Abstract
Background
Multiple composite indices of small-area socioeconomic characteristics have been used to examine how neighborhood characteristics influence cancer care, but there is little consensus regarding how to use them. This scoping review aimed to summarize the use of these indices in cancer literature and their association with outcomes.
Methods
A search was conducted to identify studies from 2015 to 2021 that investigated cancer incidence, disease stage at diagnosis, and mortality using area-based indices of deprivation as an independent variable. Studies were screened and assessed for eligibility. Data were extracted regarding the geospatial and statistical use of these indices.
Results
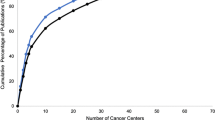
All the inclusion criteria were met by 45 studies. The area level of analysis was at the census tract level in 19 studies (42.3%), the county level in 15 studies (33.3%), the block group level in 6 studies (13.3%), and the ZIP code level in 5 studies (11.1%). Altogether, 18 unique indices were used, with 4 indices used most frequently. Of the studies that used their indices ordinally, 3 defined high and low deprivation dichotomously, 10 used tertiles, 13 used quartiles, and 15 used quintiles. Of the 45 studies, 34 (76%) showed a significant association between area deprivation and cancer-related outcomes.
Conclusions
Neighborhood deprivation indices are most commonly used at the census tract level and ordinally as quintiles. Despite variance in methods, there is a strong indication that deprived areas are at adverse odds with cancer-related outcomes. Further study investigating deprivation in the context of cancer can inform drivers of inequity and identify potential targets for care delivery and policy interventions.



Similar content being viewed by others
References
Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–78.
Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156:471–82.
Diez-Roux AV, Kiefe CI, Jacobs DR Jr, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies [published correction appears in Ann Epidemiol. 2001;30:924. [Roux AV corrected to Diez-Roux]. Ann Epidemiol. 2001;11:395–405.
Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12:703–11.
Census Bureau, U. Glossary. [online] Census.gov (2022). Accessed 10 Feb 2022 at https://www.census.gov/programs-surveys/geography/about/glossary.html#par_textimage_13.
Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. 2003;93:1137–43.
Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83:1041–62.
Saldana-Ruiz N, Clouston SA, Rubin MS, Colen CG, Link BG. Fundamental causes of colorectal cancer mortality in the United States: understanding the importance of socioeconomic status in creating inequality in mortality. Am J Public Health. 2013;103:99–104.
Rubin MS, Clouston S, Link BG. A fundamental cause approach to the study of disparities in lung cancer and pancreatic cancer mortality in the United States. Soc Sci Med. 2014;100:54–61.
Kind AJH, Buckingham W. Making neighborhood disadvantage metrics accessible: the neighborhood atlas. N Engl Jl Med. 2018;378:2456–8.
Atsdr.cdc.gov. 2015. CDC/ATSDR’s Social Vulnerability Index (SVI). [online] Accessed 15 Aug 2021 at https://www.atsdr.cdc.gov/placeandhealth/svi/index.html.
SEER. n.d. Census Tract-level SES and Rurality Database—SEER*Stat. [online] Accessed 15 Aug 2021 at https://seer.cancer.gov/seerstat/databases/census-tract/index.html.
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141–6.
Davis K, Drey N, Gould D. What are scoping studies? A review of the nursing literature. Int J Nurs Stud. 2009;46:1386–400.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. 2005;8:19–32.
Yu M, Tatalovich Z, Gibson JT, Cronin KA. Using a composite index of socioeconomic status to investigate health disparities while protecting the confidentiality of cancer registry data. Cancer Causes Control. 2014;25:81–92.
Pruitt SL, Shim MJ, Mullen PD, Vernon SW, Amick BC III. Association of area socioeconomic status and breast, cervical, and colorectal cancer screening: a systematic review. Cancer Epidemiol Biomark Prev. 2009;18:2579–99.
Jayasekera J, Onukwugha E, Cadham C, et al. An ecological approach to monitor geographic disparities in cancer outcomes. PLoS ONE. 2019;14:e0218712. https://doi.org/10.1371/journal.pone.0218712.
Song S, Duan Y, Huang J, et al. Socioeconomic inequalities in premature cancer mortality among U.S. counties during 1999 to 2018. Cancer Epidemiol Biomark Prev. 2021;30:1375–86.
