Abstract
Background
This study seeks to evaluate the impact of breast cancer (BRCA) gene status on tumor dissemination pattern, surgical outcome and survival in a multicenter cohort of paired primary ovarian cancer (pOC) and recurrent ovarian cancer (rOC).
Patients and Methods
Medical records and follow-up data from 190 patients were gathered retrospectively. All patients had surgery at pOC and at least one further rOC surgery at four European high-volume centers. Patients were divided into one cohort with confirmed mutation for BRCA1 and/or BRCA2 (BRCAmut) and a second cohort with BRCA wild type or unknown (BRCAwt). Patterns of tumor presentation, surgical outcome and survival data were analyzed between the two groups.
Results
Patients with BRCAmut disease were on average 4 years younger and had significantly more tumor involvement upon diagnosis. Patients with BRCAmut disease showed higher debulking rates at all stages. Multivariate analysis showed that only patient age had significant predictive value for complete tumor resection in pOC. At rOC, however, only BRCAmut status significantly correlated with optimal debulking. Patients with BRCAmut disease showed significantly prolonged overall survival (OS) by 24.3 months. Progression-free survival (PFS) was prolonged in the BRCAmut group at all stages as well, reaching statistical significance during recurrence.
Conclusions
Patients with BRCAmut disease showed a more aggressive course of disease with earlier onset and more extensive tumor dissemination at pOC. However, surgical outcome and OS were significantly better in patients with BRCAmut disease compared with patients with BRCAwt disease. We therefore propose to consider BRCAmut status in regard to patient selection for cytoreductive surgery, especially in rOC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Maximum tumor reduction and platinum-based chemotherapy eventually followed by maintenance with poly(ADP-ribose) polymerase inhibitors (PARPi) alone or in combination with antiangiogenesis is the standard treatment for pOC.1 However, in the recurrent state of disease, selection of the best therapeutic option depends on the recurrence timing and pattern and is considerably more complex.2 Recently published data of a randomized phase III trial conducted by Harter et al. demonstrated that secondary cytoreduction significantly extends OS as well as PFS if complete tumor resection is achieved.3 Currently, the Arbeitsgemeinschaft Gynaekologische Onkologie (AGO) score, consisting of three items (complete resection at initial surgery, good performance status, and absence of ascites) represents a well-validated tool to identify patients most likely to achieve complete secondary cytoreduction.4,5,6 However, studies have shown that patients with negative AGO score can still achieve complete resection, thus further refinement of the score is necessary.7,8,9 Hence, additional individual criteria to inform the selection of patients suitable for secondary debulking surgery must be identified.10
Since ovarian cancer is known to show high interindividual heterogeneity in clinical presentation and treatment response, as well as high recurrence risk, our main focus in recent research has been to determine the impact of BRCA status on this diversity.11 In this context, BRCA mutation status predicts the effects of PARPi with impressive clinical results.12 Moreover, the effectiveness of PARPi as maintenance treatment for newly diagnosed advanced ovarian cancer has also been proven.13 Nevertheless, surgical cytoreduction will continue to be an important therapeutic strategy to efficiently remove a large number of cancer cells at a time, even in the situation of recurrence.14 Patients with no residual tumor mass following primary tumor debulking were the ones who benefited most from maintenance with PARPi.15 However, the relevance of BRCA mutation status as a predictive factor for platinum sensitivity and targeting point for individualized therapy options is increasing.16,17 With the increasing importance of surgical treatment in rOC, the role of BRCA mutation status in secondary resection has not yet been sufficiently investigated.18
It is the aim of this multicenter retrospective study to evaluate the impact of BRCA mutation status on clinical presentation and surgical outcome in the primary and recurrent disease state, as well as patient survival.
