Abstract
Background
Identification of risk factors facilitates the prevention of breast cancer-related lymphedema (BCRL). Several published systematic reviews have already addressed the risk factors for BCRL. This study aimed to systematically identify potential risk factors for BCRL and evaluate the quality of evidence.
Methods
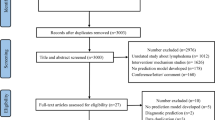
The study followed methodologic guidance from the Joanna Briggs Institute, and the Cochrane Handbook. The following electronic databases were systematically searched from inception to 15 November 2022: PubMed, Embase, CINAHL, Web of Science, Scopus, CNKI, SinoMed, Wanfang, JBI Database, Cochrane Database, ProQuest, and PROSPERO. Two authors independently screened studies, extracted data, and assessed methodologic quality using AMSTAR2, risk of bias using ROBIS, and evidence quality using GRADE. The study evaluated overlap, assessed the small-study effect, and calculated the I2 statistic and Egger’s P value as needed.
Results
The study included 14 publications comprising 10 meta-analyses and 4 systematic reviews. The authors identified 39 factors and 30 unique meta-analyses. In the study, 13 innate personal trait-related risk factors, such as higher body mass index (BMI) and axillary lymph nodes dissection, showed statistically significant associations with BCRL incidence. Breast reconstruction was found to be a protective factor. The methodologic quality was low or critically low. The majority of the systematic reviews and/or meta-analyses were rated as having a high risk of bias. Evidence quality was low for 22 associations and moderate for 8 associations.
Conclusions
The currently identified risk factors for BCRL all are innate personal trait-related factors. Future well-designed studies and robust meta-analyses are needed to explore potential associations between behavioral-, interpersonal-, and environmental-related factors and BCRL, as well as the role of genetic variations and pathophysiologic factors.


Similar content being viewed by others
References
Shen A, Lu Q, Fu X, et al. Risk factors of unilateral breast cancer-related lymphedema: an updated systematic review and meta-analysis of 84 cohort studies. Support Care Cancer. 2022;31:18.
Pappalardo M, Starnoni M, Franceschini G, Baccarani A, De Santis G. Breast cancer-related lymphedema: recent updates on diagnosis, severity, and available treatments. J Pers Med. 2021;11:402.
McLaughlin SA, Brunelle CL, Taghian A. Breast cancer-related lymphedema: risk factors, screening, management, and the impact of locoregional treatment. J Clin Oncol. 2020;38:2341–50.
Rockson SG. Lymphedema after breast cancer treatment. N Engl J Med. 2019;380:694.
Tandra P, Kallam A, Krishnamurthy J. Identification and management of lymphedema in patients with breast cancer. J Oncol Pract. 2019;15:255–62.
Gillespie TC, Sayegh HE, Brunelle CL, Daniell KM, Taghian AG. Breast cancer-related lymphedema: risk factors, precautionary measures, and treatments. Gland Surg. 2018;7:379–403.
Offord DR, Kraemer HC. Risk factors and prevention. Evid Based Ment Health. 2000;3:70–1.
He L, Qu H, Wu Q, Song Y. Lymphedema in survivors of breast cancer. Oncol Lett. 2020;19:2085–96.
Brown S, Dayan JH, Kataru RP, Mehrara BJ. The vicious circle of stasis, inflammation, and fibrosis in lymphedema. Plast Reconstr Surg. 2023;151:330e-e341.
Kapellas N, Demiri E, Lampropoulos A, Dionyssiou D. Genetic predisposition in cancer-related lymphedema: a systematic review. Lymph Res Biol. 2022;20:478–87.
Zhu YQ, Xie YH, Liu FH, et al. Systemic analysis on risk factors for breast cancer-related lymphedema. APJCP Asian Pac J Cancer Prev. 2014;15:6535–41.
Lin Y, Xu Y, Wang C, et al. Loco-regional therapy and the risk of breast cancer-related lymphedema: a systematic review and meta-analysis. Breast Cancer. 2021;28:1261–72.
Guliyeva G, Huayllani MT, Boczar D, et al. Age as a risk factor for breast cancer-related lymphedema: a systematic review. J Cancer Surviv. 2021;17(1):246.