Chakravarthy R, Stallings SC, Velez Edwards DR, et al. Determinants of stage at diagnosis of HPV-related cancer including area deprivation and clinical factors. J Public Health Oxford. 2022;44:18–27.
Wheeler DC, Czarnota J, Jones RM. Estimating an area-level socioeconomic status index and its association with colonoscopy screening adherence. PLoS ONE. 2017;12:e0179272. https://doi.org/10.1371/journal.pone.0179272.
Meliker JR, Jacquez GM, Goovaerts P, Copeland G, Yassine M. Spatial cluster analysis of early-stage breast cancer: a method for public health practice using cancer registry data. Cancer Causes Control. 2009;20:1061–9. https://doi.org/10.1007/s10552-009-9312-4. (Epub 15 February 2009. PMID: 19219634; PMCID: PMC4337842).
Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161:765–74.
Ortiz AG, Wiese D, Sorice KA, et al. Liver cancer incidence and area-level geographic disparities in Pennsylvania: a geo-additive approach. Int J Environ Res Public Health. 2020;17:7526.
Krieger N, Waterman PD, Spasojevic J, Li W, Maduro G, Van Wye G. Public health monitoring of privilege and deprivation with the index of concentration at the extremes. Am J Public Health. 2016;106:256–63.
Siegel J, Engelhardt KE, Hornor MA, Morgan KA, Lancaster WP. Travel distance and its interaction with patient and hospital factors in pancreas cancer care. Am J Surg. 2021;221:819–25. https://doi.org/10.1016/j.amjsurg.2020.08.023. (Epub 25 August 2020 PMID: 32891396).
Siegel JB, Allen S, Engelhardt KE, Morgan KA, Lancaster WP. Travel distance and overall survival in hepatocellular cancer care. Am J Surg. 2021;222:584–93. https://doi.org/10.1016/j.amjsurg.2020.12.052. (Epub 31 December 2020 PMID: 33413878).
Fong AJ, Lafaro K, Ituarte PHG, Fong Y. Association of living in urban food deserts with mortality from breast and colorectal cancer. Ann Surg Oncol. 2021;28:1311–9. https://doi.org/10.1245/s10434-020-09049-6. (Epub 25 August 2020. PMID: 32844294; PMCID: PMC8046424).
Fay KA, Maeder ME, Emond JA, Hasson RM, Millington TM, Finley DJ, Phillips JD. Residing in a food desert is associated with an increased risk of readmission following esophagectomy for cancer. J Thorac Dis. 2022;14:1854–68. https://doi.org/10.21037/jtd-21-1637.PMID:35813712;PMCID:PMC9264063.
Singh GK, Miller BA, Hankey BF. Changing area socioeconomic patterns in U.S. cancer mortality, 1950–1998: part II–lung and colorectal cancers. J Natl Cancer Inst. 2002;94:916–25. https://doi.org/10.1093/jnci/94.12.916. (PMID: 12072545).
Chang HY, Hatef E, Ma X, Weiner JP, Kharrazi H. Impact of Area Deprivation Index on the performance of claims-based risk-adjustment models in predicting health care costs and utilization. Popul Health Manage. 2021;24:403–11. https://doi.org/10.1089/pop.2020.0135. (Epub 10 September 2020 PMID: 33434448).
Ghirimoldi FM, Schmidt S, Simon RC, Wang CP, Wang Z, Brimhall BB, et al. Association of socioeconomic Area Deprivation Index with hospital readmissions after colon and rectal surgery. J Gastrointest Surg. 2021;25:795–808. https://doi.org/10.1007/s11605-020-04754-9(Epub8September2020.PMID:32901424;PMCID:PMC7996389).
Krieger N, Singh N, Waterman PD. Metrics for monitoring cancer inequities: residential segregation, the Index of Concentration at the Extremes (ICE), and breast cancer estrogen receptor status (USA, 1992–2012). Cancer Causes Control. 2016;27:1139–51. https://doi.org/10.1007/s10552-016-0793-7. (Epub 2016 Aug 8 PMID: 27503397).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Markey, C., Bello, O., Hanley, M. et al. The Use of Area-Level Socioeconomic Indices in Evaluating Cancer Care Delivery: A Scoping Review. Ann Surg Oncol 30, 2620–2628 (2023). https://doi.org/10.1245/s10434-023-13099-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13099-x