Patients and Methods
Patient Enrollment
Paired tumor tissue samples, surgical reports, medical records and follow-up data of patients from both pOC and all available rOC treatment lines were gathered retrospectively from the Ovarian Cancer Therapy-Innovative Models Prolong Survival (OCTIPS, agreement no. 279113-2) consortium database. All patients underwent cytoreductive surgery for pOC and rOC disease with maximum effort followed by platinum-based chemotherapy. Tissue samples irrespective of tumor stage were harvested during tumor debulking surgery between 1984 and 2019 and subsequently underwent histopathological analysis to confirm high-grade serous ovarian cancer (HGSOC) diagnosis. Tumor tissue samples were also used to retrospectively determine BRCA mutation status. After completion of surgery, a standardized interview with the surgeon was conducted to assess the macroscopic spread of tumor mass and the surgical procedures performed. If necessary, surgical reports were additionally reviewed to complement surgical data. All patients were treated in one of the following accredited European gynecological oncology referral centers: Charité-Universitätsmedizin Berlin (Germany), Medical University of Innsbruck (Austria), Katholieke Universiteit Leuven (Belgium) and University of Edinburgh (United Kingdom). The study received favorable approval from each local ethics committee (EK207/2003, EK260, ML2524, and EK130113).
Inclusion criteria were presence of HGSOC with availability of thorough clinicopathological and complete surgical documentation for both primary disease and at least one recurrence. Exclusion criteria were lack of the aforementioned data, other histologies, or inadequate follow-up.
Patient Clinicopathological Data
Informed consent was collected as per local ethics committee requirements prior to enrollment into the study. Clinicopathological data were obtained from the OCTIPS consortium database and processed anonymously. The 1988 International Federation of Gynecology and Obstetrics (FIGO) classification was used to determine clinical stage and the 2014 World Health Organization (WHO) classification to histologically assess the tumor tissue samples.19 To evaluate the patterns of intraoperative disease presentation, the abdominal cavity was divided into three compartments: lower abdomen (level 1, including uterus, Douglas, bladder and ureters, rectum, sigma, and vaginal stump), periumbilical section (level 2, including colon and small intestine), and upper abdomen (level 3, including omentum majus, bursa omentalis, spleen, stomach, liver, and diaphragm), according to the concept of the Intraoperative Mapping of Ovarian cancer (IMO) system.20 Extension of surgical procedures was measured by application of the surgical complexity scoring (SCS) system, defined elsewhere.21 OC recurrence was defined on the basis of clinical examination, cross-sectional imaging using the response evaluation criteria in solid tumors (RECIST) criteria, and serum marker evaluation.22 Residual tumor was defined as negative by the surgeon if macroscopically absent at the end of cytoreduction.
Statistical Analysis
IBM SPSS version 24 (IBM Corporation, Armonk, NY) was used to perform the statistical analysis of the patient cohort at Charité-Universitätsmedizin Berlin. Differences between the BRCAmut and BRCAwt cohorts concerning the investigated factors were analyzed using Pearson’s chi-squared test, Fisher’s exact test, Mann–Whitney U test, and Kendall’s tau–b test where appropriate.
OS was defined as the period from first diagnosis of ovarian cancer until death or last contact. PFS was determined as the interval from surgery until progression of disease or death. Both OS and PFS were estimated by Kaplan–Meier analysis, and survival differences were analyzed using the log-rank test. Significance level was set at a two-sided p-value ≤ 0.05. Multivariate analysis was performed to estimate the probability of complete tumor resection during pOC and rOC surgery, consisting of BRCA mutation status, patient age, and SCS.
Results
Patient Characteristics
A total of 208 patients were included in the study. To ensure that all patients were treated with surgery followed by platinum-based chemotherapy, all cases prior to 2000 were excluded. Seven further patients had to be excluded from the study due to insufficient clinicopathological documentation. In total, 190 patients were included in the final analysis of the study. Patient enrollment is visualized in Fig. 1. Mean follow-up from primary surgery was 51.7 months (range 6.7–214 months), with 124 deaths occurring during that period. All included patients had HGSOC. The majority of diagnoses (77.89%) were FIGO stage 3. A total of 138 women (72.6%) had known BRCA status [30 (15.8%) BRCA1mut, 19 (10%) BRCA2mut, and 92 (48.4%) BRCAwt] while it was unknown in 52 (27.4%) at the end of follow-up. Patients with a known BRCA mutation were on average 4 years younger at time of diagnosis (53 versus 57 years, p = 0.018). Over 90% of all patients were Caucasian, thus no further specification of ethnicity was performed. Patient characteristics are presented in Table 1.
