regarding patient selection, length of hospital stay) and the structure from the registries. Important differences between the registries were (1) voluntary and multicenter registries (North America and Germany) versus mandatory and national registries (Sweden and The Netherlands); (2) auditing strategies; and (3) length of follow-up. These variances might explain why the registry was associated with major morbidity. The current study tried to correct for these potential influences by testing the association of the four registries in the logistic regression analyses. Seventh, no data on adjuvant therapy and survival are collected in the four audits/registries, whereby it was not possible to assess the impact of complications on the receipt of adjuvant chemotherapy and overall survival.
Nevertheless, the major strength of this study is that this relates to the first multicenter study that compared the surgical outcome after DP-PVR versus standard DP, providing valuable evidence regarding the surgical risks of DP-PVR in a large international cohort. These new insights can guide surgeons in preoperative and intraoperative decision making. Future studies should focus on the comparison of DP-PVR with either extended PD-PVR or TP-PVR, hereby taking into account the extent of venous involvement and the type of PVR, and investigating the surgical outcome, including the short- and long-term venous patency as well as the long-term oncological outcome.
Conclusion
Pancreatic adenocarcinoma located in the pancreatic body with portomesenteric venous involvement can be safely managed with DP-PVR, considering the elevated but limited risk for additional major morbidity (24% vs. 18%) compared with standard DP without additional risk for mortality (1.7% vs. 1.2%).
References
Park W, Chawla A, O’Reilly EM. Pancreatic cancer: a review. JAMA. 2021;326(9):851–62. https://doi.org/10.1001/jama.2021.13027.
Tempero MA, Malafa MP, Al-Hawary M, et al. Pancreatic adenocarcinoma, version 1.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2021;19(4):439–57. https://doi.org/10.6004/jnccn.2021.0017.
Bockhorn M, Uzunoglu FG, Adham M, et al. Borderline resectable pancreatic cancer: a consensus statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2014;155(6):977–88. https://doi.org/10.1016/j.surg.2014.02.001.
Machairas N, Raptis DA, Sánchez-Velázquez P, et al. The impact of neoadjuvant treatment on survival in patients undergoing pancreatoduodenectomy with concomitant portomesenteric venous resection: an international multicenter analysis. Ann Surg. 2021;274(5):721–8. https://doi.org/10.1097/SLA.0000000000005132.
van Erning FN, Mackay TM, van der Geest LGM, et al. Association of the location of pancreatic ductal adenocarcinoma (head, body, tail) with tumor stage, treatment, and survival: a population-based analysis. Acta Oncol. 2018;57(12):1655–62. https://doi.org/10.1080/0284186X.2018.1518593.
Raptis DA, Sanchez-Velásquez P, Machairas N, et al. Defining benchmark outcomes for pancreaticoduodenectomy with concomitant portomesenteric venous resection. Ann Surg. 2020;272(5):731–7. https://doi.org/10.1097/SLA.0000000000004267.
Beane JD, House MG, Pitt SC, et al. Pancreatoduodenectomy with venous or arterial resection: a NSQIP propensity score analysis. HPB (Oxford). 2017;19(3):254–63. https://doi.org/10.1016/j.hpb.2016.11.013.
Zwart ES, Yilmaz BS, Halimi A, et al. Venous resection for pancreatic cancer, a safe and feasible option? A systematic review and meta-analysis. Pancreatology. 2022;22(6):803–9. https://doi.org/10.1016/j.pan.2022.05.001.
Xu D, Wu P, Zhang K, et al. The short-term outcomes of distal pancreatectomy with portal vein/superior mesenteric vein resection. Langenbecks Arch Surg. 2022;407(5):2161–8. https://doi.org/10.1007/s00423-021-02382-8.
Yamamoto Y, Sugiura T, Okamura Y, et al. Prognostic analysis of distal pancreatectomy for pancreatic body and/or tail cancer involving the portal vein: Is pancreatic body and/or tail cancer involving the portal vein resectable? Pancreas. 2022;51(5):502–9. https://doi.org/10.1097/MPA.0000000000002058.
Loos M, Mack CE, Xu ATL, et al. Distal pancreatectomy: extent of resection determines surgical risk categories. Ann Surg. 2024;279(3):479–85. https://doi.org/10.1097/SLA.0000000000005935.
Maekawa A, Oba A, Inoue Y, et al. Technical strategy for pancreatic body cancers: a raison d’etre of distal pancreatectomy with portal resection. Ann Surg Oncol. 2024;31(2):1347–57. https://doi.org/10.1245/s10434-023-14554-5.
