Abstract
Background
The objective of this study was to compare postoperative complication rates and healthcare charges between patients who underwent coordinated versus staged breast surgery and bilateral salpingo-oophorectomy (BSO).
Patients and Methods
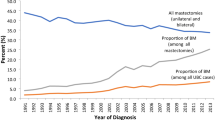
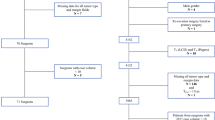
The MarketScan administrative database was used to identify adult female patients with invasive breast cancer or BRCA1/BRCA2 mutations who underwent BSO and breast surgery (lumpectomy or mastectomy with or without reconstruction) between 2010 and 2015. Patients were assigned to the coordinated group if a breast operation and BSO were performed simultaneously or assigned to the staged group if BSO was performed separately. Primary outcomes were (1) incidence of 90-day postoperative complications and (2) 2-year aggregate perioperative healthcare charges. Fisher’s exact tests, Wilcoxon rank-sum tests, and multivariable regression analyses were performed.
Results
Of the 4228 patients who underwent breast surgery and BSO, 412 (9.7%) were in the coordinated group and 3816 (90.3%) were in the staged group. The coordinated group had a higher incidence of postoperative complications (24.0% vs. 17.7%, p < 0.01), higher risk-adjusted odds of postoperative complications [odds ratio (OR) 1.37, 95% confidence interval (CI) 1.06–1.76, p = 0.02], and similar aggregate healthcare charges before (median charges: $106,500 vs. $101,555, p = 0.96) and after risk-adjustment [incidence rate ratio (IRR) 1.00, 95% CI 0.93–1.07; p = 0.95]. In a subgroup analysis, incidence of postoperative complications (12.9% for coordinated operations vs. 11.7% for staged operation, p = 0.73) was similar in patients whose breast operation was a lumpectomy.
Conclusions
While costs were similar, coordinating breast surgery with BSO was associated with more complications in patients who underwent mastectomy, but not in patients who underwent lumpectomy. These data should inform shared decision-making in high-risk patients.
Similar content being viewed by others
References
Daly MB, Pal T, Berry MP, et al. Genetic/familial high-risk assessment: breast, ovarian, and pancreatic, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2021;19(1):77–102.
Ludwig KK, Neuner J, Butler A, Geurts JL, Kong AL. Risk reduction and survival benefit of prophylactic surgery in BRCA mutation carriers, a systematic review. Am J Surg. 2016;212(4):660–9. https://doi.org/10.1016/j.amjsurg.2016.06.010.
AlHilli MM, Al-Hilli Z. Perioperative management of women undergoing risk-reducing surgery for hereditary breast and ovarian cancer. J Minim Invasive Gynecol. 2019;26(2):253–65. https://doi.org/10.1016/j.jmig.2018.09.767.
Schrag D, Kuntz KM, Garber JE, Weeks JC. Life expectancy gains from cancer prevention strategies for women with breast cancer and BRCA1 or BRCA2 mutations. JAMA. 2000;283(5):617–24. https://doi.org/10.1001/jama.283.5.617.
Kauff ND, Domchek SM, Friebel TM, et al. Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: a multicenter, prospective study. J Clin Oncol. 2008;26(8):1331–7. https://doi.org/10.1200/jco.2007.13.9626.
Agnantis NJ, Paraskevaidis E, Roukos D. Preventing breast, ovarian cancer in BRCA carriers: rational of prophylactic surgery and promises of surveillance. Ann Surg Oncol. 2004;11(12):1030–4. https://doi.org/10.1245/ASO.2004.09.910.
Bayraktar S, Arun B. BRCA mutation genetic testing implications in the United States. Breast. 2017;31:224–32. https://doi.org/10.1016/j.breast.2016.11.021.
Domchek SM, Friebel TM, Singer CF, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304(9):967–75. https://doi.org/10.1001/jama.2010.1237.
Verheijen RHM, Hermsen B. The clinical implications of genetics. BRCA1- and BRCA2-positive: How do I proceed? Implications for ovarian cancer prevention. Ann Oncol. 2008;19:84–6. https://doi.org/10.1093/annonc/mdn317.
Metcalfe K, Lynch HT, Foulkes WD, et al. Effect of oophorectomy on survival after breast cancer in BRCA1 and BRCA2 mutation carriers. JAMA Oncol. 2015;1(3):306–13. https://doi.org/10.1001/jamaoncol.2015.0658.
Pierce LJ, Levin AM, Rebbeck TR, et al. Ten-year multi-institutional results of breast-conserving surgery and radiotherapy in BRCA1/2-associated stage I/II breast cancer. J Clin Oncol. 2006;24(16):2437–43. https://doi.org/10.1200/JCO.2005.02.7888.