Tumor Dissemination Pattern and Surgical Outcome
No statistical significance was found between the two groups in terms of SCS based upon the complexity and number of procedures performed during primary and secondary cytoreductive surgery. In particular, intermediate surgical complexity was achieved in both groups during pOC, consisting of 6.0 points for the BRCAmut group (16.2% low, 62.2% intermediate, and 21.6% high surgical complexity) and 6.0 points for the BRCAwt cohort (10.2% low, 62% intermediate, and 27.8% high; p = 0.407). During secondary debulking, the median surgical complexity score was lower compared with primary surgery, with 3.0 points for the BRCAmut group (70% low and 30% intermediate) and 2.0 points for the BRCAwt group (79.5% low and 20.5% intermediate; p = 0.089). Patient characteristics are presented in Table 1.
Results for surgical outcome in relation to BRCA status are presented in Table 2. Patients with BRCAmut disease showed higher disease burden at IMO level 2 during primary surgery compared with patients with BRCAwt disease (91.7% versus 75%, p = 0.034). No other significant differences could be identified between the two groups in terms of tumor dissemination at primary or recurrent disease stages.
Complete tumor resection was achieved more often in the BRCAmut group during primary debulking surgery (82.6% versus 75.7%, p = 0.329), as well as the first (82.1% versus 56.4%, p = 0.004) and second/third relapse (75% versus 26.8%, p = 0.005), reaching statistical significance. Multivariate analysis of surgical outcome at primary debulking surgery revealed that only age was a significant predictor (OR 1.062; 95% CI 1.011–1.116; p = 0.016) of complete tumor resection, whereas BRCA mutation status (OR 0.663; CI 95% 0.202–2.179; p = 0.499) and SCS (OR 0.999; CI 95% 0.193–5.180; p = 0.999) showed no statistical significance. During secondary debulking surgery, however, only BRCA mutation status remained a statistically significant predictive factor (OR 0.214; CI 95% 0.078–0.587; p = 0.003) for complete tumor resection. Age (OR 0.972; CI 95% 0.939–1.007; p = 0.115) and surgical complexity (OR 0.557; CI 95% 0.207–1.501; p = 0.247) failed to reach statistical significance.
Focusing on the intraoperative presence of peritoneal carcinomatosis, as described by the surgeon, no significant difference could be determined between the BRCAmut and BRCAwt cohorts. In particular, involvement of the peritoneum was 76.1% versus 75.7% (p = 0.957) during pOC, 56.4% versus 60.7% (p = 0.638) in first recurrence, and 63.6% versus 68.3% (p = 0.770) in second/third recurrence, respectively.
Preoperative cancer antigen 125 (CA-125) levels were significantly higher in the BRCAmut cohort of pOC (731 versus 199 U/ml; p = 0.021) and first recurrence (241 versus 96 U/ml, p = 0.006). No significant difference could be detected during further recurrences.
Intraoperative ascites volumes did not show significant differences at pOC. The majority of patients in both groups had no ascites at initial presentation (53.5% versus 39.1%; p = 0.152). No significant differences in intraoperative ascites levels could be measured in the relapse situation.
Survival
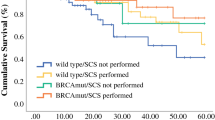
OS was significantly prolonged in the BRCAmut cohort compared with the BRCAwt patients (80.6 versus 56.3 months, p = 0.003, Fig. 2). PFS for BRCAmut and BRCAwt subgroups was 26 and 17 months in the primary situation (p = 0.182, Fig. 3), 22 versus 15 months after first relapse (p = 0.025, Fig. 4), and 11 versus 8 months after second or third relapse (p = 0.118, Fig. 5).
