Abstract
Background
Objective measures of post-pancreatectomy weight change for pancreatic ductal adenocarcinoma (PDAC) have not been extensively studied for long-term outcomes. We used weight measurements in our institutional medical record to analyze trends in post-pancreatectomy weight and determine the association with disease status.
Methods
Pancreatectomies for PDAC (n = 315) and benign indications (n = 111) were identified. Preoperative baseline, minimum postoperative (Min #1), and subsequent postoperative maximum (Max) weights were abstracted. Multivariable Cox hazards regression was conducted to analyze the association between weight change and survival.
Results
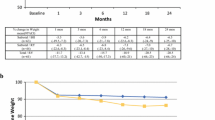
Median weight loss postoperatively in each group was > 20 lbs. PDAC patients gained 10 lbs after Min #1 compared to 15 lbs in the benign cohort (p < 0.001). Few patients returned to their preoperative weight (29.8% PDAC vs. 40.5% benign, p = 0.04). Patients with early PDAC recurrence (< 13 months) lost more weight (18.0% vs. 13.3% vs. 10.9%, p < 0.001) and gained less weight (2.1% vs. 12.0% vs. 7.9%, p < 0.001) compared with those with late cancer recurrence (≥ 13 months) or no evidence of active disease, respectively. PDAC patients lost 11.2 lbs in the year preceding recurrence diagnosis. Weight loss was not associated with survival; however, weight gain was associated with improved survival.
Conclusions
Resections for PDAC are complicated by a similar degree of weight loss as patients with benign disease, and there is no association with survival. However, failure to gain weight is especially ominous. Weight loss after weight recovery foreshadows disease recurrence. These data suggest that rigorous weight tracking is an untapped surveillance strategy in patients with PDAC.


Similar content being viewed by others
References
Hezel AF, Kimmelman AC, Stanger BZ, Bardeesy N, DePinho RA. Genetics and biology of pancreatic ductal adenocarcinoma. Genes Dev. 2006;20(10):1218–49. https://doi.org/10.1101/gad.1415606.
Lee JC, Ahn S, Cho IK, Lee J, Kim J, Hwang JH. Management of recurrent pancreatic cancer after surgical resection: a protocol for systematic review, evidence mapping and meta-analysis. BMJ Open. 2018;8:e017249. https://doi.org/10.1136/bmjopen-2017-017249.
Oettle H, Neuhaus P, Hochhaus A, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310:1473–81. https://doi.org/10.1001/jama.2013.279201.
Tian X, Li J, Gao H, et al. Prognostic factors for disease-free survival in patients with pancreatic ductal adenocarcinoma after surgery: a single center experience. J Pancreatol. 2019;2(1):22–7.
Moletta L, Serafini S, Valmasoni M, Pierobon ES, Ponzoni A, Sperti C. Surgery for recurrent pancreatic cancer: is it effective? Cancers. 2019;11(7):991. https://doi.org/10.3390/cancers11070991.
Groot VP, Rezaee N, Wu W, et al. Patterns, timing, and predictors of recurrence following pancreatectomy for pancreatic ductal adenocarcinoma. Ann Surg. 2018;267(5):936–45. https://doi.org/10.1097/SLA.0000000000002234.
Iacobuzio-Donahue CA, Fu B, Yachida S, et al. DPC4 gene status of the primary carcinoma correlates with patterns of failure in patients with pancreatic cancer. J Clin Oncol. 2009;27(11):1806–13. https://doi.org/10.1200/JCO.2008.17.7188.
Schnelldorfer T, Ware AL, Sarr MG, et al. Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma is cure possible? Ann Surg. 2008;247(3):456–62. https://doi.org/10.1097/SLA.0b013e3181613142.
Seelig MH, Janot M, Chromik AM, et al. Redo-surgery following curative resection of pancreatic carcinoma: The difference between true and suspected recurrence. Digest Surg. 2009;26(3):222–8. https://doi.org/10.1159/000219332.
Paniccia A, Hosokawa P, Henderson W, et al. Characteristics of 10-year survivors of pancreatic ductal adenocarcinoma. JAMA Surg. 2015;150(8):701–10. https://doi.org/10.1001/jamasurg.2015.0668.
