Abstract
Background
Performance of complex cancer surgeries at high-volume (HV) centers has been shown to reduce operative mortality. However, the case volume threshold that should be used to define HV centers is unknown. In this study, we determined thresholds to define HV pancreaticoduodenectomy, esophagectomy, and major lung resection centers based on clinical parameters. Then, we assessed the association of hospital volume with oncologic outcomes and overall survival.
Methods
We identified adult NCDB patients undergoing pancreaticoduodenectomy, esophagectomy, and major lung resections between 2004 and 2015. Multivariable models with restricted cubic splines were built to predict 5-year overall survival for each surgery group according to average yearly case volume, adjusting for demographic and clinicopathologic factors. The change point procedure was then used to identify volume cut-points for each surgery type.
Results
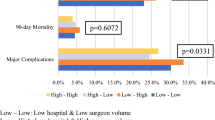
We identified the following thresholds to define HV status: 25 cases/year for pancreaticoduodenectomy; 18 cases/year for esophagectomy; and 54 cases/year for major lung resections. For all surgery types, treatment at a HV center was associated with an increased likelihood of R0 resection and adequate lymph node evaluation. HV centers had significantly decreased 30- and 90-day, postoperative mortality after adjusting for age, sex, race, comorbidities, histology, and stage. An overall survival benefit also was observed for patients undergoing resections at HV centers.
Conclusions
Using novel methodology, our study identified volume thresholds for HV pancreaticoduodenectomy, esophagectomy, and major lung resection centers that were associated with improved oncologic outcomes and overall survival. These definitions of HV centers should be considered when evaluating regionalization of complex cancer care.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–37.
Diaz A, Pawlik TM. Optimal location for centralization of hospitals performing pancreas resection in California. JAMA Surg. 2020;155(3):261.
Stitzenberg KB, Sigurdson ER, Egleston BL, Starkey RB, Meropol NJ, et al. Centralization of cancer surgery: implications for patient access to optimal care. J Clin Oncol. 2009;27(28):4671–8.
Ho V, Heslin MJ. Effect of hospital volume and experience on in-hospital mortality for pancreaticoduodenectomy. Ann Surg. 2003;237(4):509.
Hannan EL, Radzyner M, Rubin D, Dougherty J, Brennan MF, et al. The influence of hospital and surgeon volume on in-hospital mortality for colectomy, gastrectomy, and lung lobectomy in patients with cancer. Surgery. 2002;131(1):6–15.
Finlayson EVA. Hospital volume and operative mortality in cancer surgery. Arch Surg. 2003;138(7):721.
Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49(12):1076–81.
National Cancer Database. Cited 11 April 2022. https://www.facs.org/quality-programs/cancer/ncdb.
Ajani JA, D’Amico TA, Bentrem DJ, Chao J, Corvera C, Das P, et al. Esophageal and esophagogastric junction cancers, Version 2.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Netw. 2019;17(7):855–83.
Schwarz RE, Smith DD. Extent of lymph node retrieval and pancreatic cancer survival: information from a large US population database. Ann Surg Oncol. 2006;13(9):1189–200.
Tomlinson JS. Accuracy of staging node-negative pancreas cancer. Arch Surg. 2007;142(8):767.
David EA, Cooke DT, Chen Y, Nijar K, Canter RJ, Cress RD, et al. Does lymph node count influence survival in surgically resected non-small cell lung cancer? Ann Thorac Surg. 2017;103(1):226–35.
Harrell Jr F. rms: Regression Modeling Strategies. 2021.
Harrell FE. Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis, Vol. 3. Springer; 2015.
Van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67.
Plummer, M. JAGS: A program for analysis of Bayesian graphical models using Gibbs sampling. In: Proceedings of the 3rd international workshop on distributed statistical computing. 2003. Vienna, Austria.
Lindeløv JK. mcp: An R package for regression with multiple change points. 2020.
Hata T, Motoi F, Ishida M, Naitoh T, Katayose Y, Egawa S, et al. Effect of hospital volume on surgical outcomes after pancreaticoduodenectomy. Ann Surg. 2016;263(4):664–72.
Dimick JB, Pronovost PJ, Cowan JA, Lipsett PA, et al. Surgical volume and quality of care for esophageal resection: do high-volume hospitals have fewer complications? Ann Thorac Surg. 2003;75(2):337–41.
Macedo FIB, Jayanthi P, Mowzoon M, Yakoub D, Dudeja V, Merchant N, et al. The impact of surgeon volume on outcomes after pancreaticoduodenectomy: a meta-analysis. J Gastrointest Surg. 2017;21(10):1723–31.
Nakata K, Yamamoto H, Miyata H, Kakeji Y, Seto Y, Yamaue H, et al. Definition of the objective threshold of pancreatoduodenectomy with nationwide data systems. J Hepato-Biliary-Pancreatic Sci. 2020;27(3):107–13.
Lavu H, McCall NS, Winter JM, Burkhart RA, Pucci M, Leiby BE, et al. Enhancing patient outcomes while containing costs after complex abdominal operation: a randomized controlled trial of the Whipple accelerated recovery pathway. J Am Coll Surg. 2019;228(4):415–24.
Gordon TA, Bowman HM, Tielsch JM, Bass EB, Burleyson GP, Cameron JL, et al. Statewide regionalization of pancreaticoduodenectomy and its effect on in-hospital mortality. Ann Surg. 1998;228(1):71.
de Wilde RF, Besselink MGH, van der Tweel I, de Hingh IHJT, van Eijck CHJ, Dejong CHC, et al. Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. Br J Surg. 2012;99(3):404–10.
O’Mahoney PR, Yeo HL, Sedrakyan A, Trencheva K, Mao J, Isaacs AJ, et al. Centralization of pancreatoduodenectomy a decade later: impact of the volume–outcome relationship. Surgery. 2016;159(6):1528–38.
Ely S, Alabaster A, Ashiku SK, Patel A, Velotta JB, et al. Regionalization of thoracic surgery improves short-term cancer esophagectomy outcomes. J Thorac Dis. 2019;11(5):1867–78.
Sheetz KH, Dimick JB, Nathan H. Centralization of high-risk cancer surgery within existing hospital systems. J Clin Oncol. 2019;37(34):3234–42.
Leapfrog Hospital Survey. Factsheet: Inpatient Surgery. 2020.
Funding
JDK was supported by a Physician-Scientist Institutional Award from the Burroughs Wellcome Fund (award No. 1018897).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None of the authors have conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ju, M.R., Karalis, J.D., Leonard, G. et al. Defining Volume Targets for Regionalization of Pancreaticoduodenectomy, Esophagectomy, and Major Lung Resection Centers to Improve Oncologic and Surgical Outcomes. Ann Surg Oncol 31, 499–513 (2024). https://doi.org/10.1245/s10434-023-14339-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14339-w