Discussion
Summary of Main Findings
This study was conducted to evaluate and compare the role of BRCAmut status in clinical presentation, surgical outcome in the primary and recurrent disease state, as well as patient survival in a multicenter cohort of patients with HGSOC disease with paired primary and relapsed tissue samples. The study showed that BRCAmut correlates with more frequent extrapelvic presentation at initial diagnosis. Moreover, the BRCAmut cohort presented with higher optimal debulking rates at all stages. Patients with BRCAmut disease showed a significant median OS benefit of 24.3 months compared with the BRCAwt cohort. At secondary debulking surgery, multivariate analysis confirmed positive BRCA status as an independent favorable factor for complete macroscopic tumor resection. Patient characteristics of our study cohort were well comparable to other published OC collectives in terms of patient age at primary diagnosis and percentage of BRCAmut, for example.23,24
Results in the Context of Published Literature
The comparison of tumor dissemination patterns revealed that patients with BRCAmut disease showed a more aggressive course of disease during pOC, with significantly more extensive involvement of the mid-abdomen compared with the BRCAwt group. However, this phenomenon vanishes throughout the course of disease and no significant differences could be determined during rOC stages. This was confirmed by Marchetti et al., who examined the tumor dissemination pattern between patients with BRCAmut and BRCAwt disease and could not detect any significant differences at recurrence.25
Interestingly, even though patients with BRCAmut disease showed more extrapelvic tumor involvement in pOC, surgical effort to achieve maximum reduction of tumor mass did not differ in both groups, at either the primary or recurrent stage. Additionally, patients with BRCAmut disease showed higher rates of complete cytoreduction at all times. Although the difference in patients with pOC disease with complete tumor resection did not reach statistical significance compared with the BRCAwt group, optimal debulking was significantly more often achieved during rOC surgery in the BRCAmut cohort. In a recently published study by Ataseven et al., these findings were largely confirmed in a great population of 1221 patients with pOC disease.26 Similarly to our findings, the BRCAmut cohort showed higher rates of complete tumor resection compared with their BRCAwt counterparts but did not reach statistical significance, and surgical complexity was not significantly different between both groups. However, median follow-up was considerably shorter, at 31 months, and the study focused only on treatment in the pOC situation. To conclude, it is conceivable that, owing to biologic characteristics of BRCAmut OC cells, primary occurrence of disease is earlier, but tumor invasion at recurrence seems to be less aggressive. Therefore, surgery followed by an adequate adjuvant treatment line is still very effective, even during rOC, and should be the treatment modality pursued.
As already described in previous studies, we confirmed significantly younger age at primary diagnosis in patients with BRCAmut disease.27,28 Moreover, the BRCAmut cohort showed significantly prolonged OS, which is also consistent with existing published literature.29,30 However, it has been a topic of international debate whether improved survival, operability, and response rates to therapy among the BRCAmut group are solely caused by the fact that these patients are younger, or whether other tumor characteristics play an important role in that process as well.
Multivariate analysis to predict complete macroscopic tumor resection in our pOC cohort revealed that only age at diagnosis had a significant effect. This finding is in line with data by Hyman et al., where patient’s age was found to be a significant predictor for surgical outcome at primary debulking, whereas BRCA mutation status was not.31 The impact of BRCA status on surgical outcome in rOC, however, has not been sufficiently investigated. In this study, multivariate analysis detected that BRCA mutation status is the only significant predictive factor for complete resection in rOC. This is in line with Estati et al., who also validated BRCAmut status to significantly promote complete macroscopic resection in recurrence.32 The rate of complete secondary resection in their study was 89.5% in the BRCAmut group and 65.2% in the BRCAwt group.32 This indicates that especially patients with BRCAmut rOC disease show altered tumor biology and consecutively treatment response that cannot just be explained by younger age. Therefore, we suggest that BRCA mutation status should be taken into account as a parameter when selecting patients eligible for secondary debulking surgery aiming for complete macroscopic resection.