Valachis A, Nearchou AD, Lind P. Surgical management of breast cancer in BRCA-mutation carriers: a systematic review and meta-analysis. Breast Cancer Res Treat. 2014;144(3):443–55. https://doi.org/10.1007/s10549-014-2890-1.
Batista LI, Lu KH, Beahm EK, Arun BK, Bodurka DC, Meric-Bernstam F. Coordinated prophylactic surgical management for women with hereditary breast-ovarian cancer syndrome. BMC Cancer. 2008;8(1):101. https://doi.org/10.1186/1471-2407-8-101.
Tevis SE, Steiman JG, Neuman HB, Greenberg CC, Wilke LG. Postoperative complications in combined gynecologic, plastic, and breast surgery: an analysis from National Surgical Quality Improvement Program. Breast J. 2019;25(6):1111–6. https://doi.org/10.1111/tbj.13429.
Jayaraman AP, Boyd T, Hampton SN, Haddock NT, Teotia SS. The impact of combined risk-reducing gynecological surgeries on outcomes in DIEP flap and tissue-expander breast reconstruction. Plast Surg (Oakv). 2020;28(2):112–6. https://doi.org/10.1177/2292550320925905.
Del Corral GA, Wes AM, Fischer JP, Serletti JM, Wu LC. Outcomes and cost analysis in high-risk patients undergoing simultaneous free flap breast reconstruction and gynecologic procedures. Ann Plast Surg. 2015;75(5):534–8. https://doi.org/10.1097/sap.0000000000000156.
Elmi M, Azin A, Elnahas A, McCready DR, Cil TD. Concurrent risk-reduction surgery in patients with increased lifetime risk for breast and ovarian cancer: an analysis of the National Surgical Quality Improvement Program (NSQIP) database. Breast Cancer Res Treat. 2018;171(1):217–23. https://doi.org/10.1007/s10549-018-4818-7.
Sroka CJ, Nagaraja HN. Odds ratios from logistic, geometric, Poisson, and negative binomial regression models. BMC Med Res Methodol. 2018;18(1):112. https://doi.org/10.1186/s12874-018-0568-9.
Ma IT, Gray RJ, Wasif N, et al. Outcomes of concurrent breast and gynecologic risk reduction surgery. Ann Surg Oncol. 2017;24(1):77–83. https://doi.org/10.1245/s10434-016-5479-6.
Chapman JS, Roddy E, Panighetti A, et al. Comparing coordinated versus sequential salpingo-oophorectomy for BRCA1 and BRCA2 mutation carriers with breast cancer. Clin Breast Cancer. 2016;16(6):494–9.
Khadim MF, Eastwood P, Price J, Morrison P, Khan K. Multidisciplinary one-stage risk-reducing gynaecological and breast surgery with immediate reconstruction in BRCA-gene carrier women. Eur J Surg Oncol. 2013;39(12):1346–50. https://doi.org/10.1016/j.ejso.2013.09.018.
Holzmer S, Davila A, Martin MC. Cost utility analysis of staged versus single-stage cleft lip and palate repair. Ann Plast Surg. 2020;84(5S Suppl 4):S300-s306. https://doi.org/10.1097/sap.0000000000002255.
Lawson EH, Hall BL, Louie R, et al. Association between occurrence of a postoperative complication and readmission: implications for quality improvement and cost savings. Ann Surg. 2013;258(1):10–8.
Encinosa WE, Hellinger FJ. Advances in Patient Safety
What happens after a patient safety event? Medical expenditures and outcomes in medicare. In: Henriksen K, Battles JB, Marks ES, Lewin DI, eds. Advances in Patient Safety: From Research to Implementation (Volume 1: Research Findings). Agency for Healthcare Research and Quality (US); 2005.
Acknowledgements
This research was supported in part by the Shared Resource of the Colorado Cancer Center support Grant P30CA046934 and University of Colorado Department of Surgery Academic Enrichment Fund seed grant. Further support for this work was provided by Grant 2020141 from the Doris Duke Charitable Foundation and University of Colorado School of Medicine and the Paul Calabresi Clinical Scholars Award.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design performed by SV, KV, VH, GA, JA, CK, KR, SK, and ST, data collection performed by SV, MB, VH, and ST, analysis and interpretation of results performed by SV, MB, KV, VH, LB, and ST, and draft manuscript preparation and critical revision performed by SV, MB, KV, VH, LB, GA, JA, CK, KR, LB, SK, and ST All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Disclosures
Research was presented at American Society of Breast Surgeons Annual Meeting in Las Vegas, NV on 6–10 April 2022. The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
American Society of Breast Surgeons Annual Meeting, Las Vegas, NV, April 6-10, 2022.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vemuru, S.R., Bronsert, M., Vossler, K. et al. Postoperative Outcomes After Staged Versus Coordinated Breast Surgery and Bilateral Salpingo-Oophorectomy. Ann Surg Oncol 30, 5667–5680 (2023). https://doi.org/10.1245/s10434-023-13630-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13630-0