Ramacciato G, Nigri G, Petrucciani N, et al. Pancreatectomy with mesenteric and portal vein resection for borderline resectable pancreatic cancer: multicenter study of 406 patients. Ann Surg Oncol. 2016;23(6):2028–37. https://doi.org/10.1245/s10434-016-5123-5.
Hackert T, Klaiber U, Hinz U, et al. Portal vein resection in pancreatic cancer surgery: risk of thrombosis and radicality determine survival. Ann Surg. 2022;277(6):e1291–8. https://doi.org/10.1097/SLA.0000000000005444.
Bultmann U, Niedergethmann M, Gelos M. Postoperative results, pathologic outcome, and long-term patency rate of autologous vein reconstruction of the mesentericoportal axis after pancreatectomy. Langenbecks Arch Surg. 2021;406(5):1453–60. https://doi.org/10.1007/s00423-020-02026-3.
Sutton TL, Sandoval V, Warner D, et al. Patency for autologous vein is superior to cadaveric vein in portal-mesenteric venous reconstruction. HPB (Oxford). 2022;24(8):1326–34. https://doi.org/10.1016/j.hpb.2022.01.004.
Roch AM, Kilbane EM, Nguyen T, et al. Portal vein thrombosis after venous reconstruction during pancreatectomy: timing and risks. J Gastrointest Surg. 2022;26(10):2148–57. https://doi.org/10.1007/s11605-022-05401-1.
Tamburrino D, Belfiori G, Andreasi V, et al. Pancreatectomy with venous vascular resection for pancreatic cancer: impact of types of vein resection on timing and pattern of recurrence. Eur J Surg Oncol. 2023;49(8):1457–65. https://doi.org/10.1016/j.ejso.2023.03.229.
Vuorela T, Vikatmaa P, Kokkola A, et al. Long term results of pancreatectomy with and without venous resection: a comparison of safety and complications of spiral graft, end-to-end and tangential/patch reconstruction techniques. Eur J Vasc Endovasc Surg. 2022;64(2–3):244–53. https://doi.org/10.1016/j.ejvs.2022.04.006.
Sillesen M, Hansen CP, Dencker EE, et al. Long-term outcomes of venous resections in pancreatic ductal adenocarcinoma patients: a nationwide cohort study. Ann Surg Open. 2022;3(4):e219. https://doi.org/10.1097/AS9.0000000000000219
Scholten L, Stoop TF, Del Chiaro M, et al. Systematic review of functional outcome and quality of life after total pancreatectomy. Br J Surg. 2019;106(13):1735–46. https://doi.org/10.1002/bjs.11296.
Stoop TF, Ateeb Z, Ghorbani P, et al. Impact of endocrine and exocrine insufficiency on quality of life after total pancreatectomy. Ann Surg Oncol. 2020;27(2):587–96. https://doi.org/10.1245/s10434-019-07853-3.
Stoop TF, Bergquist E, Theijse RT, et al. Systematic review and meta-analysis of the role of total pancreatectomy as an alternative to pancreatoduodenectomy in patients at high risk for postoperative pancreatic fistula: Is it a justifiable indication? Ann Surg. 2023;278(4):e702–11. https://doi.org/10.1097/SLA.0000000000005895.
Sanchez-Velazquez P, Muller X, Malleo G, et al. Benchmarks in pancreatic surgery: a novel tool for unbiased outcome comparisons. Ann Surg. 2019;270(2):211–8. https://doi.org/10.1097/SLA.0000000000003223.
Durin T, Marchese U, Sauvanet A, et al. Defining benchmark outcomes for distal pancreatectomy: results of a French multicentric study. Ann Surg. 2023;278(1):103–9. https://doi.org/10.1097/SLA.0000000000005539.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008.
Mackay TM, Gleeson EM, Wellner UF, et al. Transatlantic registries of pancreatic surgery in the United States of America, Germany, the Netherlands, and Sweden: comparing design, variables, patients, treatment strategies, and outcomes. Surgery. 2021;169(2):396–402. https://doi.org/10.1016/j.surg.2020.07.012.
Petrucciani N, Debs T, Nigri G, et al. Pancreatectomy combined with multivisceral resection for pancreatic malignancies: Is it justified? Results of a systematic review. HPB (Oxford). 2018;20(1):3–10. https://doi.org/10.1016/j.hpb.2017.08.002.
Nigri G, Petrucciani N, Belloni E, et al. Distal pancreatectomy with celiac axis resection: systematic review and meta-analysis. Cancers (Basel). 2021;13(8):1967. https://doi.org/10.3390/cancers13081967.
Wellner UF, Klinger C, Lehmann K, Buhr H, Neugebauer E, Keck T. The pancreatic surgery registry (StuDoQ|Pancreas) of the German Society for general and visceral surgery (DGAV)—presentation and systematic quality evaluation. Trials. 2017;18(1):163. https://doi.org/10.1186/s13063-017-1911-x.