Surgery in patients with first rOC disease has been proven to significantly prolong PFS and OS in the DESKTOP III trial only if macroscopic tumor clearance could be achieved.3 If there was still residual tumor mass left, patients showed worse survival compared with those treated with chemotherapy alone. Two further prospective randomized clinical trials confirmed better PFS rates in patients with rOC disease if complete macroscopic tumor resection could be achieved, but the GOG trial failed to show a significant OS benefit in patients from the surgery cohort.33,34 One crucial difference between the GOG trial and the DESKTOP III and SOC-1 trials is the lack of a scoring system to select patients who will more likely benefit from secondary tumor debulking. These findings underline that reliable criteria to assess eligibility of individual patients for surgical treatment are indispensable. Implementation of the AGO criteria into this decision-making process has already been proven to be a very helpful tool in clinical practice, although only complete resection rates of 67–75.5% of patients with rOC and AGO positive score were reported in recent studies.3,4 Conversely, complete macroscopic resection was still achievable in 48.5% patients with an AGO negative score.4 Hence, identifying new selection criteria for secondary tumor debulking is mandatory, especially in borderline decision cases to identify those patients in whom maximal rOC surgery is feasible without harming those patients who would not benefit from it. In this context, we suggest implementing BRCAmut status as a favorable factor for surgical therapy in patients with rOC disease. To our understanding, the combination of effective cytoreductive surgery with chemotherapy followed by effective maintenance therapy such as PARP inhibitors can be a key factor to achieve prolonged survival in a larger cohort of patients with BRCAmut OC disease. The superiority of this treatment combination has already been proven in a recent study by Marchetti et al.35 Additional factors, such as further homologous recombination deficiencies, need to be investigated in future studies to estimate predictive value for complete macroscopic tumor resection during primary and recurrent OC.
In our study cohort, we confirmed BRCAmut status to be a predictive factor for patient survival. Although patients with BRCAmut disease showed longer PFS at all times, a significant difference could only be measured during recurrence. Additionally, patients with BRCAmut disease showed a median OS benefit of 24.3 months compared with the BRCAwt group. These findings are partially in line with the clinical trial conducted by Bookman et al., which investigated the impact of platinum-free interval and BRCA mutation status on treatment and survival of patients with rOC. One major finding was that patients with BRCAmut disease showed a prolonged OS without reaching statistical significance.23 However, it has to be stated that, in the mentioned study, median follow-up was 25 months and, therefore, the observation period was possibly not long enough to detect long-term effects of BRCA mutation status on survival. In our study, median follow-up after first-line treatment was considerably longer, at 51.7 months, and effects of BRCA positivity on OS were significant. Another trial by Jorge et al. had a similar median follow-up of 49.3 months and compared survival of patients with BRCA1 and BRCA2 mutated OC disease treated with surgery and platinum-based chemotherapy. They calculated a median OS of 76.2 months from diagnosis for patients with positive BRCA1 and 82.0 months for patients with positive BRCA2 disease, which is in line with our finding of 80.6 months for the BRCAmut cohort.24
Strengths and Limitations
The current study has some strengths and limitations. Its strengths included the multicenter trial design, which allowed gathering a large, demographically heterogeneous study cohort. Moreover, this is the first trial to focus on surgical outcome and survival of patients with BRCAmut disease from pOC through several courses of recurrence. Limitations include the retrospective nature of our investigation, as well as the fact that none of the BRCAmut patients incorporated into this study had received PARP inhibitors in their maintenance therapy regimens. Lastly, the fact that 27.4% of our study cohort were yet untested for BRCA mutations at the end of follow-up needs to be mentioned as a limitation. However, we deliberately decided to incorporate these patients into the BRCAwt cohort since our main intention was to identify effects of BRCAmut status. Therefore, it can be assumed that our findings definitely do not overestimate the real effect of BRCA mutations, since a small number of unexamined patients could also be carriers of the mutation yet were included in the negative group.
