Abstract
Background
Despite awareness regarding financial toxicity in breast cancer care, little is known about the financial strain associated with breast reconstruction. This study aims to describe financial toxicity and identify factors independently associated with financial toxicity for women pursuing post-mastectomy breast reconstruction.
Methods
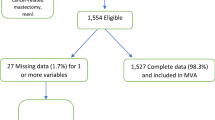
A 33-item electronic survey was distributed to members of the Love Research Army. Women over 18 years of age and at least 1 year after post-mastectomy breast reconstruction were invited to participate. The primary outcome of interest was self-reported financial toxicity due to breast reconstruction, while secondary outcomes of interest were patient-reported out-of-pocket expenses and impact of financial toxicity on surgical decision making.
Results
In total, 922 women were included (mean age 58.6 years, standard deviation 10.3 years); 216 women (23.8%) reported financial toxicity from reconstruction. These women had significantly greater out-of-pocket medical expenses. When compared with women who did not experience financial toxicity, those who did were more likely to have debt due to reconstruction (50.9% vs. 3.2%, p < 0.001). Younger age, lower annual household income, greater out-of-pocket expenses, and a postoperative major complication were independently associated with an increased risk for financial toxicity. If faced with the same decision, women experiencing financial toxicity were more likely to decide against reconstruction (p < 0.001) compared with women not experiencing financial toxicity.
Conclusions
Nearly one in four women experienced financial toxicity from breast reconstruction. Women who reported higher levels of financial toxicity were more likely to change their decisions about surgery. Identified factors predictive of financial toxicity could guide preoperative discussions to inform decision making that mitigates undesired financial decline.

Similar content being viewed by others
References
Keisler-Starkey K, Bunch LN. Health insurance coverage in the United States: 2019. 2020. Available at: https://www.census.gov/content/dam/Census/library/publications/2020/demo/p60-271.pdf. Accessed 28 May 2021.
Definitions of health insurance terms. Available at: https://www.bls.gov/ncs/ebs/sp/healthterms.pdf. Accessed 27 May 2021.
Women’s Health and Cancer Rights Act (WHCRA). The center for consumer information and insurance oversight. 2020. Available at: https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/whcra_factsheet. Accessed 21 Aug 2020.
Levit KR, Cowan CA. The burden of health care costs: business, households, and governments. Health Care Financ Rev. 1990;12(2):127–37.
Cowan CA, McDonnell PA, Levit KR, Zezza MA. Burden of health care costs: businesses, households, and governments, 1987–2000. Health Care Financ Rev. 2002;23(3):131–59.
Emanuel EJ, Glickman A, Johnson D. Measuring the burden of health care costs on US families: the affordability index. JAMA. 2017;318(19):1863–4.
Billig JI, Lan WC, Chung KC, Kuo CF, Sears ED. The increasing financial burden of outpatient elective surgery for the privately insured. Ann Surg. 2020;272(3):530–6.
Desai A, Gyawali B. Financial toxicity of cancer treatment: moving the discussion from acknowledgement of the problem to identifying solutions. EClinicalMedicine. 2020;20:100269.
Zafar SY, Abernethy AP. Financial toxicity, part I: a new name for a growing problem. Oncology (Williston Park). 2013;27(2):80–1.
Witte J, Mehlis K, Surmann B, et al. Methods for measuring financial toxicity after cancer diagnosis and treatment: a systematic review and its implications. Ann Oncol. 2019;30(7):1061–70.
Jagsi R, Pottow JA, Griffith KA, et al. Long-term financial burden of breast cancer: experiences of a diverse cohort of survivors identified through population-based registries. J Clin Oncol. 2014;32(12):1269–76.
Resnicow K, Patel MR, McLeod MC, Katz SJ, Jagsi R. Physician attitudes about cost consciousness for breast cancer treatment: differences by cancer sub-specialty. Breast Cancer Res Treat. 2019;173(1):31–6.
Jagsi R, Ward KC, Abrahamse PH, et al. Unmet need for clinician engagement regarding financial toxicity after diagnosis of breast cancer. Cancer. 2018;124(18):3668–76.
Offodile AC, Asaad M, Boukovalas S, et al. Financial toxicity following surgical treatment for breast cancer: a cross-sectional pilot study. Ann Surg Oncol. 2020;28(5):2451–62.
Panchal H, Matros E. Current trends in postmastectomy breast reconstruction. Plast Reconstr Surg. 2017;140(5S Advances in Breast Reconstruction):7S-13S.
Albornoz C, Bach P, Mehrara B, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131(1):15–23.
Dr Susan Love Foundation. About the love research army. Available at: https://www.loveresearcharmy.org/about-love-research-army. Accessed 1 Sep 2020.
Greenup RA, Rushing C, Fish L, et al. Financial costs and burden related to decisions for breast cancer surgery. J Oncol Pract. 2019;15(8):e666–76.
Yan C, Fischer JP, Wes AM, et al. The cost of major complications associated with immediate two-stage expander/implant-based breast reconstruction. J Plast Surg Hand Surg. 2015;49(3):166–71.
Wilkins EG, Hamill JB, Kim HM, et al. Complications in postmastectomy breast reconstruction: One-year outcomes of the mastectomy reconstruction outcomes consortium (MROC) study. Ann Surg. 2018;267(1):164–70.
Berlin NL, Chung KC, Matros E, Chen JS, Momoh AO. The Costs of breast reconstruction and implications for episode-based bundled payment models. Plast Reconstr Surg. 2020;146(6):721e–30e.
Smith BD, Jiang J, Shih YC, et al. Cost and complications of local therapies for early-stage breast cancer. J Natl Cancer Inst. 2017;109(1):djw178.
Atisha DM, Rushing CN, Samsa GP, et al. A national snapshot of satisfaction with breast cancer procedures. Ann Surg Oncol. 2015;22(2):361–9.
Acknowledgments
The authors would like to thank the members of the Love Research Army who volunteered their time to complete our survey and who contributed financial information regarding their cancer care.
Funding
The University of Michigan Section of Plastic Surgery MacNguyen Fund was used to support collaboration with the Susan Love Research Foundation Love Research Army.
Author information
Authors and Affiliations
Contributions
Nishant Ganesh Kumar and Nicholas L. Berlin contributed equally as co-first authors. Adeyiza O. Momoh is the senior/last author. All authors and co-authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship.
Corresponding author
Ethics declarations
Disclosures
Nishant Ganesh Kumar, Nicholas L. Berlin, Sarah T. Hawley, Reshma Jagsi, and Adeyiza O. Momoh report no financial conflicts of interests or relevant disclosures in relation to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ganesh Kumar, N., Berlin, N.L., Hawley, S.T. et al. Financial Toxicity in Breast Reconstruction: A National Survey of Women Who have Undergone Breast Reconstruction After Mastectomy. Ann Surg Oncol 29, 535–544 (2022). https://doi.org/10.1245/s10434-021-10708-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10708-5