Azizian A, Rühlmann F, Krause T, et al. CA19-9 for detecting recurrence of pancreatic cancer. Sci Rep. 2020;10:1332. https://doi.org/10.1038/s41598-020-57930-x.
Humphris JL, Chang DK, Johns AL, et al. The prognostic and predictive value of serum CA19.9 in pancreatic cancer. Ann Oncol. 2012;23(7):1713–22. https://doi.org/10.1093/annonc/mdr561.
Winter JM, Tang LH, Klimstra DS, et al. A novel survival-based tissue microarray of pancreatic cancer validates MUC1 and mesothelin as biomarkers. PLoS ONE. 2012;7(7):e40157. https://doi.org/10.1371/journal.pone.0040157.
Hashimoto D, Chikamoto A, Ohmuraya M, et al. Impact of postoperative weight loss on survival after resection for pancreatic cancer. J Parenteral Enteral Nutr. 2015;39(5):598–603. https://doi.org/10.1177/0148607114520992.
Morita Y, Sakaguchi T, Kitajima R, et al. Body weight loss after surgery affects the continuity of adjuvant chemotherapy for pancreatic cancer. BMC Cancer. 2019;19:416. https://doi.org/10.1186/s12885-019-5621-5.
Trudeau MT, Casciani F, Gershuni VM, et al. Defining postoperative weight change after pancreatectomy: Factors associated with distinct and dynamic weight trajectories. Surgery. 2020;168(6):1041–7. https://doi.org/10.1016/j.surg.2020.07.056.
National Comprehensive Cancer Network Clinical Practice Guidelines in Clinical Oncology: Pancreatic Adenocarcinoma. Version 1.2020. 2019.
Sheffield KM, Crowell KT, Lin YL, Djukom C, Goodwin JS, Riall TS. Surveillance of pancreatic cancer patients after surgical resection. Ann Surg Oncol. 2012;19(5):1670–7. https://doi.org/10.1245/s10434-011-2152-y.
Tempero MA, Uchida E, Takasaki H, Burnett DA, Steplewski Z, Pour PM. Relationship of carbohydrate antigen 19–9 and Lewis antigens in pancreatic cancer. Cancer Res. 1987;47(20):5501–3.
Hue JJ, Sugumar K, Kyasaram RK, et al. Weight loss as an untapped early detection marker in pancreatic and periampullary cancer. Ann Surg Oncol. 2021. https://doi.org/10.1245/s10434-021-09861-8.
Wente MN, Bassi C, Dervenis C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142(5):761–8. https://doi.org/10.1016/j.surg.2007.05.005.
Bassi C, Marchegiani G, Dervenis C, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery (United States). 2017;161(3):584–91. https://doi.org/10.1016/j.surg.2016.11.014.
Hue JJ, Markt SC, Rao G, Winter JM. Patient-centered weight tracking as an early cancer detection strategy. J Cancer Prev. 2020;25(3):1–8. https://doi.org/10.15430/JCP.2020.25.3.181.
Hendifar AE, Petzel MQB, Zimmers TA, et al. Pancreas cancer-associated weight loss. Oncologist. 2019;24(5):691–701. https://doi.org/10.1634/theoncologist.2018-0266.
Yuan C, Babic A, Khalaf N, et al. Diabetes, weight change, and pancreatic cancer risk. JAMA Oncol. 2020;6(10):e202948. https://doi.org/10.1001/jamaoncol.2020.2948.
Hue JJ, Markt SC, Sugumar K, et al. Weight loss during neoadjuvant therapy for pancreatic cancer does not predict poor outcomes. Am J Surg. 2021. https://doi.org/10.1016/j.amjsurg.2021.10.001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare no potential conflicts of interest
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hue, J.J., Ocuin, L.M., Kyasaram, R.K. et al. Weight Tracking as a Novel Prognostic Marker After Pancreatectomy. Ann Surg Oncol 29, 3450–3459 (2022). https://doi.org/10.1245/s10434-022-11325-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11325-6