Conclusions
Our study shows that patients with BRCAmut disease benefit from surgical treatment, especially in rOC, suggesting the inclusion of BRCA mutation status information in the decision-making process in case of recurrence. We will prospectively evaluate these findings in ENGOT-ov47-TR /NOGGO-AGO TR2/HELPER, a study that enrolls 500 patients with first relapsed ovarian cancer who are going to receive surgery followed by systemic treatment, versus systemic treatment alone on the basis of physician choice.
References
Sehouli J, Grabowski JP. Surgery for recurrent ovarian cancer: options and limits. Best Pract Res Clin Obstet Gynaecol. 2017;41:88–95.
Capozzi VA, Rosati A, Turco LC, Sozzi G, Riccò M, Chiofalo B, et al. Surgery vs chemotherapy for ovarian cancer recurrence: what is the best treatment option. Gland Surg. 2020;9(4):1112–7.
Harter P, Sehouli J, Vergote I, Ferron G, Reuss A, Meier W, Greggi S, Mosgaard BJ, Selle F, Guyon F, Pomel C, Lécuru F, Zang R, Avall-Lundqvist E, Kim JW, Ponce J, Raspagliesi F, Kristensen G, Classe JM, Hillemanns P, Jensen P, Hasenburg A, Ghaem-Maghami S, Mirza MR, Lund B, Reinthaller A, Santaballa A, Olaitan A, Hilpert F, du Bois A; DESKTOP III Investigators. Randomized trial of cytoreductive surgery for relapsed ovarian cancer. N Engl J Med. 2 Dec 2021;385(23):2123–2131. https://doi.org/10.1056/NEJMoa2103294. Erratum in: N Engl J Med. 17 Feb 2022;386(7):704.
Muallem MZ, Gasimli K, Richter R, Almuheimid J, Nasser S, Braicu EI, et al. AGO score as a predictor of surgical outcome at secondary cytoreduction in patients with ovarian cancer. Anticancer Res. 2015;35(6):3423–9.
Harter P, du Bois A, Hahmann M, Hasenburg A, Burges A, Loibl S, et al. Surgery in recurrent ovarian cancer: the Arbeitsgemeinschaft Gynaekologische Onkologie (AGO) DESKTOP OVAR trial. Ann Surg Oncol. 2006;13(12):1702–10.
Harter P, Sehouli J, Reuss A, Hasenburg A, Scambia G, Cibula D, et al. Prospective validation study of a predictive score for operability of recurrent ovarian cancer: the Multicenter Intergroup Study DESKTOP II. A project of the AGO Kommission OVAR, AGO Study Group, NOGGO, AGO-Austria, and MITO. Int J Gynecol Cancer. 2011;21(2):289–95.
Janco JM, Kumar A, Weaver AL, McGree ME, Cliby WA. Performance of AGO score for secondary cytoreduction in a high-volume U.S. center. Gynecol Oncol. 2016;141(1):140–7.
Harter P, Beutel B, Alesina PF, Lorenz D, Boergers A, Heitz F, et al. Prognostic and predictive value of the Arbeitsgemeinschaft Gynaekologische Onkologie (AGO) score in surgery for recurrent ovarian cancer. Gynecol Oncol. 2014;132(3):537–41.
Bogani G, Tagliabue E, Signorelli M, Ditto A, Martinelli F, Chiappa V, et al. A score system for complete cytoreduction in selected recurrent ovarian cancer patients undergoing secondary cytoreductive surgery: predictors- and nomogram-based analyses. J Gynecol Oncol. 2018;29(3):e40.
Sehouli J, Richter R, Braicu EI, Buhling KJ, Bahra M, Neuhaus P, et al. Role of secondary cytoreductive surgery in ovarian cancer relapse: who will benefit? A systematic analysis of 240 consecutive patients. J Surg Oncol. 2010;102(6):656–62.
Knabben L, Imboden S, Mueller MD. Genetic testing in ovarian cancer—clinical impact and current practices. Horm Mol Biol Clin Investig. 2019;41(3).