Tingstedt B, Andersson B, Jonsson C, et al. First results from the Swedish National Pancreatic and Periampullary Cancer Registry. HPB (Oxford). 2019;21(1):34–42. https://doi.org/10.1016/j.hpb.2018.06.1811.
van Rijssen LB, Groot Koerkamp B, Zwart MJ, et al. Nationwide prospective audit of pancreatic surgery: design, accuracy, and outcomes of the Dutch Pancreatic Cancer Audit. HPB (Oxford). 2017;19(10):919–26. https://doi.org/10.1016/j.hpb.2017/06.010.
van der Geest LG, van Rijssen LB, Molenaar IQ, et al. Volume-outcome relationships in pancreatoduodenectomy for cancer. HPB (Oxford). 2016;18(4):317–24. https://doi.org/10.1016/j.hpb.2016.01.515.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Bassi C, Marchegiani G, Dervenis C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017;161(3):584–91. https://doi.org/10.1016/j.surg.2016.11.014.
Wente MN, Bassi C, Dervenis C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142(5):761–8. https://doi.org/10.1016/j.surg.2007.05.005.
Wente MN, Veit JA, Bassi C, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142(1):20–5. https://doi.org/10.1016/j.surg.2007.02.001.
Campbell F, Foulis A, Verbeke C. Dataset for the histopathological reporting of carcinomas of the pancreas, ampulla of Vater and common bile duct. R Coll Pathol. 2010;7:1–70.
van Bodegraven EA, Balduzzi A, van Ramshorst TME, et al. Prophylactic abdominal drainage after distal pancreatectomy (PANDORINA): an international, multicentre, open-label, randomised controlled, non-inferiority trial. Lancet Gastroenterol Hepatol. 2024;9(5):438–47. https://doi.org/10.1016/S2468-1253(24)00037-2.
Smits FJ, Henry AC, Besselink MG, et al. Algorithm-based care versus usual care for the Arly recognition and management of complications after pancreatic resection in the Netherlands: an open-label, nationwide, stepped-wedge cluster-randomised trial. Lancet. 2022;399(10338):1867–75. https://doi.org/10.1016/S0140-6736(22)00182-9.
Lavikainen LI, Guyatt GH, Sallinen VJ, et al. Systematic reviews and meta-analyses of the procedure-specific risks of thrombosis and bleeding in general abdominal, colorectal, upper gastrointestinal, and hepatopancreatobiliary surgery. Ann Surg. 2024;279(2):213–25. https://doi.org/10.1097/SLA.0000000000006059.
Clancy TE, Baker EH, Maegawa FA, et al. AHPBA guidelines for managing VTE prophylaxis and anticoagulation for pancreatic surgery. HPB (Oxford). 2022;24(5):575–85. https://doi.org/10.1016/j.hpb.2021.12.010.
Del Chiaro M, Segersvard R, Rangelova E, et al. Cattell-Braasch maneuver combined with artery-first approach for superior mesenteric-portal vein resection during pancreatectomy. J Gastrointest Surg. 2015;19(12):2264–8. https://doi.org/10.1007/s11605-015-2958-1.
Groen JV, Michiels N, van Roessel S, et al. Venous wedge and segment resection during pancreatoduodenectomy for pancreatic cancer: impact on short- and long-term outcomes in a nationwide cohort analysis. Br J Surg. 2021;109(1):96–104. https://doi.org/10.1093/bjs/znab345
Labori KJ, Kleive D, Khan A, Farnes I, Fosby B, Line PD. Graft type for superior mesenteric and portal vein reconstruction in pancreatic surgery: a systematic review. HPB (Oxford). 2021;23(4):483–94. https://doi.org/10.1016/j.hpb.2020.11.008.
Gudmundsdottir H, Tomlinson JL, Graham RP, et al. Outcomes of pancreatectomy with portomesenteric venous resection and reconstruction for locally advanced pancreatic neuroendocrine neoplasms. HPB (Oxford). 2022;24(7):1186–93. https://doi.org/10.1016/j.hpb.2021.12.016.
Stoop TF, Ateeb Z, Ghorbani P, et al. Surgical outcomes after total pancreatectomy: a high-volume center experience. Ann Surg Oncol. 2021;28(3):1543–51. https://doi.org/10.1245/s10434-020-08957-x
Loos M, Al-Saeedi M, Hinz U, et al. Categorization of different types of total pancreatectomy. JAMA Surg. 2022;157(2):120–8. https://doi.org/10.1001/jamasurg.2021.5834.
