Abstract
Background
A margin of “no ink on tumor” has been established for primary breast conservation therapy (BCT), but the appropriate margin following neoadjuvant chemotherapy (NAC) remains controversial. We examined the impact of margin width on ipsilateral breast tumor recurrence (IBTR) in the NAC-BCT population.
Methods
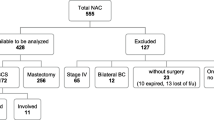
Consecutive patients receiving NAC-BCT were identified from a prospective database. The associations between clinicopathologic characteristics, margin width, and isolated IBTR were evaluated.
Results
From 2013 to 2019 we identified 582 patients with 586 tumors who received NAC-BCT. The median age of the cohort was 54 years (IQR 45, 62); 84% of patients had cT1/T2 tumors and 61% were clinically node positive. The majority of tumors were HER2+ (38%) or triple negative (TN) (31%). Pathologic complete response was observed in 29%. Margin width was > 2 mm in 517 tumors (88%) and ≤ 2 mm in 69 (12%). At a median follow-up of 39 months, 14 patients had IBTR as a first event, with 64% occurring within 24 months of surgery. The 4-year IBTR rate was 2% (95% CI 1–4%), and there was no difference based on margin width (3% ≤ 2 mm vs 2% > 2 mm; p = not significant). On univariate analysis, clinical and pathologic T stage and receptor subtype, but not margin width, were associated with IBTR (p < 0.05). On multivariable analysis, TN subtype and higher pathologic T stage were associated with isolated IBTR (both p < 0.05).
Conclusion
Pathologic features and tumor biology, not margin width, were associated with IBTR in NAC-BCT patients.

Similar content being viewed by others
References
King TA, Morrow M. Surgical issues in patients with breast cancer receiving neoadjuvant chemotherapy. Nat Rev Clin Oncol. 2015;12:335–43.
Boughey JC, McCall LM, Ballman KV, et al. Tumor Biology Correlates with Rates of Breast-Conserving Surgery and Pathologic Complete Response After Neoadjuvant Chemotherapy for Breast Cancer. Ann Surg. 2014;260:608–16.
Mamtani A, Barrio AV, King TA, et al. How Often Does Neoadjuvant Chemotherapy Avoid Axillary Dissection in Patients with Histologically Confirmed Nodal Metastases? Results of a Prospective Study. Ann Surg Oncol. 2016;23:3467–74.
Boughey JC, Peintinger F, Meric-Bernstam F, et al. Impact of Preoperative Versus Postoperative Chemotherapy on the Extent and Number of Surgical Procedures in Patients Treated in Randomized Clinical Trials for Breast Cancer. Ann Surg. 2006;244:464–70.
Golshan M, Cirrincione CT, Sikov WM, et al. Impact of Neoadjuvant Chemotherapy in Stage II-III Triple Negative Breast Cancer on Eligibility for Breast-Conserving Surgery and Breast Conservation Rates. Ann Surg. 2015;262:434–9.
Golshan M, Cirrincione CT, Sikov WM, et al. Impact of neoadjuvant chemotherapy on eligibility for and frequency of breast conservation in stage II-III Her2-positive breast cancer: surgical results of CALGB 40601 (Alliance). Breast Cancer Res Treat. 2016;160:297–304.
Petruolo O, Sevilimedu V, Montagna G, Le T, Morrow M, Barrio AV. How Often Does Modern Neoadjuvant Chemotherapy Downstage Patients to Breast-Conserving Surgery? Ann Surg Oncol. 2021;28(1):287–94.
Fisher B, Brown A, Mamounas E, et al. Effect of Preoperative Chemotherapy on Local-Regional Disease in Women with Operable Breast Cancer: Findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997;15:2483–93.
Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol. 2018;19:27–39.
Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology-American Society for Radiation Oncology Consensus Guideline on Margins for Breast-Conserving Surgery with Whole-Breast Irradiation in Stage I and II Invasive Breast Cancer. J Clin Oncol. 2014;32:1507–1515.
Mukhtar RA, Yau C, Rosen M, et al. Clinically Meaningful Tumor Reduction Rates Vary by Prechemotherapy MRI Phenotype and Tumor Subtype in the I-SPY 1 TRIAL (CALGB 150007/150012; ACRIN 6657). Ann Surg Oncol. 2013;20:3823–3830.
Bossuyt V, Provenzano E, Symmans WF, et al. Recommendations for standardized pathological characterization of residual disease for neoadjuvant clinical trials of breast cancer by the BIG-NABCG collaboration. Annals of Oncology. 2015;26:1280–91.