Mirza MR, Coleman RL, González-Martín A, Moore KN, Colombo N, Ray-Coquard I, et al. The forefront of ovarian cancer therapy: update on PARP inhibitors. Ann Oncol. 2020;31(9):1148–59.
Moore K, Colombo N, Scambia G, Kim B-G, Oaknin A, Friedlander M, et al. Maintenance Olaparib in patients with newly diagnosed advanced ovarian cancer. New Eng J Med. 2018;379(26):2495–505.
Bickell NA, Egorova N, Prasad-Hayes M, Franco R, Howell EA, Wisnivesky J, et al. Secondary surgery versus chemotherapy for recurrent ovarian cancer. Am J Clin Oncol. 2018;41(5):458–64.
Ray-Coquard I, Pautier P, Pignata S, Pérol D, González-Martín A, Berger R, et al. Olaparib plus bevacizumab as first-line maintenance in ovarian cancer. New Eng J Med. 2019;381(25):2416–28.
Gadducci A, Guarneri V, Peccatori FA, Ronzino G, Scandurra G, Zamagni C, et al. Current strategies for the targeted treatment of high-grade serous epithelial ovarian cancer and relevance of BRCA mutational status. J Ovarian Res. 2019;12(1):9.
Marchetti C, Minucci A, Pietragalla A, Scambia G, Fagotti A. BRCA status assessment in epithelial ovarian cancer and the challenge of tumor testing. Int J Gynecol Cancer. 2020;30(9):1465–6.
Giudice MT, D’Indinosante M, Cappuccio S, Gallotta V, Fagotti A, Scambia G, et al. Secondary cytoreduction in ovarian cancer: who really benefits? Arch Gynecol Obstet. 2018;298(5):873–9.
Kurman RJ, International Agency for Research on Cancer., World Health Organization. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: IARC Sci Publ; 2014. 307 p.p.
Sehouli J, Konsgen D, Mustea A, Oskay-Ozcelik G, Katsares I, Weidemann H, et al. “IMO”–intraoperative mapping of ovarian cancer. Zentralbl Gynakol. 2003;125(3–4):129–35.
Aletti GD, Santillan A, Eisenhauer EL, Hu J, Aletti G, Podratz KC, et al. A new frontier for quality of care in gynecologic oncology surgery: Multi-institutional assessment of short-term outcomes for ovarian cancer using a risk-adjusted model. J Gynecol Oncol. 2007;107(1):99–106.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Bookman MA, Tyczynski JE, Espirito JL, Wilson TW, Fernandes AW. Impact of primary platinum-free interval and BRCA1/2 mutation status on treatment and survival in patients with recurrent ovarian cancer. Gynecol Oncol. 2017;146(1):58–63.
Jorge S, Swisher EM, Norquist BM, Pennington KP, Gray HJ, Urban RR, et al. Patterns and duration of primary and recurrent treatment in ovarian cancer patients with germline BRCA mutations. Gynecol Oncol Rep. 2019;29:113–7.
Marchetti C, De Leo R, Musella A, D’Indinosante M, Capoluongo E, Minucci A, et al. BRCA mutation status to personalize management of recurrent ovarian cancer: a multicenter study. Ann Surg Oncol. 2018;25(12):3701–8.
Ataseven B, Tripon D, Schwameis R, et al. Clinical outcome in patients with primary epithelial ovarian cancer and germline BRCA 1/2-mutation—real life data. Gynecol Oncol. 2021;163(3):569–77.
Ben David Y, Chetrit A, Hirsh-Yechezkel G, Friedman E, Beck BD, Beller U, et al. Effect of BRCA mutations on the length of survival in epithelial ovarian tumors. J Clin Oncol. 2002;20(2):463–6.
Kubelac P, Vlad C, Berindan Neagoe I, Irimie A, Achimas Cadariu P. The clinical features associated with mutated BRCA1 and 2 genes in ovarian cancer patients. JBUON. 2019;24(4):1538–43.