Stoop TF, Von Gohren A, Engstrand J, et al. Risk factors, management, and outcome of gastric venous congestion after total pancreatectomy: an underestimated complication requiring standardized identification, grading, and management. Ann Surg Oncol. 2023;30(12):7700–11. https://doi.org/10.1245/s10434-023-13847-z.
Hackert T, Weitz J, Büchler MW. Reinsertion of the gastric coronary vein to avoid venous gastric congestion in pancreatic surgery. HPB (Oxford). 2015;17(4):368–70. https://doi.org/10.1111/hpb.12321.
van Ramshorst TME, van Hilst J, Bannone E, et al. International survey on opinions and use of robot-assisted and laparoscopic minimally invasive pancreatic surgery: 5-year follow up. HPB (Oxford). 2024;26(1):63–72. https://doi.org/10.1016/j.hpb.2023.09.004.
Korrel M, Jones LR, van Hilst J, et al. Minimally invasive versus open distal pancreatectomy for resectable pancreatic cancer (DIPLOMA): an international randomised non-inferiority trial. Lancet Reg Health Eur. 2023;31:100673. https://doi.org/10.1016/j.lanepe.2023.100673.
Balduzzi A, van der Heijde N, Alseidi A, et al. Risk factors and outcomes of conversion in minimally invasive distal pancreatectomy: a systematic review. Langenbecks Arch Surg. 2021;406(3):597–605. https://doi.org/10.1007/s00423-020-02043-2.
Wismans LV, Suurmeijer JA, van Dongen JC, et al. Preoperative chemoradiotherapy but not chemotherapy is associated with reduced risk of postoperative pancreatic fistula after pancreatoduodenectomy for pancreatic ductal adenocarcinoma: a nationwide analysis. Surgery. 2024;175(6):1580–6. https://doi.org/10.1016/j.surg.2024.01.029.
Mihaljevic AL, Hackert T, Loos M, et al. Not all Whipple procedures are equal: proposal for a classification of pancreatoduodenectomies. Surgery. 2021;169(6):1456–62. https://doi.org/10.1016/j.surg.2020.11.030.
Acknowledgment
Collaborators for the Global Audits on Pancreatic Surgery Group (GAPASURG): Tara M. Mackay, MD, PhD2,3; Salvador Rodriguez Franco, MD1; Susan van Dieren, MSc, PhD2.
Funding
Thomas F. Stoop has received grants from the Dutch Cancer Society (KWF) and Deltaplan Alvleesklierkanker for the Dutch PREOPANC-4 trial on multidisciplinary management of locally advanced pancreatic cancer (NCT05524090), and from the Cultuurfonds (Jan de Ruijsscher/Pia Huisman Fonds) and Cancer Center Amsterdam.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Disclosure
Marco Del Chiaro has been awarded an industry grant (Haemonetics, Inc.) to conduct a multicenter study to evaluate the prognostic implications of TEG in pancreatic cancer. He is co-principal investigator of a Boston Scientific-sponsored international multicenter study on the use of intraoperative pancreatoscopy of patients with intraductal papillary mucinous neoplasms (IPMN). Simone Augustinus, Bergthor Björnsson, Bobby Tingstedt, Bodil Andersson, Christopher L. Wolfgang, Jens Werner, Karin Johansen, Martijn W.J. Stommel, Matthew H.G. Katz, Michael Ghadimi, Michael G. House, Poya Ghorbani, I. Quintus Molenaar, Roeland F. de Wilde, J. Sven D. Mieog, Tobias Keck, Ulrich F. Wellner, Waldemar Uhl, Marc G. Besselink, and Henry A. Pitt have no conflicts of interest to declare that may be relevant to the contents of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1. Major differences in registry designs
Appendix 1. Major differences in registry designs
North America | Germany | Sweden | The Netherlands | |
|---|---|---|---|---|
Design | Multicenter | Multicenter | Nationwide | Nationwide |
Participation | Voluntary | Voluntary | Mandatory | Mandatory |
Auditing | No auditing, but data entry by independent reviewersa | Yearly auditing | Auditing each third year | Auditing performed once (2017) |
Portomesenteric venous resection | Only ISGPS types 2–4 are registered | ISGPS types 1–4 are registered | ISGPS types 1–4 are registered | ISGPS types 1–4 are registered |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stoop, T.F., Augustinus, S., Björnsson, B. et al. Surgical Outcome After Distal Pancreatectomy With and Without Portomesenteric Venous Resection in Patients with Pancreatic Adenocarcinoma: A Transatlantic Evaluation of Patients in North America, Germany, Sweden, and The Netherlands (GAPASURG). Ann Surg Oncol (2024). https://doi.org/10.1245/s10434-024-15932-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1245/s10434-024-15932-3