Chen MA, Meric-Bernstan F, Hunt KK, et al. Breast Conservation After Neoadjuvant Chemotherapy: the MD Anderson Cancer Center Experience. J Clin Oncol. 2004;22:2303–12.
Choi J, Laws A, Hu J, Barry W, Golshan M, King T. Margins in Breast-Conserving Surgery After Neoadjuvant Therapy. Ann Surg Oncol. 2018;25:3541–7.
Lin J, Lin KJ, Wang YF, Huang LH, Chen SLI, Chen DR. Association of surgical margins with local recurrence in patients undergoing breast-conserving surgery after neoadjuvant chemotherapy. BMC Cancer. 2020;20:451.
Wimmer K, Bollinger M, Bago-Horvath Z, et al. Impact of Surgical Margins in Breast Cancer After Preoperative Systemic Chemotherapy on Local Recurrence and Survival. Ann Surg Oncol. 2020;27:1700–7.
Rouzier R, Extra JM, Carton M, et al. Primary Chemotherapy for Operable Breast Cancer: Incidence and Prognostic Significance of Ipsilateral Breast Tumor Recurrence After Breast-Conserving Surgery. J Clin Oncol. 2001;19:3828–35.
Gray RJ. A Class of K-Sample Tests for Comparing Cumulative Incidence of a Competing Risk. Ann Statist. 1988;16(3):1141–54.
Mamounas EP, Anderson SJ, Dignam JJ, et al. Predictors of Locoregional Recurrence After Neoadjuvant Chemotherapy: Results from Combined Analysis of National Surgical Adjuvant Breast and Bowel Project B-18 and B-27. J Clin Oncol. 2012;30:3960–6.
Aebi S, Gelber S, Anderson SJ, et al. Chemotherapy for isolated locoregional recurrence of breast cancer (CALOR): a randomized trial. Lancet Oncol. 2014;15:156–63.
Caudle AS, Yu TK, Tucker SL, et al. Local-regional control according to markers of breast cancer subtypes and response to neoadjuvant chemotherapy in breast cancer patients undergoing breast conserving therapy. Breast Cancer Research. 2012;14:R83.
Jwa E, Shin KH, Kim JY, et al. Locoregional Recurrence by Tumor Biology in Breast Cancer Patients after Preoperative Chemotherapy and Breast Conservation Treatment. Cancer Res Treat. 2016;48:1363–72.
Marinovich ML, Noguchi N, Morrow M, Houssami N. Changes in Reoperation After Publication of Consensus Guidelines on Margins for Breast-Conserving Surgery: A Systematic Review and Meta-analysis. JAMA Surg. 2020;155(10):e203025.
Morrow M, Abrahamse P, Hofer TP, et al. Trends in Reoperation After Initial Lumpectomy for Breast Cancer Addressing Overtreatment in Surgical Management. JAMA Oncology. 2017;3:1352–7.
Bhutiani N, Mercer MK, Bachmann KC, et al. Evaluating the Effect of Margin Consensus Guideline Publication on Operative Patterns and Financial Impact of Breast Cancer Operation. JACS. 2018;227:6–11.
Havel L, Naik H, Ramirez L, Morrow M, Landercasper J. Impact of the SSO-ASTRO Margin Guideline on Rates of Re-excision After Lumpectomy for Breast Cancer: A Meta-Analysis. Ann Surg Oncol. 2019;26:1238–44.
Dahlback C, Manjer J, Rehn M, Ringberg A. Determinants of patient satisfaction regarding aesthetic outcome and skin sensitivity after breast-conserving surgery. World Journal of Surgical Oncology. 2016;14:303.
Pogoda K, Niwinska A, Murawska M, Pienkowski T. Analysis of pattern, time and risk factors influencing recurrence in triple-negative breast cancer patients. Medical Oncology. 2013;30:388.
Van Maaren MC, de Munck L, Strobbe LJA, et al. Ten-year recurrence rates for breast cancer subtypes in the Netherlands: a large population-based study. Int J Cancer. 2019;144:263–72.
Acknowledgment
This research was funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Monica Morrow has received speaking honoraria from Exact Sciences and Roche. The remaining authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was presented as an oral presentation at the SSO 2021.
Rights and permissions
About this article
Cite this article
Mrdutt, M., Heerdt, A., Sevilimedu, V. et al. Margin Width and Local Recurrence in Patients Undergoing Breast Conservation After Neoadjuvant Chemotherapy. Ann Surg Oncol 29, 484–492 (2022). https://doi.org/10.1245/s10434-021-10533-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10533-w