Abstract
Purpose
This study was designed to assess the computed tomography maximum (CTmax) value on pretherapeutic arterial phase computed tomography (APCT) images to predict pancreatic neuroendocrine tumours (pNETs) recurrence and clarify its role in predicting the outcome of tumour therapy.
Methods
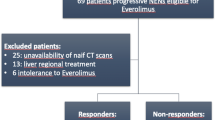
This retrospective study enrolled 250 surgical patients and 24 nonsurgical patients with sunitinib-based treatment in our hospital from 2008 to 2019. CT images were assessed, the maximum value was defined as “CTmax,” and recurrence-free survival (RFS) or progression-free survival (PFS) was compared between a high-CTmax group and a low-CTmax group among patients who underwent surgical resection or nonsurgical, sunitinib-based treatment according to the CTmax cutoff value.
Results
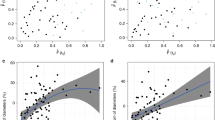
In ROC curve analysis, a CTmax of 108 Hounsfield units, as the cutoff value, achieved an AUC of 0.796 in predicting recurrence. Compared with the low-CTmax group, the high-CTmax group had a longer RFS (p < 0.001). Low CTmax was identified as an independent factor for RFS (p < 0.001) in multivariate analysis; these results were confirmed using the internal validation set. The CTmax value was significantly correlated with the microvascular density (MVD) value (p < 0.001) and the vascular endothelial growth factor receptor 2 (VEGFR2) score (p < 0.001). Furthermore, the high-CTmax group had a better PFS than the low-CTmax group among the sunitinib treatment group (p = 0.007).
Conclusions
The tumour CTmax on APCT might be a potential and independent indicator for predicting recurrence in patients who have undergone surgical resection and assessing the efficacy of sunitinib for patients with advanced metastatic pNETs.





Similar content being viewed by others
References
Bezzi C, Mapelli P, Presotto L, et al. Radiomics in pancreatic neuroendocrine tumors: methodological issues and clinical significance. Eur J Nucl Med Mol Imag. 2021;48(12):4002–15.
Egal ESA, Jacenik D, Soares HP, et al. Translational challenges in pancreatic neuroendocrine tumor immunotherapy. Biochim Biophys Acta Rev Cancer. 2021;1876(2):188640.
Ferraro V, Tedeschi M, Laera L, et al. The role of laparoscopic surgery in localized pancreatic neuroendocrine tumours. Curr Treat Options Oncol. 2021;22(4):27.
Mauriello C, Napolitano S, Gambardella C, et al. Conservative management and parenchyma-sparing resections of pancreatic neuroendocrine tumors: literature review. Int J Surg. 2015;21(Suppl 1):S10–4.
Hua J, Shi S, Xu J, et al. Expression patterns and prognostic value of DNA damage repair proteins in resected pancreatic neuroendocrine neoplasms. Ann Surg. 2022;275(2):e443–52.
Halfdanarson TR, Rubin J, Farnell MB, et al. Pancreatic endocrine neoplasms: epidemiology and prognosis of pancreatic endocrine tumors. Endocr Relat Cancer. 2008;15(2):409–27.
Metz DC, Jensen RT. Gastrointestinal neuroendocrine tumors: pancreatic endocrine tumors. Gastroenterology. 2008;135(5):1469–92.
Mizumoto T, Toyama H, Terai S, et al. Prediction of lymph node metastasis in pancreatic neuroendocrine tumors by contrast enhancement characteristics. Pancreatology. 2017;17(6):956–61.
Singh S, Chan DL, Moody L, et al. Recurrence in resected gastroenteropancreatic neuroendocrine tumors. JAMA Oncol. 2018;4(4):583–5.
Kwekkeboom DJ, Krenning EP. Peptide receptor radionuclide therapy in the treatment of neuroendocrine tumors. Hematol Oncol Clin North Am. 2016;30(1):179–91.
Sorbye H, Welin S, Langer SW, et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24(1):152–60.
Frost M, Lines KE, Thakker RV. Current and emerging therapies for PNETs in patients with or without MEN1. Nat Rev Endocrinol. 2018;14(4):216–27.
Kaderli RM, Spanjol M, Kollár A, et al. Therapeutic options for neuroendocrine tumors: a systematic review and network meta-analysis. JAMA Oncol. 2019;5(4):480–9.
Cives M, Strosberg JR. Gastroenteropancreatic neuroendocrine tumors. CA Cancer J Clin. 2018;68(6):471–87.
Lamarca A, Barriuso J, Kulke M, et al. Determination of an optimal response cut-off able to predict progression-free survival in patients with well-differentiated advanced pancreatic neuroendocrine tumours treated with sunitinib: an alternative to the current RECIST-defined response. Br J Cancer. 2018;118(2):181–8.
Amoroso V, Fazio N, Mosca A, et al. When should everolimus be administered in the natural history of pancreatic neuroendocrine tumors? J Clin Oncol. 2017;35(13):1487–8.
Ma ZY, Gong YF, Zhuang HK, et al. Pancreatic neuroendocrine tumors: A review of serum biomarkers, staging, and management. World J Gastroenterol. 2020;26(19):2305–22.