Guliyeva G, Huayllani MT, Boczar D, Avila FR, Forte AJ. Correlation of older age with severity of lymphedema in breast cancer survivors: a systematic review. Breast Dis. 2021;40:191–7.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Aromataris E, Munn Z. JBI Manual for Evidence Synthesis. JBI; 2020.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2nd Ed. Chichester, UK: John Wiley & Sons; 2019.
Aromataris E, Fernandez R, Godfrey CM, et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13:132–40.
Shen A, Lu Q, Zhang L, et al. Risk factors of breast cancer-related lymphoedema: protocol of an umbrella review. BMJ Open. 2023;13:e070907.
Morgan RL, Whaley P, Thayer KA, Schunemann HJ. Identifying the PECO: a framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ Int. 2018;121(Pt 1):1027–31.
Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Whiting P, Savovic J, Higgins JP, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–6.
Pieper D, Antoine SL, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67:368–75.
Belbasis L, Bellou V, Evangelou E, Ioannidis JP, Tzoulaki I. Environmental risk factors and multiple sclerosis: an umbrella review of systematic reviews and meta-analyses. Lancet Neurol. 2015;14:263–73.
Che Bakri NA, Kwasnicki RM, Khan N, et al. Impact of axillary lymph node dissection and sentinel lymph node biopsy on upper limb morbidity in breast cancer patients: a systematic review and meta-analysis. Ann Surg. 2022;277:572.
Disipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14:1077–4114 ((print)(6): 500–515).
Kanda MH, da Costa Vieira RA, Lima JPSN, Paiva CE, Cunha de Araujo RL. Late locoregional complications associated with adjuvant radiotherapy in the treatment of breast cancer: systematic review and meta-analysis. J Surg Oncol. 2020;121:766–76.
Manirakiza A, Irakoze L, Shui L, Manirakiza S, Ngendahayo L. Lymphoedema after breast cancer treatment is associated with higher body mass index: a systematic review and meta-analysis. East Afr Health Res J. 2019;3:178–92.
Siotos C, Sebai ME, Wan EL, et al. Breast reconstruction and risk of arm lymphedema development: a meta-analysis. J Plast Reconstr Aesth Surg. 2018;71:807–18.
Torgbenu E, Luckett T, Buhagiar MA, Chang S, Phillips JL. Prevalence and incidence of cancer-related lymphedema in low and middle-income countries: a systematic review and meta-analysis. BMC Cancer. 2020;20:1–20.
Visser J, van Geel M, Cornelissen AJM, van der Hulst RRWJ, Qiu SS. Breast cancer-related lymphedema and genetic predisposition: a systematic review of the literature. Lymph Res Biol. 2019;17:288–93.
Wu R, Huang X, Dong X, Zhang H, Zhuang L. Obese patients have higher risk of breast cancer-related lymphedema than overweight patients after breast cancer: a meta-analysis. Ann Translat Med. 2019;7:172.
Chen C, Gu W, Chen Y, et al. Risk factors for postoperative breast cancer-related lymphedema: a meta-analysis. Chin Evid Based Nurs. 2021;7:866–74.
Zhang H, Liu R, Zhu L, et al. Risk factors for breast cancer-related lymphedema in Chinese women: a meta-analysis. Chin Gen Pract. 2021;24:3349–58, 3376.
Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1997;32:513.
Kennedy W, Fruin R, Lue A, Logan SW. Using ecological models of health behavior to promote health care access and physical activity engagement for persons with disabilities. J Patient Exp. 2021;8:23743735211034030.
Schmitz KH, Troxel AB, Dean LT, et al. Effect of home-based exercise and weight loss programs on breast cancer-related lymphedema outcomes among overweight breast cancer survivors: the WISER survivor randomized clinical trial. JAMA Oncol. 2019;5:1605–13.
Perry R, Whitmarsh A, Leach V, Davies P. A comparison of two assessment tools used in overviews of systematic reviews: ROBIS versus AMSTAR-2. Syst Rev. 2021;10:273.
Acknowledgments
This umbrella review was supported by the National Natural Science Foundation of China (72174011).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shen, A., Qiang, W., Zhang, L. et al. Risk Factors for Breast Cancer-Related Lymphedema: An Umbrella Review. Ann Surg Oncol 31, 284–302 (2024). https://doi.org/10.1245/s10434-023-14277-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14277-7