Xu K, Yang S, Zhao Y. Prognostic significance of BRCA mutations in ovarian cancer: an updated systematic review with meta-analysis. Oncotarget. 2017;8(1):285–302.
Ashour M, Ezzat Shafik H. Frequency of germline mutations in BRCA1 and BRCA2 in ovarian cancer patients and their effect on treatment outcome. Cancer Manag Res. 2019;11:6275–84.
Hyman DM, Long KC, Tanner EJ, Grisham RN, Arnold AG, Bhatia J, et al. Outcomes of primary surgical cytoreduction in patients with BRCA-associated high-grade serous ovarian carcinoma. Gynecol Oncol. 2012;126(2):224–8.
Estati FL, Pirolli R, de Alencar VTL, Ribeiro ARG, Formiga MN, Torrezan GT, et al. Impact of BRCA1/2 mutations on the efficacy of secondary cytoreductive surgery. Ann Surg Oncol. 2020;28:3637–45.
Shi T, Zhu J, Feng Y, et al. Secondary cytoreduction followed by chemotherapy versus chemotherapy alone in platinum-sensitive relapsed ovarian cancer (SOC-1): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22(4):439–49.
Coleman RL, Brady MF, Herzog TJ, et al. Bevacizumab and paclitaxel-carboplatin chemotherapy and secondary cytoreduction in recurrent, platinum-sensitive ovarian cancer (NRG Oncology/Gynecologic Oncology Group study GOG-0213): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2017;18(6):779–91.
Marchetti C, Rosati A, Scaletta G, Pietragalla A, Arcieri M, Ergasti R, et al. Secondary cytoreductive surgery in platinum-sensitive recurrent ovarian cancer before olaparib maintenance: Still getting any benefit? A case-control study. Gynecol Oncol. 2019;155(3):400–5.
Acknowledgement
E.I.B. is a Feodor Lynen fellow of the Humboldt Foundation and a participant of the Charité Clinical Scientist Program funded by the Charité Universitätsmedizin Berlin and the Berlin Institute of Health. This work was supported by European Commission’s Seventh Framework Programme under grant agreement no. 279113 (OCTIPS; www.octips.eu).
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by European Commission’s Seventh Framework Programme under Grant Agreement No. 279113 (OCTIPS; www.octips.eu).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
F.T. received grants, research support, advisory boards, honoraria, and travel expenses from AstraZeneca, Clovis, GSK, Medac, MSD, PharmaMar, Roche, and Tesaro. C.G. received personal fees from Roche, AstraZeneca, MSD, GSK, Tesaro, Nucana, Clovis, Foundation One, Chugai, Sierra Oncology, Cor2Ed, and Takeda; and research funding from AstraZeneca, Novartis, Aprea, Nucana, GSK, Tesaro, BerGen Bio, and Medannexin. O.D. served on advisory boards for Clovis Oncology, IMV, Tesaro, and Merck; and on the speaker bureau for AstraZeneca and Tesaro. J.S. received grants and personal fees from Astra Zeneca, Bayer, Eisai, Clovis, Olympus, Johnson and Johnson, PharmaMar, Pfizer, TEVA, Tesaro/GSK, MSD, Lilly, Roche, and Merck. E.I.B. received research funding from Bayer, Roche Diagnostics, Tesaro, GSK, snd AstraZeneca; and personal fees from AstraZeneca, Clovis, GSK, Tesaro, EISAI, RochePharma, and Roche Diagnostics. All remaining authors have declared no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Glajzer, J., Castillo-Tong, D.C., Richter, R. et al. Impact of BRCA Mutation Status on Tumor Dissemination Pattern, Surgical Outcome and Patient Survival in Primary and Recurrent High-Grade Serous Ovarian Cancer: A Multicenter Retrospective Study by the Ovarian Cancer Therapy-Innovative Models Prolong Survival (OCTIPS) Consortium. Ann Surg Oncol 30, 35–45 (2023). https://doi.org/10.1245/s10434-022-12459-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12459-3