Fujimori N, Osoegawa T, Lee L, et al. Efficacy of endoscopic ultrasonography and endoscopic ultrasonography-guided fine-needle aspiration for the diagnosis and grading of pancreatic neuroendocrine tumors. Scand J Gastroenterol. 2016;51(2):245–52.
Guo CG, Ren S, Chen X, et al. Pancreatic neuroendocrine tumor: prediction of the tumor grade using magnetic resonance imaging findings and texture analysis with 3-T magnetic resonance. Cancer Manag Res. 2019;11:1933–44.
Worhunsky DJ, Krampitz GW, Poullos PD, et al. Pancreatic neuroendocrine tumours: hypoenhancement on arterial phase computed tomography predicts biological aggressiveness. HPB (Oxford). 2014;16(4):304–11.
Rodallec M, Vilgrain V, Couvelard A, et al. Endocrine pancreatic tumours and helical CT: contrast enhancement is correlated with microvascular density, histoprognostic factors and survival. Pancreatology. 2006;6(1–2):77–85.
Lewis RB, Lattin GE Jr, Paal E. Pancreatic endocrine tumors: radiologic-clinicopathologic correlation. Radiographics. 2010;30(6):1445–64.
Pavel M, Jann H, Prasad V, et al. NET blood transcript analysis defines the crossing of the clinical rubicon: when stable disease becomes progressive. Neuroendocrinology. 2017;104(2):170–82.
Nakano A, Hayano K, Tochigi T, et al. Prediction of non-functioning pancreatic neuroendocrine tumor grades with fractal analysis of preoperative contrast-enhanced computed tomography images. Eur J Radiol. 2021;141:109803.
Sadri D, Shahsavari F, Hezarkhani M, et al. Expression of CD34 and CD31 in central and peripheral giant cell granulomas. J Dent (Shiraz). 2019;20(1):10–5.
Frilling A, Li J, Malamutmann E, et al. Treatment of liver metastases from neuroendocrine tumours in relation to the extent of hepatic disease. Br J Surg. 2009;96(2):175–84.
Yano M, Misra S, Carpenter DH, et al. Pancreatic neuroendocrine tumors: computed tomography enhancement, but not histological grade, correlates with tumor aggression. Pancreas. 2017;46(10):1366–72.
VandenBussche CJ, Allison DB, Graham MK, et al. Alternative lengthening of telomeres and ATRX/DAXX loss can be reliably detected in FNAs of pancreatic neuroendocrine tumors. Cancer Cytopathol. 2017;125(7):544–51.
Singhi AD, Liu TC, Roncaioli JL, et al. Alternative lengthening of telomeres and loss of DAXX/ATRX expression predicts metastatic disease and poor survival in patients with pancreatic neuroendocrine tumors. Clin Cancer Res. 2017;23(2):600–9.
Marinoni I, Kurrer AS, Vassella E, et al. Loss of DAXX and ATRX are associated with chromosome instability and reduced survival of patients with pancreatic neuroendocrine tumors. Gastroenterology. 2014;146(2):453-60.e455.
Kim JY, Brosnan-Cashman JA, An S, et al. Alternative lengthening of telomeres in primary pancreatic neuroendocrine tumors is associated with aggressive clinical behavior and poor survival. Clin Cancer Res. 2017;23(6):1598–606.
Pea A, Yu J, Marchionni L, et al. Genetic analysis of small well-differentiated pancreatic neuroendocrine tumors identifies subgroups with differing risks of liver metastases. Ann Surg. 2020;271(3):566–73.
Vinik AI, Raymond E. Pancreatic neuroendocrine tumors: approach to treatment with focus on sunitinib. Therap Adv Gastroenterol. 2013;6(5):396–411.
Acknowledgment
This work was supported in part by the National Natural Science Foundation of China (U21A20374), the Shanghai Municipal Science and Technology Major Project (21JC1401500), the Scientific Innovation Project of Shanghai Education Committee (2019-01-07-00-07-E00057), the Clinical Research Plan of Shanghai Hospital Development Center (SHDC2020CR1006A), the Xuhui District Artificial Intelligence Medical Hospital Cooperation Project (2021-011), the Shanghai Municipal Science and Technology Commission (20ZR1471100), and the National Science Foundation of China (No. 82141129, 82173281, 82173282, 82172577 and 82172948).
Author information
Authors and Affiliations
Contributions
SRJ, XJY, and WT contributed to the conception of the study; ZY, XL, WHZ, HLG, YQ, and JC contributed significantly to analysis and manuscript preparation; HDC, ZL, YHH, XMC, YZ, and XWX performed the data analyses and wrote the manuscript; HDC helped perform the analysis with constructive discussions.
Corresponding authors
Ethics declarations
Disclosure
The authors report no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, H., Li, Z., Hu, Y. et al. Maximum Value on Arterial Phase Computed Tomography Predicts Prognosis and Treatment Efficacy of Sunitinib for Pancreatic Neuroendocrine Tumours. Ann Surg Oncol 30, 2988–2998 (2023). https://doi.org/10.1245/s10434-022-12693-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12693-9